Practice Essentials
Rheumatoid arthritis (RA) is a systemic inflammatory disease that results in cartilage and bone destruction. RA is characterized by a typical pattern and distribution of synovial joint involvement. Disorganization of the joint leads to deformities and loss of function. In the hands, the metacarpophalangeal (MCP), proximal interphalangeal (PIP), and thumb interphalangeal (IP) joints are most frequently involved. The distal interphalangeal (DIP) joints are involved only in the presence of a coexisting MCP or PIP disease. Tenosynovitis of the flexor tendons causes a reduction in finger flexion and grip strength. Nodular thickening in the tendon sheath may also produce a trigger finger.
The hands are affected symmetrically, and the disease process is usually visible first at the second and third MCP joints and the third PIP joint. The disease continues in the remainder of the MCP and PIP joints. Varying stages may be seen in different joints at a single point in time. DIP joint involvement without proximal involvement is rare. Erosions may be detected first either in the MCP and PIP joints or at the carpal bones. Erosions may also be seen at the intra-articular portion of the distal end of the radius or within the carpal bones. Carpal bone ankylosis is a common and fairly specific sign, particularly in the Asian population, in whom it tends to occur early in the disease process.
In the wrist, the early stages of RA cause tenosynovitis of the extensor tendons, causing swelling over the distal wrist. The ulnar styloid may become tender, which indicates inflammatory synovitis. The distal end of the ulna tends to sublux dorsally, and the carpal bones sublux anteriorly to the distal radius and ulna.
Although occasional flares of joint pain occur throughout the course of the disease, these can usually be controlled with the use of anti-inflammatory medication, especially early in their course. When joint subluxations and deformity take place, performing basic daily tasks (eg, writing and holding utensils) can become a problem. Some patients resort to the use of custom-designed writing instruments or utensils to overcome this difficulty. The primary effect of RA is in joint deformity and fusion, which occurs in the advanced stages. Permanent disability occurs in approximately 10-20% of patients.
Complications of therapy may be seen, such as generalized osteoporosis from steroid usage. Large bony erosions and severe osteopenia predispose patients to relatively atraumatic fractures. Long-term steroid use also predisposes patients to avascular necrosis.
(See the images below.)
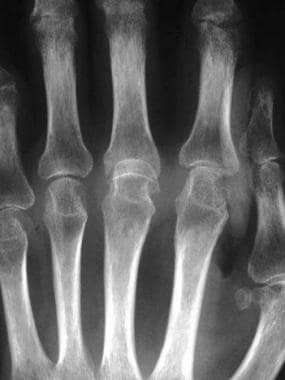
 Soft-tissue swelling and early erosions in the proximal interphalangeal joints in a patient with rheumatoid arthritis of the hands.
Soft-tissue swelling and early erosions in the proximal interphalangeal joints in a patient with rheumatoid arthritis of the hands.
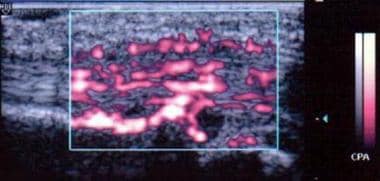 Power Doppler image shows hyperemic blood flow in the flexor tendon sheath in a patient with rheumatoid arthritis of the hands.
Power Doppler image shows hyperemic blood flow in the flexor tendon sheath in a patient with rheumatoid arthritis of the hands.
Preferred examination
The primary role of imaging in RA of the hands and wrists is to exclude septic arthritis. Percutaneous ultrasonography-guided aspiration may be useful for localizing and obtaining samples of any collection that can be found. (See the image below.)
 Ultrasonography-guided synovial biopsy of the second metacarpophalangeal joint of the right hand in a patient with rheumatoid arthritis of the hands. The biopsy needle is seen as a straight echogenic line on the left side of the image in an oblique orientation.
Ultrasonography-guided synovial biopsy of the second metacarpophalangeal joint of the right hand in a patient with rheumatoid arthritis of the hands. The biopsy needle is seen as a straight echogenic line on the left side of the image in an oblique orientation.
