Practice Essentials
Brain abscess is a focal area of necrosis with a surrounding membrane within the brain parenchyma, usually resulting from an infectious process or, rarely, from a traumatic process. [1] The introduction of infectious agents results in various responses from the central nervous system (CNS). In the earliest stage of purulent bacterial brain infection, the generalized initial reaction is cerebritis. Within the background of cellular response to the infection, cerebritis evolves into a localized abscess in a predictable series of stages. Neuroimaging of these stages reflects the underlying pathophysiology of abscess formation. Variations in the brain's reaction at different locations and similarities in the brain's reaction to certain agents and in the appearances of aggressive neoplasms all require correlation of medical history, neuroimaging, and results of microbiologic analysis.
Brain abscess is a potentially fatal injury that must be treated promptly to avoid complications that require neurosurgery, such as intraventricular rupture. Patients with brain abscess may exhibit a variety of nonspecific symptoms, simulating the presence of neurologic disease such as ischemic stroke or an intracranial tumor mass. Early radiologic diagnosis with adequate subsequent treatment improves the patient's chances of recovery. Magnetic resonance imaging (MRI) with diffusion-weighted images and apparent diffusion coefficient maps have made it possible to diagnose an intraventricular rupture of the abscess and consequently to provide appropriate neurosurgical treatment. [2]
Brain abscess may result from a traumatic brain injury, neurosurgical procedures, contiguous spread from a local source, or hematogenous spread of a systemic infection. [3, 4, 5] Immunosuppressed patients, especially those patients who have received an organ transplant, are susceptible to the development of cerebral infections. [6] Pyogenic infection of brain parenchyma begins with cerebritis, a localized area of inflammation, which can progress to an immature capsular stage and then to brain abscess, which is characterized by an area of parenchymal infection that contains pus encapsulated by a vascularized membrane. Clinical symptoms of brain abscess include focal neurologic deficits and increased intracranial pressure. [7, 8, 9, 10, 11] Brain abscesses may also present as nonspecific findings that are suggestive of other conditions. [12] Cranial nerve involvement may present a confusing clinical pattern. [13]
With the advent of antimicrobials and imaging studies such as computed tomography (CT) scanning and MRI, mortality has been reduced. Rupture of a brain abscess, however, is more fatal. Long-term neurologic sequelae after infection are dependent on early diagnosis and administration of antibiotics. [1, 14, 15]
Imaging modalities
In the earliest stages of the evolution of a cerebral abscess, a CT scan of the brain may be negative or it may show subtle nonspecific findings. MRI of the brain performed without and with a gadolinium contrast agent is the more sensitive test. The enhancement seen on MRI following intravenous contrast is relatively more sensitive and somewhat more specific than CT. [7, 10, 11, 16, 17, 18, 19, 20, 21]
The preferred initial examination of the patient in whom brain abscess is suspected is MRI with and without gadolinium enhancement. Similar diagnostic results can be expected from cranial CT scans without and with the intravenous administration of iodinated contrast medium. Both imaging techniques help detect the mass effect of the abscess; however, findings on MRI with a diffusion protocol are more specific in differentiating cerebral tumor, stroke, and abscess. In particular, examination of the metabolite peaks with MR spectroscopy can help to specifically differentiate tumor, radiation necrosis, and abscess by identifying their different spectral profiles. [7, 10, 11, 16, 17, 21, 22, 23, 24]
In the early stage of cerebritis, noncontrast CT may show localized hypoattenuation, and contrast enhancement is variable but, if present, may show a nodular or ringlike pattern. When a capsule forms, a round or ovoid area of hypoattenuation will be seen with ring enhancement that dissipates on delayed images. [7]
On MRI, early cerebritis is characterized as poorly defined hyperintensity on T2-weighted images and as hypointensity on T1-weighted images. With progressing infection, T1-weighted images will show localized fluid collection as hyperintense compared to CSF and hypointense relative to white matter. On T2-weighted images, fluid collections appear as isointense to hyperintense. [7] Diffusion-weighted images may aid in the diagnosis by displaying the central nonenhancing portion of an abscess as hyperintense on diffusion-weighted images and as hypointense on apparent diffusion coefficient maps. [7, 8]
Perfusion MRI has also been used to differentiate these lesions by evaluating vascularity with blood flow analysis with dynamic intravenous gadolinium contrast injection studies.
Occasionally, distinguishing brain abscess from neoplasm or postoperative changes from infection is difficult. In these patients, a nuclear agent can be used to tag white blood cells or antibodies to help differentiation.
In a study by Chiang et al, diffusion, perfusion-weighted, and spectroscopic MRIs were able to differentiate cerebral abscesses from necrotic tumors. The authors found that the mean apparent diffusion coefficient value at the central cavities of the cerebral abscesses were significantly lower; the mean relative cerebral blood volume values of the necrotic tumor walls were significantly higher; and amino acids were present only in the cerebral abscesses. [25]
Sepahdari et al found that in 9 cases of orbital cellulitis, including 6 cases of pyogenic abscess, diffusion-weighted imaging confirmed abscess in a majority of cases without contrast-enhanced imaging. According to the authors, this may be of particular importance in patients in whom the use of contrast is contraindicated. Diffusion-weighted imaging improved diagnostic confidence in virtually all the patients with orbital abscess when it was used along with contrast-enhanced imaging. [26]
Transcranial color-coded duplex ultrasonography is a valuable monitoring tool used in the intensive care unit after neurosurgical procedures, providing information in B-mode, color, and pulsed-wave Doppler modes. [27]
Early and improved diagnostic imaging techniques have allowed the discovery of brain abscess at a much earlier stage.
(See the images below.)
 Brain abscess. Axial CT scan in a patient who presented with a headache, fever, and a history of a recent pneumonia demonstrates a poorly defined area of posterior parietal brain edema (arrows). Early cerebritis may not outline a focal mass clearly.
Brain abscess. Axial CT scan in a patient who presented with a headache, fever, and a history of a recent pneumonia demonstrates a poorly defined area of posterior parietal brain edema (arrows). Early cerebritis may not outline a focal mass clearly.
 Brain abscess. Axial nonenhanced cranial CT scan in a patient who presented with fever, headache, and a previous paranasal sinus infection demonstrates a poorly defined pattern of mass effect and low attenuation in the left temporal lobe. The pattern is consistent with possible early cerebritis; however, glioma and infarct may have similar presentations.
Brain abscess. Axial nonenhanced cranial CT scan in a patient who presented with fever, headache, and a previous paranasal sinus infection demonstrates a poorly defined pattern of mass effect and low attenuation in the left temporal lobe. The pattern is consistent with possible early cerebritis; however, glioma and infarct may have similar presentations.
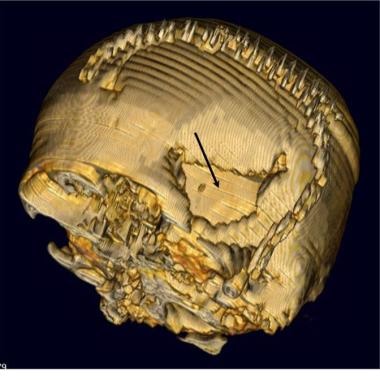 Brain abscess. Three-dimensional surface model of a cranial CT scan in a patient with a postcraniotomy abscess. The large deformity in the skull indicates the route of abscess spread.