Radiography remains the first choice in imaging RA. Radiography is cheap, is easily reproducible, and allows easy serial comparison for assessment of disease progression. The main disadvantage is the absence of specific radiographic findings in early disease, since visualization of erosions may only be seen later. [1]
Magnetic resonance imaging (MRI) provides a more accurate assessment, as well as earlier detection of lesions. Magnetic resonance imaging (MRI) continues to develop as a treatment tool, with the main thrust being detection of early disease at a stage at which disease-modifying drugs can be used; however, the cost of the examination and the small size of the joints involved limit widespread use. [2, 1, 3, 4, 5]
Ultrasonography of specific joints based on radiographs may have a role as well. [2, 6]
Computed tomography (CT) has a minimal role in treating RA of the hands. Although CT is useful for demonstrating bony pathology, erosions in the small joints of the hands are evaluated best by using a combination of radiography and MRI. MRI also has the added advantage of being able to visualize bone marrow edema and synovial and soft-tissue involvement.
RA may occur as part of a mixed connective tissue disease in which clinical and radiologic appearances are not typical of one particular disease.
Radiography
RA is indicated on radiographs by the overall pattern and features of joint involvement. Although the presence of bony erosions is typical of RA, erosions are not specific because of the large number of other erosive arthritides. An absence of osteophyte formation and subchondral sclerosis is also indicative of RA rather than osteoarthritis. Of concern is the possibility of misdiagnosing another erosive arthropathy as RA or vice versa. Because the diagnosis of RA is a predominantly clinical one, the primary role of imaging is in follow-up observation. In the late stage (but not in the early stage), the deformities and joint fusion of RA are usually distinguishable from other causes of erosive arthropathy. No normal variants simulate RA.
Morphology
Usually, the earliest sign of RA is a periarticular soft-tissue swelling with a fusiform appearance. Normal fat planes may be obliterated, which occurs as a result of joint effusion, edema, and tenosynovitis. Juxta-articular osteopenia is another early sign, particularly during the acute inflammatory stage. Osteopenia subsequently becomes more generalized as the disease progresses. [7]
(See the images below.)
 Soft-tissue swelling and early erosions in the proximal interphalangeal joints in a patient with rheumatoid arthritis of the hands.
Soft-tissue swelling and early erosions in the proximal interphalangeal joints in a patient with rheumatoid arthritis of the hands.
 Prominent juxta-articular osteopenia in all interphalangeal joints in a patient with rheumatoid arthritis of the hands.
Prominent juxta-articular osteopenia in all interphalangeal joints in a patient with rheumatoid arthritis of the hands.
Initially, joint spaces in the small joints of the hands show widening as a result of effusion; however, with cartilage destruction, joint spaces narrow. Erosions usually begin at the bare area of the joint not covered by cartilage, such as the intracapsular articular margins. Marginal erosions occur as a result of direct mechanical action of the hypertrophied synovium and granulation tissue. (See the images below.)
 Well-defined bony erosions in the carpal bones and metacarpal bases in a patient with rheumatoid arthritis of the hands.
Well-defined bony erosions in the carpal bones and metacarpal bases in a patient with rheumatoid arthritis of the hands.
 Multiple erosions with deformity of the carpal bones in a patient with rheumatoid arthritis of the hands.
Multiple erosions with deformity of the carpal bones in a patient with rheumatoid arthritis of the hands.
 Follow-up radiograph obtained after an 18-month interval in a patient with rheumatoid arthritis of the hands. Ankylosis of the carpal bones has occurred, with enlargement of the erosions.
Follow-up radiograph obtained after an 18-month interval in a patient with rheumatoid arthritis of the hands. Ankylosis of the carpal bones has occurred, with enlargement of the erosions.
The forces of tendon imbalance and capsular contraction result in joint subluxation and malalignment. Characteristic appearances include the boutonnière (flexion at the PIP joint and extension at the DIP joint) and swan-neck (extension at the PIP joint and flexion at the DIP joint) deformities at the IP joints. Ulnar deviation is also commonly present at the MCP joints. MCP joints may also dislocate and have overriding ends (main en lorgnette or telescoping joints). Subluxations are progressive and may occur with or without the presence of bony erosions. Tendinous involvement of RA may result in rupture of the tendon, causing increased disability. If significant involvement of the scapholunate joint is present, laxity or rupture may cause rotatory subluxation of the scaphoid. (See the images below.)