Brain abscess. Three-dimensional surface model of a cranial CT scan in a patient with a postcraniotomy abscess. The large deformity in the skull indicates the route of abscess spread.
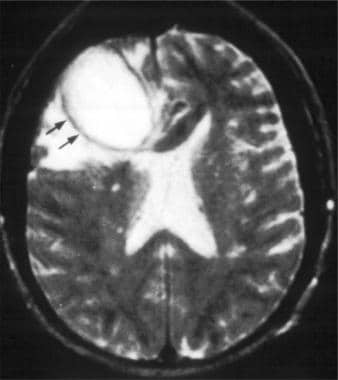 Brain abscess. Axial T2-weighted MRI in a patient with a right frontal abscess. Note the mass effect and surrounding edema. The wall of the abscess is relatively thin (black arrows).
Brain abscess. Axial T2-weighted MRI in a patient with a right frontal abscess. Note the mass effect and surrounding edema. The wall of the abscess is relatively thin (black arrows).
Pathophysiology
Brain abscesses may occur as a result of direct skull trauma or following surgery. The spread of infection from the paranasal sinuses, from the middle ear and the mastoid air cells, from a tooth abscess, or by hematogenous spread from the lungs or heart are other potential infectious mechanisms.
Rhinosinusitis-induced brain abscesses are rare but can result in devastating long-term sequalae and mortality; they require a high index of suspicion with early imaging to start early empiric parenteral antibiotic treatment covering aerobes and anaerobes. [28]
Brain infection and bacteremia are common clinical manifestations of listeriosis. [29]
(See the images below.)
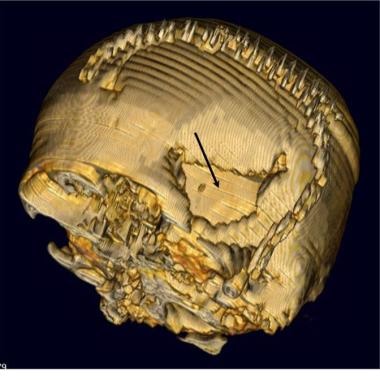 Brain abscess. Three-dimensional surface model of a cranial CT scan in a patient with a postcraniotomy abscess. The large deformity in the skull indicates the route of abscess spread.
Brain abscess. Three-dimensional surface model of a cranial CT scan in a patient with a postcraniotomy abscess. The large deformity in the skull indicates the route of abscess spread.
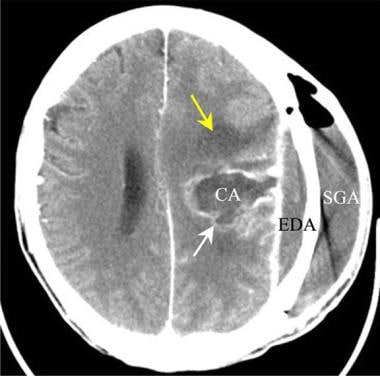 Brain abscess. Axial contrast-enhanced CT scan in a patient who was treated surgically for a depressed skull fracture. The left parietal cranial injury has become complicated by an abscess of the subgaleal space (SGA), of the epidural space (EDA), and within the left cerebral hemisphere (CA). Edema related to the abscess is indicated by the yellow arrow. The cerebral abscess wall enhances (white arrow).
Brain abscess. Axial contrast-enhanced CT scan in a patient who was treated surgically for a depressed skull fracture. The left parietal cranial injury has become complicated by an abscess of the subgaleal space (SGA), of the epidural space (EDA), and within the left cerebral hemisphere (CA). Edema related to the abscess is indicated by the yellow arrow. The cerebral abscess wall enhances (white arrow).
 Brain abscess. Anterior view of a chest radiograph in a patient with thick-walled right lung abscess. The patient later developed a brain abscess.
Brain abscess. Anterior view of a chest radiograph in a patient with thick-walled right lung abscess. The patient later developed a brain abscess.
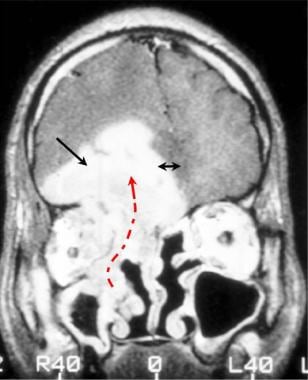 Brain abscess. Gadolinium-enhanced coronal T1-weighted MRI in a patient who presented with headache, fever, and diplopia. The right frontal lobe of the brain is shifted across the midline (double arrow) by an intracranial abscess (single black arrow) that has extended upward from the medial right orbit and medial ethmoid air cells (curved dotted arrow). Aspergillus organisms were recovered from the sinuses and brain tissue.
Brain abscess. Gadolinium-enhanced coronal T1-weighted MRI in a patient who presented with headache, fever, and diplopia. The right frontal lobe of the brain is shifted across the midline (double arrow) by an intracranial abscess (single black arrow) that has extended upward from the medial right orbit and medial ethmoid air cells (curved dotted arrow). Aspergillus organisms were recovered from the sinuses and brain tissue.
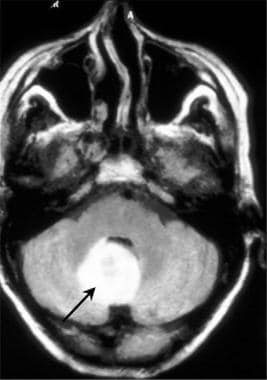 Brain abscess. Axial fluid-attenuated inversion recovery (FLAIR) MRI in a patient with Nocardia-related abscess of the cerebellar vermis (black arrow).
Brain abscess. Axial fluid-attenuated inversion recovery (FLAIR) MRI in a patient with Nocardia-related abscess of the cerebellar vermis (black arrow).
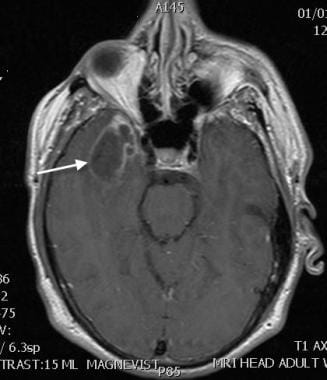 Cerebral abscess. This T1 contrast-enhanced MRI of a right temporal abscess demonstrates an irregular mass with moderate peripheral enhancement. This image was obtained early in the clinical course. The etiology of the brain abscess was an abscessed tooth.
Cerebral abscess. This T1 contrast-enhanced MRI of a right temporal abscess demonstrates an irregular mass with moderate peripheral enhancement. This image was obtained early in the clinical course. The etiology of the brain abscess was an abscessed tooth.
Differentials
The differential diagnosis includes the following:
Limitations of techniques
Plain radiographs of the paranasal sinuses can only suggest a possible etiology for cerebral abscess. Early findings of CT examinations are not specific for cerebral abscess. The edema pattern and moderate mass effect cannot be differentiated from tumor or stroke in some patients. MRI findings in patients with cerebritis may resemble findings in stroke, while findings in the infarcts that result from vasculitis and cerebritis may resemble those of embolic strokes. Nuclear medicine single photon emission CT (SPECT) findings are not specific for brain abscess unless a white cell tag is used.
Follow-up scans for certain infectious agents, such as Mycobacterium tuberculosis, may be necessary because infection by these organisms may not follow a predictable response to treatment. Tuberculosis-related brain abscesses that retain positive results to culture and smears following 4 weeks of treatment may not represent treatment failure. In addition, treatment of fungal infections may require many weeks of treatment with interval follow-up imaging studies. Follow-up imaging during the treatment for toxoplasmosis is important in avoiding brain biopsy.
Intervention
Intervention in patients with cerebral abscess is most commonly limited to biopsy and aspiration of infectious material that may represent the origin of a CNS infection. Aspiration and biopsy of small lesions is best performed by using a CT-guided computer-assisted technique or with the aid of an external frame, which (with the aid of CT data) directs the placement of the aspiration needle. Fully computer-aided virtual imaging programs have provided greater flexibility in the application of both CT and MRI sets during craniotomy procedures and in the aspiration of selected lesions. Intraoperative ultrasonography may aid in the detection and treatment of relatively large superficial abscess collections. [30]
Radiography
Radiographic findings are usually limited to paranasal or mastoid sinus opacification; however, gas bubbles or air-fluid levels within the cranium may indicate a gas-producing organism or a communication with the paranasal sinuses or the nose.
Direct evidence of osteomyelitis of the skull is generally a mixed pattern of lucency with a destruction of the outer or inner tables of the skull.
Occasionally, foreign bodies (eg, in gunshot wounds) or osteomyelitis of the maxillary bone may indicate a probable source for an intracranial abscess. Bone destruction of the roof, floor, or lateral wall of the sinuses may indicate an aggressive osteomyelitis with extension into the intracranial space.
Degree of confidence
Clouding of the sinuses is not a direct indication of an intracranial abscess, merely a possible etiology. Air-fluid levels within the cranial vault strongly suggest abscess formation.
Patients with established intracranial abscesses may develop fluid retention within the mastoid and paranasal sinuses secondary to endotracheal intubation and chronic disability. Most patients with osteomyelitis of the mandible or maxilla do not develop intracranial abscesses.
Computed Tomography
Because CT scanners are commonly available for the evaluation of critically ill patients, cerebral infections will most likely be first identified on a CT scan of the brain. The clinical symptoms of an early brain abscess may be nonspecific. On nonenhanced CT, Toxoplasma encephalitis appears as areas of isointense or hypodense mass effect. The basal ganglia and the corticomedullary junction are most commonly affected. Contrast-enhanced CT demonstrates a ring or nodular enhancement pattern with lesions of 1-3 cm in diameter. The enhancement is greatest within the intermediate zone, where inflammation is the greatest.
(See the images below.)
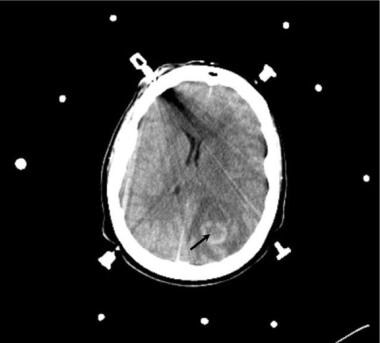
 Brain abscess. Axial CT scan with intravenous (IV) contrast enhancement in a patient who presented with headache and fever. Initial CT scan demonstrated mass effect and edema within the left temporal lobe. Since the edema and mass pattern were poorly defined, a biopsy of the left temporal lobe was performed to exclude a tumor. Following resection of the temporal lobe abscess, extracranial, subdural, and intracerebral abscesses developed (arrows).
Brain abscess. Axial CT scan with intravenous (IV) contrast enhancement in a patient who presented with headache and fever. Initial CT scan demonstrated mass effect and edema within the left temporal lobe. Since the edema and mass pattern were poorly defined, a biopsy of the left temporal lobe was performed to exclude a tumor. Following resection of the temporal lobe abscess, extracranial, subdural, and intracerebral abscesses developed (arrows).
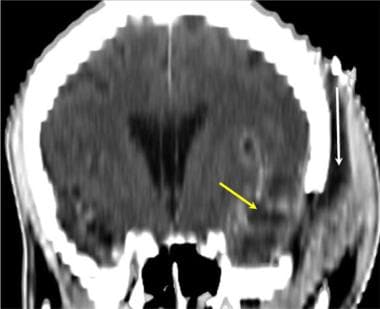 Brain abscess. Coronal multiplanar reformatted CT scan in a patient who developed temporal brain abscesses (yellow arrows) and a left-sided extracranial abscess (white arrow) following surgery of the left temporal skull.
Brain abscess. Coronal multiplanar reformatted CT scan in a patient who developed temporal brain abscesses (yellow arrows) and a left-sided extracranial abscess (white arrow) following surgery of the left temporal skull.
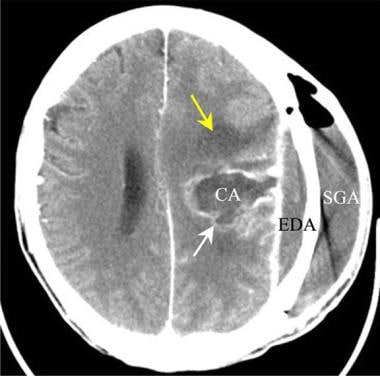 Brain abscess. Axial contrast-enhanced CT scan in a patient who was treated surgically for a depressed skull fracture. The left parietal cranial injury has become complicated by an abscess of the subgaleal space (SGA), of the epidural space (EDA), and within the left cerebral hemisphere (CA). Edema related to the abscess is indicated by the yellow arrow. The cerebral abscess wall enhances (white arrow).
Brain abscess. Axial contrast-enhanced CT scan in a patient who was treated surgically for a depressed skull fracture. The left parietal cranial injury has become complicated by an abscess of the subgaleal space (SGA), of the epidural space (EDA), and within the left cerebral hemisphere (CA). Edema related to the abscess is indicated by the yellow arrow. The cerebral abscess wall enhances (white arrow).
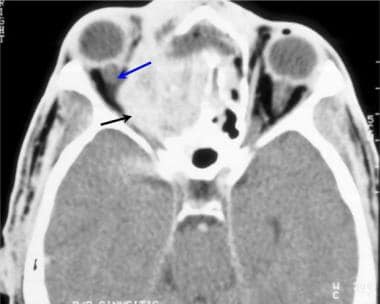 Brain abscess. Axial CT scan with intravenous (IV) contrast enhancement in a patient with fever and diplopia demonstrates an enhancing mass arising from within the ethmoid air cells, with expansion into the medial right orbit (black arrow). The optic nerve is in contact with the mass (blue arrow).
Brain abscess. Axial CT scan with intravenous (IV) contrast enhancement in a patient with fever and diplopia demonstrates an enhancing mass arising from within the ethmoid air cells, with expansion into the medial right orbit (black arrow). The optic nerve is in contact with the mass (blue arrow).
CT manifestations of an intracranial abscess depend on the stage of the abscess formation. The earliest phase may be related to meningitis, with no findings on unenhanced CT studies. Enhancement of the meningeal surfaces is a nonspecific and inconsistent finding in patients with meningitis. [7, 31]
Brain abscess passes through 4 stages: early cerebritis, late cerebritis, early capsule, and late capsule. [32]
During early cerebritis, nonenhanced CT scans may demonstrate normal findings or may show only poorly marginated subcortical hypodense areas. Contrast-enhanced CT studies demonstrate an ill-defined contrast-enhancing area within the edematous region.