 Subluxation in the metacarpophalangeal joints, with ulnar deviation, in a patient with rheumatoid arthritis of the hands.
Subluxation in the metacarpophalangeal joints, with ulnar deviation, in a patient with rheumatoid arthritis of the hands.
 Subluxation at the third metacarpophalangeal joint and marginal erosions at the heads of the second to fourth metacarpals in a patient with rheumatoid arthritis of the hands.
Subluxation at the third metacarpophalangeal joint and marginal erosions at the heads of the second to fourth metacarpals in a patient with rheumatoid arthritis of the hands.
Fusion or joint ankylosis is common in the later stages of RA. Fusion usually takes place in a deformed or malaligned position. This further reduces the functionality of the hand and affects independence in the activities of daily living. In the end stages, extensive erosions may combine to result in resorption and tapering of the ends of the bones. (See the images below.)
 Partial collapse of fused carpal bones with subluxation at the radiocarpal joint in a patient with rheumatoid arthritis of the hands.
Partial collapse of fused carpal bones with subluxation at the radiocarpal joint in a patient with rheumatoid arthritis of the hands.
Magnetic Resonance Imaging
MRI provides images with good delineation of soft-tissue changes, cartilaginous defects, and osseous erosions associated with RA. In particular, the ability to detect synovial hypertrophy and pannus formation before the onset of bony erosions has become more valuable with the advent of disease-modifying antirheumatic drugs. The drugs, which retard the progression of RA, are most effective in the early stages of disease. [3, 4, 8, 9, 10] MRI has been shown to be more sensitive to early changes in RA, and in the appropriate clinical setting, it is more accurate than plain radiography in the diagnosis of RA. Routine use of MRI in evaluating rheumatoid arthropathy in the hands and wrist has been limited by the relatively high cost, the difficulty in positioning disabled patients, and the inability to image several joints simultaneously. [11]
Signal intensity of the inflamed synovial lining may vary markedly on T1- and T2-weighted images. An inflamed synovial lining usually demonstrates low signal intensity on T2-weighted images, and the images may be even darker if hemosiderin or a predominantly fibrous component is present within the lining. Tenosynovitis resulting from inflammation is seen as high–signal-intensity fluid on T2-weighted sequences. (See the image below.)
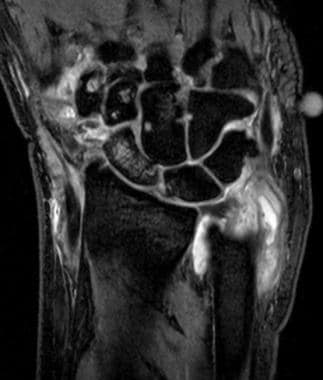 Coronal fine-section gradient echo MR image demonstrates multiple erosions in the carpal bones and bases of the metacarpals, with pannus formation around the distal ulna.
Coronal fine-section gradient echo MR image demonstrates multiple erosions in the carpal bones and bases of the metacarpals, with pannus formation around the distal ulna.
The intravenous (IV) administration of a gadolinium-based contrast agent allows better distinction of inflammatory soft-tissue changes and can help differentiate pannus from eburnation. In addition, rapid enhancement of proliferative inflammatory synovium has been reported, compared to minimal signal change in healthy soft tissue and bone. Fat suppression and fast dynamic scanning have also been used to increase the sensitivity of synovial imaging. [12, 13, 14]
MRI is clearly superior to radiography in the early detection of bone erosions. MRI is more sensitive to bone marrow edema. Bright lesions on T2-weighted images often do not correspond to findings on radiographs or T1-weighted images. These lesions are believed to represent potentially reversible pre-erosive changes. [15, 16] (See the images below.)
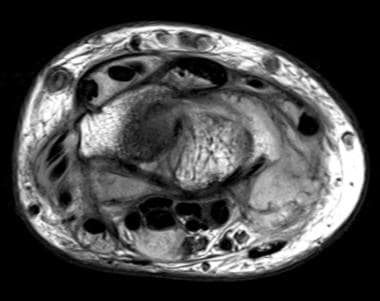 Axial proton-density weighted MR image at the level of the radio-carpal joint shows extensive tenosynovitis involving the dorsal extensor and volar flexor tendons, with fluid in the tendon sheaths.