During the early stage of a formed abscess, the lesion coalesces, with an irregular enhancing rim that surrounds a central low-attenuating area.
Scans obtained with a time delay following contrast enhancement in cerebritis may show contrast "filling in" the central low-attenuating region. A formed abscess will not "fill in" the central portion of the abscess.
Peripheral edema results in considerable mass effect with sulcal obliteration.
The early capsule stage is characterized by a distinct collagenous capsule, while a relatively thin, well-delineated capsule marks the final stage of a fully formed abscess.
Ring-enhancing lesions are commonly seen in various disease conditions. In addition to being seen in abscesses, a ringlike enhancement pattern also is seen in metastatic brain tumors, some primary brain tumors (particularly grade 4 astrocytomas), granulomas, resolving hematomas, and infarctions. The cystic pattern is a particularly prominent feature of cysticercosis, because of the infestation of the larva of Taenia solium. In most pyogenic abscesses, the ring is smooth and thin walled (< 5 mm). The medial margin is often thinner along the medial margin, which may reflect the variation of cerebral perfusion of gray and white matter. The wall of a cystic neoplasm is generally thick and irregular, frondlike, or lobulated. [7, 31]
(See the images below.)
 Brain abscess. Axial CT scan obtained with intravenous (IV) contrast enhancement in a patient with fever and headaches. Because a definite diagnosis of abscess is difficult to determine in some patients in whom ring enhancement is not associated with an apparent source of infection, stereotactic biopsy and culture of a walled abscess may be necessary.
Brain abscess. Axial CT scan obtained with intravenous (IV) contrast enhancement in a patient with fever and headaches. Because a definite diagnosis of abscess is difficult to determine in some patients in whom ring enhancement is not associated with an apparent source of infection, stereotactic biopsy and culture of a walled abscess may be necessary.
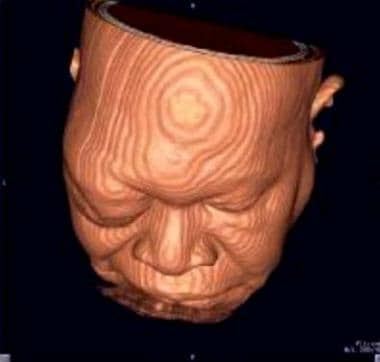 Brain abscess. Surface 3-dimensional model of a craniofacial CT scan in a patient with headache, orbital swelling, and diplopia of 48 hours' duration. Note the remarkable degree of right orbital swelling, which has resulted in the right lid being closed.
Brain abscess. Surface 3-dimensional model of a craniofacial CT scan in a patient with headache, orbital swelling, and diplopia of 48 hours' duration. Note the remarkable degree of right orbital swelling, which has resulted in the right lid being closed.
Degree of confidence
The moderate vasogenic edema that is seen in the early stages of cerebritis and abscess formation must be interpreted in the context of the clinical presentation. The presence of fever, known infection, and immunosuppression supports the probable diagnosis of early abscess formation; however, cerebrovascular accidents (CVAs) and tumors must be included in the differential diagnosis. Later, the well-formed abscess wall must be inspected within the context of other known malignancies, which may be a source for cerebral metastatic disease, glioma, lymphoma, and multiple sclerosis.
False positives/negatives
False-negative CT scans may occur if intravenous contrast enhancement is not adequate or if imaging of the brain is performed too soon after contrast administration, which can happen easily when a rapid CT (eg, multisection) scanner is used.
False-positive results primarily are the result of mistaking alternative causes of ringlike lesions of the brain for an abscess. Ring-enhancing lesions must be placed into the differential diagnosis, which includes some primary brain tumors (eg, anaplastic astrocytoma), metastatic brain tumors, abscess, granuloma, resolving hematoma, brain infarct, thrombosed vascular malformation, demyelinating disease (eg, multiple sclerosis), thrombosed aneurysm, and other primary brain tumors, particularly primary CNS lymphoma in patients with AIDS.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is the imaging modality of choice for diagnosis and follow-up of lesions. It is more sensitive than other modalities for early cerebritis and satellite lesions, particularly those present in the brainstem, as well as for estimating necrosis and extent of the lesion. It enables greater contrast between cerebral edema and the brain and is more sensitive for detecting the spread of inflammation into ventricles and the subarachnoid space. [1]
The findings of a brain abscess on noncontrast CT are somewhat nonspecific. Most commonly, mass effect with surrounding edema is found (see the image below). On MRI, early cerebritis is characterized as poorly defined hyperintensity on T2-weighted images and as hypointensity on T1-weighted images. With progressing infection, T1-weighted images will show localized fluid collection as hyperintense, compared to CSF, and hypointense relative to white matter. On T2-weighted images, fluid collections appear as isointense to hyperintense. [7] Diffusion-weighted images may aid in the diagnosis by displaying the central nonenhancing portion of an abscess as hyperintense on diffusion-weighted images and as hypointense on apparent diffusion coefficient maps. [7, 8]
Perfusion MRI has also been used to differentiate these lesions by evaluating vascularity with blood flow analysis with dynamic intravenous gadolinium contrast injection studies. MRI of the brain offers a better opportunity to differentiate a brain abscess from other causes of a cerebral mass. [16, 17] Occasionally, distinguishing brain abscess from neoplasm or postoperative changes from infection is difficult. In such cases, a nuclear agent can be used to tag white blood cells or antibodies to assist in differentiation.
 Brain abscess. A large left frontal low-density mass. The patient presented with headache and a low-grade fever. The abscess was drained. The abscess contained many white blood cells; however, no culture growth was noted. A diagnosis of an anaerobic gram-positive cocci was made on the basis of histological studies.
Brain abscess. A large left frontal low-density mass. The patient presented with headache and a low-grade fever. The abscess was drained. The abscess contained many white blood cells; however, no culture growth was noted. A diagnosis of an anaerobic gram-positive cocci was made on the basis of histological studies.
The use of intravenous contrast helps define the wall of the abscess and improves the differentiation of a brain abscess from cerebral contusion or infarcts. Many brain neoplasms have a similar enhancement pattern and may be difficult to differentiate from a brain abscess. [33]
(See the image below.)
 Brain abscess. Sagittal contrast-enhanced T1 MRI. The patient presented with headache and a low-grade fever. The abscess was drained. The abscess contained many white blood cells; however, no culture growth was noted. A diagnosis of an anaerobic gram-positive cocci was made on the basis of histological studies. MRI of the brain demonstrates mass effect and a ring enhancement in this case of a left frontal abscess.
Brain abscess. Sagittal contrast-enhanced T1 MRI. The patient presented with headache and a low-grade fever. The abscess was drained. The abscess contained many white blood cells; however, no culture growth was noted. A diagnosis of an anaerobic gram-positive cocci was made on the basis of histological studies. MRI of the brain demonstrates mass effect and a ring enhancement in this case of a left frontal abscess.
Abscesses that conform to the common cerebrospinal fluid spaces can be differentiated by the characteristics of diffusion restriction and marginal contrast enhancement on MRI. (See the images below.)