Axial proton-density weighted MR image at the level of the radio-carpal joint shows extensive tenosynovitis involving the dorsal extensor and volar flexor tendons, with fluid in the tendon sheaths.
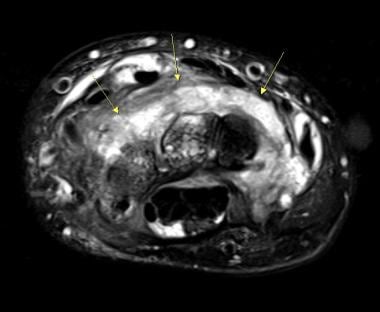 Axial T2-weighted fat-suppresed MR image at the level of the carpal bones shows diffuse synovial hypertrophy over the dorsal aspect (arrows), with a heterogenous appearance and adjacent fluid. Fluid is also present in the dorsal extensor tendon sheaths.
Axial T2-weighted fat-suppresed MR image at the level of the carpal bones shows diffuse synovial hypertrophy over the dorsal aspect (arrows), with a heterogenous appearance and adjacent fluid. Fluid is also present in the dorsal extensor tendon sheaths.
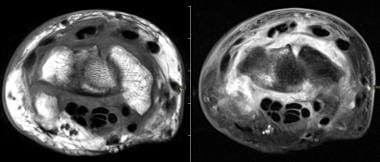 Axial T1-weighted MR image of the wrist before and after gadolinium administration shows diffuse contrast enhancement in the areas of synovial hypertrophy and thickening, over both the dorsal and volar aspects.
Axial T1-weighted MR image of the wrist before and after gadolinium administration shows diffuse contrast enhancement in the areas of synovial hypertrophy and thickening, over both the dorsal and volar aspects.
Olech et al evaluated the sensitivity and specificity of MRI in detecting erosions, bone edema, and synovitis in the metacarpophalangeal and wrist joints for RA by comparing scans of bilateral hands and wrists of 40 healthy subjects with those of 40 RA patients using 0.2 T extremity-MRI. A total of 3,360 bones were evaluated, and patients with RA were found to have significantly more erosions, as well as higher scores for bone edema and synovitis. Although age had a significant effect on the number of erosions in both groups, age became insignificant in RA patients when disease duration was factored in. The number of erosions correlated with positive rheumatoid factor and higher C-reactive protein values. Bone marrow edema was the most specific MRI lesion for RA, with 65% sensitivity and 82.5% specificity. [17]
In a study by Lisbona et al, subclinical inflammation was identified by MRI in 96.4% of patients with RA who had achieved sustained clinical remission. Significantly higher scores of bone marrow edema were observed after sustained remission in patients with progression of erosions, as compared to patients with no erosion progression. According to the authors of the study, persistence of higher scores of BME may explain the progression of bone erosions in patients with persistent clinical remission. [18]
According to a study by Taniguchi et al, using MRI with maximum intensity projection (MIP) images, together with palpation, makes detailed evaluation of synovitis of the hand in RA easy. The researchers concluded that MIP images may predict further joint damage because they allow semiquantitative estimation of the degree of thickening of the synovial membrane. [19]
Contrast-enhanced MRI with maximum intensity projection (MRI-MIP) has been found to be a useful imaging technique to evaluate synovitis in hands with RA. [20]
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). These diseases have occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or magnetic resonance angiography (MRA) scans. NSF/NFD are debilitating and sometimes fatal diseases. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Schwenzer et al investigated dynamic contrast-enhanced MRI in the differential diagnosis of psoriatic arthritis (PA) and RA in the hand and wrist by evaluating 45 patients (31 with RA; 14 with PA) with a 3-T whole-body MR unit. There was a statistically significant difference observed between the 2 groups regarding relative synovial enhancement after 15 minutes following contrast injection; however, there was no difference in relative enhancement at 35 seconds, 52 seconds, or 3 minutes. Significant correlations were found between inflammatory parameters and dynamic contrast-enhanced parameters in patients with RA but not in those with PA. [21]
Ultrasonography
High-resolution sonography with a high-frequency probe is used for evaluation of the small joints in RA (see the image below). Joint effusion is hypoechoic, while the hypertrophic synovium is more echogenic. Rheumatoid nodules are seen as fluid-filled round cavities with sharp borders. Bone erosions may be seen as irregularities in the hyperechoic cortex. [22, 23, 24]
 Illustration of the scanning technique. Photograph depicts the typical scanning technique with application of the Entos Probe to the volar (flexor) aspect of the third metacarpophalangeal joint. The technique allows visualization of the joint surfaces, flexor tendon, and synovial sheaths in patients with rheumatoid arthritis.
Illustration of the scanning technique. Photograph depicts the typical scanning technique with application of the Entos Probe to the volar (flexor) aspect of the third metacarpophalangeal joint. The technique allows visualization of the joint surfaces, flexor tendon, and synovial sheaths in patients with rheumatoid arthritis.
Complications of RA, such as tenosynovitis and tendon rupture, can also be visualized by using ultrasonography. This is most useful in the MCP and IP joints. The carpal bones and the carpometacarpal joints are not visualized as well because of their irregular configuration and deeper location. [25, 26, 27, 28, 29, 30]
Sonography has been applied to the assessment of RA with the goal of improving on the current standard of conventional radiography. Ultrasonography, especially when augmented by amplitude color Doppler (ACD) imaging, has also provided clinically useful information in the assessment of RA. Originally, ACD or power Doppler scanning was developed as an improvement to existing vascular sonographic imaging techniques to delineate stenoses by imaging blood flowing in vessel lumina by virtue of higher sensitivity to flow and lack of directional dependence. [31]
ACD imaging has been applied to RA with the goal of evaluating the manifestation of hyperemia in the inflammatory joint tissues at the symptomatic sites of disease. Synovial hyperemia is a fundamental pathophysiologic feature of RA. Most likely, synovial hyperemia is the principal factor underlying the hallmark x-ray observation of periarticular demineralization on radiographs of patients with RA, and it is believed to occur in proportion to joint-destructive disease activity. Hyperemia in the tendon sheath is common as well. (See the images below.)
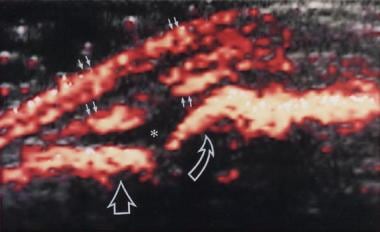 Amplitude color Doppler sonogram in a patient with active rheumatoid arthritis. Dorsal (extensor) surface of the second metacarpophalangeal joint is imaged. Intense-amplitude Doppler color flow signal demarcates the inflamed synovium (ie, joint pannus) resulting from severe hyperemia. Solid arrows indicate the extensor tendon sheath and dorsal and volar margins. Straight open arrow indicates the synovium of the joint overlying the proximal phalanx of the second digit. Curved open arrow indicates the inflamed synovium overlying the metacarpal. The asterisk indicates a small amount of anechoic fluid in the joint space.
Amplitude color Doppler sonogram in a patient with active rheumatoid arthritis. Dorsal (extensor) surface of the second metacarpophalangeal joint is imaged. Intense-amplitude Doppler color flow signal demarcates the inflamed synovium (ie, joint pannus) resulting from severe hyperemia. Solid arrows indicate the extensor tendon sheath and dorsal and volar margins. Straight open arrow indicates the synovium of the joint overlying the proximal phalanx of the second digit. Curved open arrow indicates the inflamed synovium overlying the metacarpal. The asterisk indicates a small amount of anechoic fluid in the joint space.
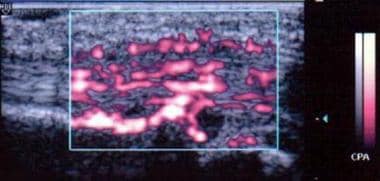 Power Doppler image shows hyperemic blood flow in the flexor tendon sheath in a patient with rheumatoid arthritis of the hands.
Power Doppler image shows hyperemic blood flow in the flexor tendon sheath in a patient with rheumatoid arthritis of the hands.