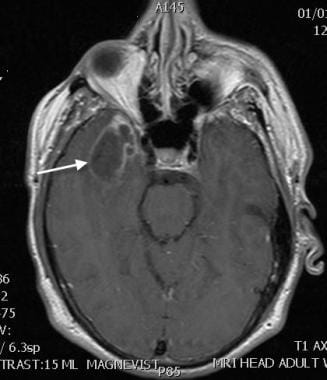 Cerebral abscess. This T1 contrast-enhanced MRI of a right temporal abscess demonstrates an irregular mass with moderate peripheral enhancement. This image was obtained early in the clinical course. The etiology of the brain abscess was an abscessed tooth.
Cerebral abscess. This T1 contrast-enhanced MRI of a right temporal abscess demonstrates an irregular mass with moderate peripheral enhancement. This image was obtained early in the clinical course. The etiology of the brain abscess was an abscessed tooth.
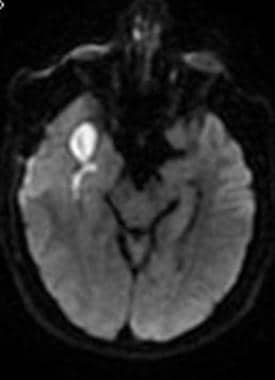 Cerebral abscess. Diffusion-weighted MRI demonstrates increased signal brightness within the abscess of the right temporal fossa.
Cerebral abscess. Diffusion-weighted MRI demonstrates increased signal brightness within the abscess of the right temporal fossa.
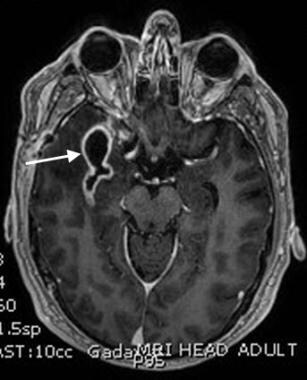 MRI of right temporal lobe abscess. This T1 contrast-enhanced image demonstrates many of the characteristics of a typical brain abscess. Note the thick wall, which demonstrates significant enhancement following the administration of gadolinium-based contrast.
MRI of right temporal lobe abscess. This T1 contrast-enhanced image demonstrates many of the characteristics of a typical brain abscess. Note the thick wall, which demonstrates significant enhancement following the administration of gadolinium-based contrast.
MRI of the brain without and with intravenous gadolinium contrast enhancement is the most sensitive test for Toxoplasma encephalitis. Lesions with contrast may be hyperintense compared to normal brain tissue and may be difficult to identify compared to the edema pattern otherwise seen in the surrounding brain. The ring enhancement, which is best seen on T1-weighted gadolinium-enhanced studies, represents the enhancement within the most active area of the infection. Following treatment with pyrimethamine and sulfadiazine or clindamycin, the lesions become reduced in size with resolution of the ring of enhancement. (See the images below.)
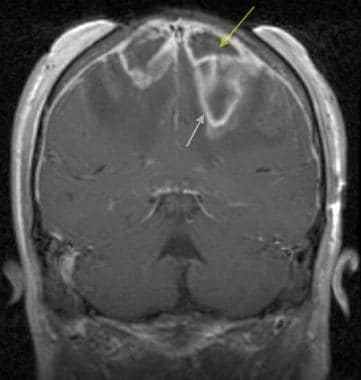 Brain abscess. Coronal T1-weighted post–gadolinium-enhanced MRI of the brain in a patient with fever following head trauma. Osteomyelitis of the skull developed in this patient following cranial trauma. Bilateral subdural abscesses (yellow arrow) developed by direct extension of the infection beyond the skull. The leading edge of the cerebritis is marked by the pattern of enhancement within the deeper margins of the left parietal lobe (white arrow).
Brain abscess. Coronal T1-weighted post–gadolinium-enhanced MRI of the brain in a patient with fever following head trauma. Osteomyelitis of the skull developed in this patient following cranial trauma. Bilateral subdural abscesses (yellow arrow) developed by direct extension of the infection beyond the skull. The leading edge of the cerebritis is marked by the pattern of enhancement within the deeper margins of the left parietal lobe (white arrow).
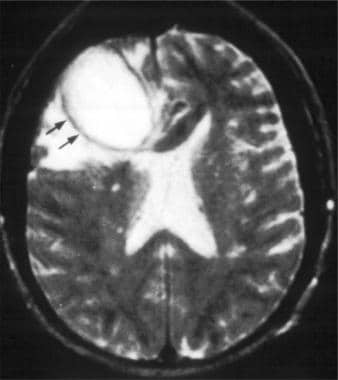 Brain abscess. Axial T2-weighted MRI in a patient with a right frontal abscess. Note the mass effect and surrounding edema. The wall of the abscess is relatively thin (black arrows).
Brain abscess. Axial T2-weighted MRI in a patient with a right frontal abscess. Note the mass effect and surrounding edema. The wall of the abscess is relatively thin (black arrows).
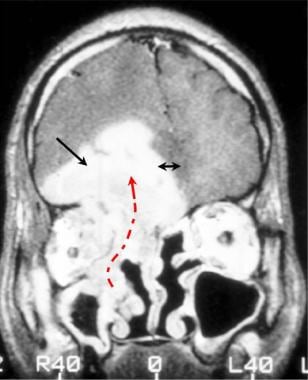 Brain abscess. Gadolinium-enhanced coronal T1-weighted MRI in a patient who presented with headache, fever, and diplopia. The right frontal lobe of the brain is shifted across the midline (double arrow) by an intracranial abscess (single black arrow) that has extended upward from the medial right orbit and medial ethmoid air cells (curved dotted arrow). Aspergillus organisms were recovered from the sinuses and brain tissue.
Brain abscess. Gadolinium-enhanced coronal T1-weighted MRI in a patient who presented with headache, fever, and diplopia. The right frontal lobe of the brain is shifted across the midline (double arrow) by an intracranial abscess (single black arrow) that has extended upward from the medial right orbit and medial ethmoid air cells (curved dotted arrow). Aspergillus organisms were recovered from the sinuses and brain tissue.
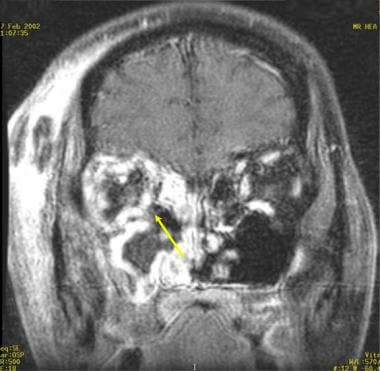 Brain abscess. Coronal T1-weighted gadolinium-enhanced MRI in a patient with sudden onset of diplopia, fever, and right orbital swelling. Note the enhancement within the right ethmoid sinuses from which the infection arose. The medial superior right maxillary sinus has been destroyed (yellow arrow).
Brain abscess. Coronal T1-weighted gadolinium-enhanced MRI in a patient with sudden onset of diplopia, fever, and right orbital swelling. Note the enhancement within the right ethmoid sinuses from which the infection arose. The medial superior right maxillary sinus has been destroyed (yellow arrow).