Two reports in the literature have explored a possible role for Doppler ultrasonography in evaluating arthritis, especially RA, on the basis of synovial hyperemia. Newman et al [32] used a 3-level semiquantitative approach by trained radiologists to grade Doppler flow subjectively in patients with RA, psoriatic arthritis, and calcium pyrophosphate deposition disease arthritis. The investigators found that the degree of abnormal tissue hyperemia visualized correlates grossly with the severity of local disease activity as measured by synovial-fluid white blood cell (WBC) counts and patients' subjective estimates of symptoms. The report did not include joint examinations or other physical/functional measurements.
Hau et al [33] from the University Hospital of Wurzburg, Germany, reported findings from ultrasound in the MCP and PIP joints of 34 patients with RA and 15 control subjects over a 6-month period. In the protocol, each patient was examined only once. Patients were stratified into 3 groups based on swelling and tenderness. Ultrasonography was performed by using a Siemens Doppler unit and a 5- to 13-MHz linear-array transducer operating at 12 MHz. The authors identified joint pannus on gray-scale images as hypoechoic soft tissue adjacent to the articular surfaces and described the pannus distribution as favoring the radial side of the joints. Velocity color Doppler (ie, conventional direction-sensitive Doppler) imaging was used to evaluate vascularization and blood flow in the rheumatoid pannus as a surrogate marker of inflammation. The quantitation method used was analogous to that used by one of the coauthors of this article in preliminary studies.
A simple image-based quantification was obtained in the study by Hau et al [33] by summing the color pixels within all joints in each patient classification after selection of regions of interest within each joint. The result was a unitless numerical scale that showed a greater than tenfold difference between patients with active RA and controls. From the preliminary investigations, both the Newman and Hau studies [32, 33] concluded that power Doppler ultrasonography can reflect disease activity in RA, and each group suggested further research in this area.
Teh et al [34] evaluated quantitative power Doppler ultrasonography for the assessment of therapeutic response in rheumatoid synovitis in 13 consecutive patients over 7 months, with correlation to serum inflammatory markers and clinical evaluation. Quantitiative power Doppler spectra were derived within select regions of interest from each patient’s scan, both before and after treatment; essentially, the method used was an automated pixel-counting technique similar to that of Hau. There was extremely good correlation between the image-based quantitation of synovial hyperemia and the clinical and laboratory assessment of disease activity in this study. Thus, quantitative power Doppler ultrasonography was able to accurately depict the patients’ response to treatment. The authors of the study felt that the addition of quantitative power Doppler ultrasonography to the routine assessment of therapeutic response in RA yielded more accurate findings than existing clinical and laboratory methods alone.
Strunk et al [35] compared quantified power Doppler ultrasonography with laboratory measurement of serum vascular endothelial growth factor (VEGF level) as markers for disease activity, finding a very high correlation (P< 0.0001) for ultrasound and no relation with the immediate serum VEGF level in the same patient. Salaffi et al [36] evaluated quantified power Doppler ultrasonography augmented by the use of IV ultrasound contrasts, such as Levovist, using a quantitative time-intensity curve integration to arrive at the quantification in arbitrary units. The results showed a correlation of the Doppler signal to other measures of disease and treatment efficacy.
Fukae et al studied the relation between synovial vascularity, assessed by quantitative power Doppler ultrasonography (PDUS), and structural bone damage in a single finger joint by comparing 190 metacarpophalangeal (MCP) and 190 proximal interphalangeal (PIP) joints of 19 patients with active RA who received disease-modifying antirheumatic drugs (DMARDs). The authors found that quantitative PDUS was significantly correlated with enhancement rate of MRI in each single finger joint. Comparing quantitative synovial vascularity and radiographic change in single MCP or PIP joints, the level of vascularity at baseline showed significant positive correlation with radiographic progression at the 20th week. Quantitative PDUS was found to be more useful than the semiquantitative method in evaluating synovial vascularity in a single finger joint. [37]
Fiocco et al [38] found that both C-reactive protein and Doppler findings reliably measured response to treatment with etancercept, an anti–tumor necrosis factor-alpha medication that has shown considerable efficacy in rheumatoid arthritis.