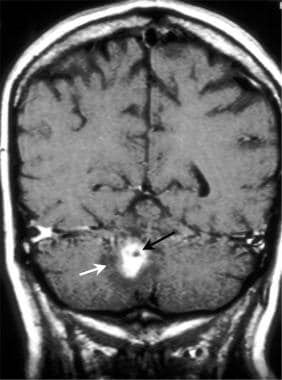 Brain abscess. Coronal T1-weighted spin-echo gadolinium-enhanced MRI demonstrates a central zone of enhancement within the abscess, with a zone of decreased brightness (edema, white arrow). Nocardia organisms were cultured from within the abscess cavity.
Brain abscess. Coronal T1-weighted spin-echo gadolinium-enhanced MRI demonstrates a central zone of enhancement within the abscess, with a zone of decreased brightness (edema, white arrow). Nocardia organisms were cultured from within the abscess cavity.
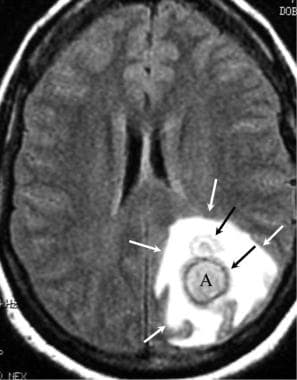 Brain abscess. Axial fluid-attenuated inversion recovery (FLAIR) MRI of a left occipital-parietal brain abscess. The edema pattern (white arrows) surrounds the central abscess (A). A secondary (daughter) abscess is noted anterior to the primary abscess cavity.
Brain abscess. Axial fluid-attenuated inversion recovery (FLAIR) MRI of a left occipital-parietal brain abscess. The edema pattern (white arrows) surrounds the central abscess (A). A secondary (daughter) abscess is noted anterior to the primary abscess cavity.
MRI findings of brain abscess vary with time. [18, 19, 34, 35, 36, 37, 38]
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Early cerebritis stage
The early cerebritis stage presents as an ill-defined subcortical hyperintense zone that can be noted on T2-weighted imaging.
Lesions appearing hyperintense on diffusion-weighted imaging with apparent-diffusion-coefficient (ADC) values less than 0.9 are most commonly brain abscess, whereas hypointense lesions on diffusion-weighted imaging with ADC values greater than 2 are more likely nonabscess cystic lesions.
Contrast-enhanced T1-weighted studies demonstrate poorly delineated enhancing areas within the isointense to mildly hypointense edematous region.
Late cerebritis stage
During the late cerebritis stage, the central necrotic area is hyperintense to brain tissue on proton-density and T2-weighted sequences.
The thick, somewhat irregularly marginated rim appears isointense to mildly hyperintense on spin-echo T1-weighted images and isointense to relatively hypointense on proton-density and T2-weighted scans.
Peripheral edema is common. The rim enhances intensely following contrast administration. Satellite lesions may be demonstrated.
Early and late capsule stages
During the early and late capsule stages, the collagenous abscess capsule is visible prior to contrast as a comparatively thin-walled, isointense to slightly hyperintense ring that becomes hypointense on T2-weighted MRIs.
Diffusion-weighted imaging aids in depiction of specific features of a brain abscess. If a cerebral abscess ruptures into the ventricular system, diffusion-weighted images demonstrate specific patterns.
Purulent material within the ventricle appears similar to that of the central abscess cavity, with a strongly hyperintense signal on diffusion-weighted images.
Magnetic resonance spectroscopy
MR spectroscopy may be helpful in the differential diagnosis of toxoplasmosis versus CNS lymphoma. CNS lymphoma generally shows a mild pattern of elevated lipid and lactate peaks, with a prominent choline peak with some other normal metabolites. In toxoplasmosis, there are elevated lipid and lactate peaks, while other normal brain metabolites are nearly absent.
Diffusion-weighted MRI
Diffusion-weighted MRI may be useful in differentiating abscess from necrotic tumor. Diffusion-weighted echo planar images demonstrate an abscess as a high signal intensity with a corresponding reduction in the apparent diffusion coefficient. The brightness on diffusion-weighted imaging (DWI) is related to the cellularity and viscosity of the contents within the abscess cavity. Tumors with central necrosis have marked hypointensity on diffusion-weighted images and much higher apparent diffusion coefficient values. The pattern described above for an abscess has also been noted for acute cerebral infarction.
Diffusion-tensor imaging
This imaging approach is based on 3-dimensional diffusivity and is commonly used for evaluation of white matter tracts. Fractional anisotropy, a quantitative variable, is calculated by diffusion-tensor imaging. This variable reflects the degree of tissue organization and is quite higher in abscess, supposedly due to organized leukocytes in the abscess cavity. [1]
Degree of confidence
In patients with ring-enhancing cerebral mass lesions, restricted diffusion is characteristic but not pathognomonic for abscess. Low apparent diffusion coefficient values also may be found in brain metastases. Diffusion imaging techniques should be corrected for T2 brightness contribution. Corrected diffusion maps more accurately reflect the relative diffusion within a large or complex lesion. Diffusion imaging is more sensitive than conventional MRI alone in detection of changes due to infections and ischemic lesions.
Single-voxel proton MR spectroscopy is useful in differentiating ringlike enhanced lesions that cannot be diagnosed correctly using enhanced MRI alone. MR spectroscopy can help to specifically differentiate tumor, radiation necrosis, or abscess by identifying their different spectral profiles. Perfusion MRI has also been used to differentiate these lesions by evaluating their degree of vascularity through dynamic blood flow analysis studies.
Diffusion MRI does not help in differentiating brain abscess formation from focal brain infarcts related to venous thrombosis, although superior imaging of the anatomic distribution of lesions proves useful. Restricted diffusion within ring enhancement is not pathognomonic for brain abscess.
Ultrasonography
On ultrasonograms, cerebral abscess is depicted as a complex cystic pattern with an echogenic wall and an ultrasonographically hypoechoic or mildly hyperechoic central zone of necrosis. Cerebral ultrasonography is rarely used in the evaluation of cerebral abscess in the adult, except for intraoperative guidance for aspiration procedures, because the intact skull is a barrier to the procedure.
In the neonate, abscess can be diagnosed by ultrasonographic images obtained through the anterior fontanelle. [39] Brain ultrasonograms can reveal the size and number of abscesses but provide only a limited suggestion of a possible origin for the infection. Ultrasonography-guided aspiration of brain abscesses through a single burr hole has been performed with excellent overall results.
Ultrasonography cannot help differentiate a cystic neoplasm from an abscess. When seen in the neonate, periventricular and arachnoid cysts are not commonly abscesses.
Porencephalic cysts may suggest thin-walled abscesses if communication with the ventricle is not depicted clearly. Arachnoid cysts have thin walls with a marked, hypoechoic pattern.
Nuclear Imaging
Brain SPECT imaging by using thallous chloride Tl 201 (thallium-201; 201Tl) can help detect and differentiate infectious processes from lymphoma and other primary brain neoplasms. Brain abscess may be evaluated using gallium Ga 67 (gallium-67; 67Ga) citrate and technetium-99mm hexamethylpropyleneamine oxime (HMPAO)–labeled leukocytes. In patients with an active abscess, nuclear agents collect in the wall of the abscess. Similar findings occur within high-grade brain tumors (glioma). Differential considerations of rounded (ring) lesions of the brain include some primary brain tumors (eg, anaplastic astrocytoma), metastatic brain tumors, abscess, granuloma, resolving hematoma, brain infarct, thrombosed vascular malformation, demyelinating disease, thrombosed aneurysm, and primary CNS lymphoma in patients with AIDS.
Degree of confidence
Tl-201 brain SPECT imaging appears to be unreliable for differentiating primary lymphoma from nonmalignant brain lesions in patients with AIDS. Follow-up scans showing improvement may help further differentiate the lesions, but brain biopsy is necessary to establish a definitive diagnosis in questionable cases.
False-positive 201Tl SPECT imaging in brain abscess may indicate focally increased intracranial 201Tl uptake; however, such activity may be an abscess if positive tumor activity is reported. Single lesions demonstrated on MRI scans with focal accumulation of 201Tl strongly suggest lymphoma. Multiple lesions demonstrated on MRIs with 201Tl SPECT uptake ratios of 2.9 or more also suggest lymphoma; however, uptake ratios less than 2.1 do not aid in discrimination.
Differentiation of toxoplasmosis abscess from primary brain lymphoma requires a difficult combination of clinical history, laboratory findings, and radiographic considerations. A trial period of treatment against the toxoplasmosis organism with follow-up imaging is necessary in some patients before excluding the possibility of CNS lymphoma.
Angiography
Cerebral angiography is rarely performed to define an abscess; however, mycotic cerebral aneurysms may occur related to an infectious vasculitis. These may rupture, resulting in a cerebral hematoma. If the hematoma is evacuated without adequate antibiotic treatment, the bed of the hematoma near the site of the mycotic aneurysm may become infected, later forming an abscess.
Cerebral angiography is the best means with which to detect vasculitis or mycotic aneurysms. The mass effect caused by an abscess can be localized using angiographic criteria.
The beaded appearance of the blood vessels affected by active vasculitis may be mistaken for movement on the part of the patient.
-
Brain abscess. Axial CT scan in a patient who presented with a headache, fever, and a history of a recent pneumonia demonstrates a poorly defined area of posterior parietal brain edema (arrows). Early cerebritis may not outline a focal mass clearly.
-
Brain abscess. Axial nonenhanced cranial CT scan in a patient who presented with fever, headache, and a previous paranasal sinus infection demonstrates a poorly defined pattern of mass effect and low attenuation in the left temporal lobe. The pattern is consistent with possible early cerebritis; however, glioma and infarct may have similar presentations.
-
Brain abscess. Axial CT scan with intravenous (IV) contrast enhancement in a patient with fever, headache, and a recent history of pneumonia. An area of ringlike enhancement (yellow arrow) is noted within a much larger pattern of edema (white arrow). The central core of the abscess (black arrow) does not enhance, which is consistent with central necrosis.
-
Brain abscess. Axial CT scan with intravenous (IV) contrast enhancement in a patient who presented with headache and fever. Initial CT scan demonstrated mass effect and edema within the left temporal lobe. Since the edema and mass pattern were poorly defined, a biopsy of the left temporal lobe was performed to exclude a tumor. Following resection of the temporal lobe abscess, extracranial, subdural, and intracerebral abscesses developed (arrows).
-
Brain abscess. Coronal multiplanar reformatted CT scan in a patient who developed temporal brain abscesses (yellow arrows) and a left-sided extracranial abscess (white arrow) following surgery of the left temporal skull.
-
Brain abscess. Three-dimensional surface model of a cranial CT scan in a patient with a postcraniotomy abscess. The large deformity in the skull indicates the route of abscess spread.
-
Brain abscess. Sagittal T1 weighted unenhanced MRI of the brain in a patient with fever following head trauma. Osteomyelitis of the skull developed in this patient following cranial trauma (yellow arrow. An abscess of the brain (red arrow) developed by direct extension of the infection beyond the skull. The leading edge of the cerebritis is marked by the pattern of mass effect within the deeper margins of the left parietal lobe (white arrow).
-
Brain abscess. Sagittal diffusion weighted unenhanced MRI of the brain in a patient with fever following head trauma. Osteomyelitis of the skull developed in this patient following cranial trauma. An abscess of the brain (white arrows) developed by direct extension of the infection beyond the skull. Cerebral abscesses may present with an intermediate degree of signal brightness, as in this case, when evaluated by diffusion-weighted protocols.
-
Brain abscess. Coronal T1-weighted post–gadolinium-enhanced MRI of the brain in a patient with fever following head trauma. Osteomyelitis of the skull developed in this patient following cranial trauma. Bilateral subdural abscesses (yellow arrow) developed by direct extension of the infection beyond the skull. The leading edge of the cerebritis is marked by the pattern of enhancement within the deeper margins of the left parietal lobe (white arrow).
-
Brain abscess. Axial CT scan obtained with intravenous (IV) contrast enhancement in a patient with fever and headaches. Because a definite diagnosis of abscess is difficult to determine in some patients in whom ring enhancement is not associated with an apparent source of infection, stereotactic biopsy and culture of a walled abscess may be necessary.
-
Brain abscess. Axial contrast-enhanced CT scan in a patient who was treated surgically for a depressed skull fracture. The left parietal cranial injury has become complicated by an abscess of the subgaleal space (SGA), of the epidural space (EDA), and within the left cerebral hemisphere (CA). Edema related to the abscess is indicated by the yellow arrow. The cerebral abscess wall enhances (white arrow).
-
MRI, axial T2. This examination demonstrates a moderately thin-walled brain abscess (solid arrow) with a surrounding brain edema pattern (broken arrow).
-
MRI, sagittal T2 fluid-attenuated inversion recovery (FLAIR). FLAIR is very sensitive in the detection of cerebritis and brain edema surrounding brain abscess.
-
Brain MRI, T1 with IV contrast. The examination demonstrates the characteristic ring enhancement associated with a brain abscess.
-
Brain abscess. Axial T2-weighted MRI in a patient with a right frontal abscess. Note the mass effect and surrounding edema. The wall of the abscess is relatively thin (black arrows).
-
Brain abscess. Axial T1-weighted MRI in a patient with a mature cerebral abscess of the right frontal lobe of the brain. Note the thick wall of the abscess with enhancement (black arrow). The central content of the abscess is dark on T1-weighted imaging with no enhancement (double white arrows.)
-
Brain abscess. Anterior view of a chest radiograph in a patient with thick-walled right lung abscess. The patient later developed a brain abscess.
-
Brain abscess. Axial fast spin-echo inversion recovery MRI in a patient with left orbital swelling. Orbital cellulitis may progress to intracranial abscess, as the infection spreads, by causing venous thrombosis and sepsis. Arrows indicate the nonfocal nature of the cellulitis in this patient.
-
Brain abscess. Axial contrast-enhanced CT scan in a patient with a 6-day history of right orbital pain and swelling. The optic nerve (black arrow) is displaced by an abscess that has formed posterior to the globe of the eye (white arrow). Such a mass may cause retro-orbital veins to clot, resulting in septic phlebothrombosis and the development of an intracranial abscess.
-
Brain abscess. Axial CT scan with intravenous (IV) contrast enhancement in a patient with fever and diplopia demonstrates an enhancing mass arising from within the ethmoid air cells, with expansion into the medial right orbit (black arrow). The optic nerve is in contact with the mass (blue arrow).