Research in this area is ongoing, but according to published reports, quantified power Doppler ultrasonography is a reproducible and reliable surrogate indicator of disease activity, which can predict and evaluate treatment response with a greater degree of sensitivity and specificity than other available clinical methodologies. [39, 40]
Questions & Answers
Overview
What is rheumatoid arthritis (RA) and how does it affect the hands?
What is the role of hand imaging in the workup of rheumatoid arthritis (RA)?
Which findings on radiography are characteristic of rheumatoid arthritis (RA) in the hands?
What is the characteristic distribution of rheumatoid arthritis (RA) in the hands on radiographs?
What is the accuracy of hand radiography in the diagnosis of rheumatoid arthritis (RA)?
What is the role of CT scanning of the hand in the evaluation of rheumatoid arthritis (RA)?
What is the role of MRI of the hand in the evaluation of rheumatoid arthritis (RA)?
What is the accuracy of MRI of the hands in the diagnosis of rheumatoid arthritis (RA)?
What is the role of ultrasonography of the hands in the workup of rheumatoid arthritis (RA)?
-
Soft-tissue swelling and early erosions in the proximal interphalangeal joints in a patient with rheumatoid arthritis of the hands.
-
Prominent juxta-articular osteopenia in all interphalangeal joints in a patient with rheumatoid arthritis of the hands.
-
Well-defined bony erosions in the carpal bones and metacarpal bases in a patient with rheumatoid arthritis of the hands.
-
Multiple erosions with deformity of the carpal bones in a patient with rheumatoid arthritis of the hands.
-
Follow-up radiograph obtained after an 18-month interval in a patient with rheumatoid arthritis of the hands. Ankylosis of the carpal bones has occurred, with enlargement of the erosions.
-
Subluxation in the metacarpophalangeal joints, with ulnar deviation, in a patient with rheumatoid arthritis of the hands.
-
Subluxation at the third metacarpophalangeal joint and marginal erosions at the heads of the second to fourth metacarpals in a patient with rheumatoid arthritis of the hands.
-
Marked ankylosis of most of the carpal bones in a patient with rheumatoid arthritis of the hands.
-
Partial collapse of fused carpal bones with subluxation at the radiocarpal joint in a patient with rheumatoid arthritis of the hands.
-
Coronal fine-section gradient echo MR image demonstrates multiple erosions in the carpal bones and bases of the metacarpals, with pannus formation around the distal ulna.
-
Axial proton-density weighted MR image at the level of the radio-carpal joint shows extensive tenosynovitis involving the dorsal extensor and volar flexor tendons, with fluid in the tendon sheaths.
-
Axial T2-weighted fat-suppresed MR image at the level of the carpal bones shows diffuse synovial hypertrophy over the dorsal aspect (arrows), with a heterogenous appearance and adjacent fluid. Fluid is also present in the dorsal extensor tendon sheaths.
-
Axial T1-weighted MR image of the wrist before and after gadolinium administration shows diffuse contrast enhancement in the areas of synovial hypertrophy and thickening, over both the dorsal and volar aspects.
-
Illustration of the scanning technique. Photograph depicts the typical scanning technique with application of the Entos Probe to the volar (flexor) aspect of the third metacarpophalangeal joint. The technique allows visualization of the joint surfaces, flexor tendon, and synovial sheaths in patients with rheumatoid arthritis.
-
Amplitude color Doppler sonogram in a patient with active rheumatoid arthritis. Dorsal (extensor) surface of the second metacarpophalangeal joint is imaged. Intense-amplitude Doppler color flow signal demarcates the inflamed synovium (ie, joint pannus) resulting from severe hyperemia. Solid arrows indicate the extensor tendon sheath and dorsal and volar margins. Straight open arrow indicates the synovium of the joint overlying the proximal phalanx of the second digit. Curved open arrow indicates the inflamed synovium overlying the metacarpal. The asterisk indicates a small amount of anechoic fluid in the joint space.
-
Power Doppler image shows hyperemic blood flow in the flexor tendon sheath in a patient with rheumatoid arthritis of the hands.
-
Ultrasonography-guided synovial biopsy of the second metacarpophalangeal joint of the right hand in a patient with rheumatoid arthritis of the hands. The biopsy needle is seen as a straight echogenic line on the left side of the image in an oblique orientation.