-
Brain abscess. Gadolinium-enhanced coronal T1-weighted MRI in a patient who presented with headache, fever, and diplopia. The right frontal lobe of the brain is shifted across the midline (double arrow) by an intracranial abscess (single black arrow) that has extended upward from the medial right orbit and medial ethmoid air cells (curved dotted arrow). Aspergillus organisms were recovered from the sinuses and brain tissue.
-
Brain abscess. Coronal T1-weighted gadolinium-enhanced MRI in a patient with sudden onset of diplopia, fever, and right orbital swelling. Note the enhancement within the right ethmoid sinuses from which the infection arose. The medial superior right maxillary sinus has been destroyed (yellow arrow).
-
Brain abscess. Coronal T1-weighted gadolinium-enhanced MRI of the orbits and sinuses in a patient who presented with diplopia, headache, and fever. An abscess is noted within the medial inferior right orbit. The right maxillary sinus (double white arrows) contains infected secretions and mucus.
-
Brain abscess. Surface 3-dimensional model of a craniofacial CT scan in a patient with headache, orbital swelling, and diplopia of 48 hours' duration. Note the remarkable degree of right orbital swelling, which has resulted in the right lid being closed.
-
Brain abscess. Axial fluid-attenuated inversion recovery (FLAIR) MRI in a patient with Nocardia-related abscess of the cerebellar vermis (black arrow).
-
Brain abscess. Axial T2-weighted fast spin-echo MRI in a patient with a Nocardia-related abscess of the midline cerebellum. Note the large area of increased signal, both within the abscess and within the surrounding cerebellum (black arrow).
-
Brain abscess. Anteroposterior chest radiograph in a chronically ill patient who has diabetes and has had prior coronary surgery. Note the infiltrate in the right lower lobe (black arrow). Pneumonia resulting from Nocardia infection provided the source for an abscess of the midline cerebellum.
-
Brain abscess. Coronal T1-weighted spin-echo gadolinium-enhanced MRI demonstrates a central zone of enhancement within the abscess, with a zone of decreased brightness (edema, white arrow). Nocardia organisms were cultured from within the abscess cavity.
-
Brain abscess. Sagittal T1-weighted spin-echo gadolinium-enhanced MRI demonstrates an enhanced mass within the right medial cerebellum (yellow arrow). The thick-walled cystic mass was opened. Nocardia organisms were cultured from within the abscess.
-
Brain abscess. Nocardia organisms (black arrows) were identified on this microscopic slide of the aspirate from an abscess of the midline cerebellum (silver stain, original magnification X100).
-
Brain abscess. Axial fluid-attenuated inversion recovery (FLAIR) MRI of a left occipital-parietal brain abscess. The edema pattern (white arrows) surrounds the central abscess (A). A secondary (daughter) abscess is noted anterior to the primary abscess cavity.
-
Brain abscess. Axial diffusion weighted echo-planar MRI of a left occipital-parietal abscess. Both the primary and secondary (daughter) abscesses are demonstrated well (A). Fluid and necrotic tissue (bright area) are present within the abscess cavities, while edema surrounds the abscess cavities (black arrows).
-
Brain abscess. T1-weighted gadolinium-enhanced axial MRI of a primary abscess and a smaller daughter abscess (black arrows). Edema surrounding the abscess does not enhance (white arrows).
-
Brain abscess. Axial diffusion-weighted and T2-weighted echo-planar MRIs. A mildly increased signal brightness and mass effect are noted in the left thalamus and near the right caudate head. Analysis of a brain biopsy specimen demonstrated primary cerebral lymphoma.
-
Brain abscess. Axial T1-weighted gadolinium-enhanced MRI in a patient with multicentric brain lymphoma. Note the moderate mass effect on the left, with multiple areas of enhancement in both cerebral hemispheres (black arrows). This pattern is unlike the more geographic enhancement of a typical cerebral abscess.
-
Brain abscess. Coronal T2-weighted gradient-echo MRI in a patient with multicentric primary brain lymphoma. Mass effect, with associated surrounding edema in the left temporal lobe, is indicated by black arrows.
-
Brain abscess. Axial T2-weighted fast spin-echo MRI of the brain in a patient with multicentric brain lymphoma. Areas of intermediately increased brightness (black arrows) are noted lateral to the right thalamus and in the medial left temporal lobe.
-
Brain abscess. Thallous chloride Tl 201 single-photon emission CT scans demonstrate a large focus of increased activity in the left thalamic and left periventricular region of the brain (black arrows).
-
Brain abscess. Axial nonenhanced CT scan demonstrates mass effect (white arrows).
-
Brain abscess. Axial T2-weighted fluid-attenuated inversion recovery (FLAIR) MRI demonstrates 2 areas of increased signal brightness that are noted in the left frontal and the left parietal brain (black arrows) in a patient with toxoplasmosis.
-
Brain abscess. Axial diffusion-weighted echo-planar MRI in a patient with toxoplasmosis. Mildly increased brightness suggests 2 areas of diffusion restriction in the left frontal and left parietal brain. Increased brightness is due primarily to a T2-weighted contribution rather than diffusion restriction.
-
Brain abscess. Coronal T1-weighted gadolinium-enhanced MRI in a patient with toxoplasmosis. The area of surrounding edema does not enhance (white arrows), while a nodule of enhancement is demonstrated within the ring lesion (yellow arrow).
-
Brain abscess. Sagittal T1-weighted gadolinium-enhanced MRI in a patient with toxoplasmosis. The area of surrounding edema does not enhance (white arrows), while a nodule of enhancement is demonstrated within the ring lesion (yellow arrow). The use of multiple images in several projections allows identification of additional lesions in patients with toxoplasmosis.
-
Brain abscess. Sagittal T1-weighted gadolinium-enhanced MRI in a patient with toxoplasmosis. Multiple small cystic areas of enhancement are noted in the periventricular region of the third ventricle.
-
Brain abscess. Thallous chloride Tl 201 single-photon emission CT scan demonstrates a large focus of mildly increased activity in the left temporal and periventricular region of the brain (black arrows).
-
Brain abscess. A large left frontal low-density mass. The patient presented with headache and a low-grade fever. The abscess was drained. The abscess contained many white blood cells; however, no culture growth was noted. A diagnosis of an anaerobic gram-positive cocci was made on the basis of histological studies.
-
Brain abscess. Sagittal contrast-enhanced T1 MRI. The patient presented with headache and a low-grade fever. The abscess was drained. The abscess contained many white blood cells; however, no culture growth was noted. A diagnosis of an anaerobic gram-positive cocci was made on the basis of histological studies. MRI of the brain demonstrates mass effect and a ring enhancement in this case of a left frontal abscess.
-
Cerebral abscess. This T1 contrast-enhanced MRI of a right temporal abscess demonstrates an irregular mass with moderate peripheral enhancement. This image was obtained early in the clinical course. The etiology of the brain abscess was an abscessed tooth.
-
Cerebral abscess. Diffusion-weighted MRI demonstrates increased signal brightness within the abscess of the right temporal fossa.
-
MRI of right temporal lobe abscess. This T1 contrast-enhanced image demonstrates many of the characteristics of a typical brain abscess. Note the thick wall, which demonstrates significant enhancement following the administration of gadolinium-based contrast.



