Practice Essentials
Blastomyces dermatitidis is a thermally dimorphic fungus that causes the systemic pyogranulomatous disease termed blastomycosis. This pathogen is endemic to North America, particularly in the states bordering the Mississippi and Ohio rivers, the Great Lakes, and the St. Lawrence Seaway. [1] B gilchristii has also been identified as a mode of infection. [2, 3] Blastomycosis is the least common of the endemic systemic mycoses; the other, more common mycoses include histoplasmosis and coccidioidomycosis. Blastomycosis most commonly presents as a pulmonary infection after inhalation of spores. Severe, life-threatening complications may occur, such as acute respiratory distress syndrome (ARDS). Extrapulmonary disease occurs in 25-30% of patients after dissemination from the lungs; the skin is the most common site of extrapulmonary disease. [4, 5, 6, 7, 8, 9, 10, 11, 12]
(See the images below.)
 A patient visited central Canada several months ago. He developed cough, fever, and dyspnea. Chest radiograph demonstrates focal patchy opacity in the lingula. Blastomyces dermatitidis was identified on bronchoscopy.
A patient visited central Canada several months ago. He developed cough, fever, and dyspnea. Chest radiograph demonstrates focal patchy opacity in the lingula. Blastomyces dermatitidis was identified on bronchoscopy.
 Lateral chest radiograph (same patient as in the previous image) reveals the ill-defined lingular opacity and an absence of pleural effusions.
Lateral chest radiograph (same patient as in the previous image) reveals the ill-defined lingular opacity and an absence of pleural effusions.
Benedict et al reported on the incidence of blastomycosis in 5 states: Arkansas, Louisiana, Michigan, Minnesota, and Wisconsin. Surveillance identified 4,441 cases during the period 1987–2018 (mean, 192 cases/yr). The mean annual incidence was less than 1 case per 100,000 population in most areas, but it was more than 20 cases per 100,000 population in some northern counties of Wisconsin. The median patient age was 46 years; 2,892 (65%) patients were male; 1,662 (57%) were hospitalized; and 278 (8%) died. The median time from onset of symptoms to diagnosis was 33 days. [13]
In a 2014 study, according to the United States Agency for Healthcare Research and Quality, states within the Mississippi and Ohio River valleys had the highest age-adjusted hospitalization incidence of blastomycosis cases, with Wisconsin having the highest incidence (2.9 hospitalizations per 100,000 person-years). From 2000 to 2011, blastomycosis-associated hospitalizations increased significantly in Illinois and Kentucky, with an average annual increase of 4.4% and 8.4%, respectively. Overall, 64% of blastomycosis-associated hospitalizations were among men, and the median age at hospitalization was 53 years. [10]
The diagnosis of thoracic blastomycosis is made on the basis of a demonstration of organisms in culture or on fungal stains (10% potassium hydroxide) of sputum, bronchoscopy specimens, or secretions obtained from cerebrospinal fluids or dermal, subcutaneous, or other lesions. [9] Cultures are positive in more than 90% of cases. Culture growth may take from one to several weeks.
Radiographic findings are nonspecific and variable, with radiographic patterns of thoracic blastomycosis being indistinguishable from those of other mycotic infections. In addition, the signs and symptoms of blastomycosis overlap with not only other fungal infections but also bacterial and viral pneumonia, influenza, and tuberculosis. [14] Delayed and/or misdiagnosis is not uncommon and results in overuse of antibiotics. [15]
In a study of 36 patients (age range, 3 mo to 17 yr) by Rozovsky et al, consolidation was found in 94.4% of patients and was unilateral in 76.5% and bilateral in 23.5%. The upper lobes were involved in 70.6%, and middle lobes in 47.1%. Air bronchograms were identified in 76.5% of patients with consolidations; masslike consolidation was found in 55.9%; cavitation in 38.2%; and bubbly pattern (ie, multiple small cavities) in 32.4%. [16]
Chest radiography is the first imaging study performed. The most common pattern observed is acute, nonspecific focal lung opacity, which is found in 25-75% of patients. [17, 18, 19, 20, 21]
Pulmonary blastomycosis can be present on radiography in the airspace, lobar, and interstitial areas, with airspace consolidation being the most common. [2, 22, 23]
ICD-10 codes
The ICD-10 codes include the following:
-
B40.0 Acute pulmonary blastomycosis
-
B40.1 Chronic pulmonary blastomycosis
-
B40.2 Pulmonary blastomycosis, unspecified
-
B40.3 Cutaneous blastomycosis
-
B40.7 Disseminated blastomycosis
-
B40.8 Other forms of blastomycosis
-
B40.9 Blastomycosis, unspecified
Radiography
Chest radiographs usually reveal focal lung opacities in the upper lobes (seen in 25-75% of patients); these opacities are often nodular in character. In adults, the upper lobes are affected more frequently than the lower lobes; the ratio is approximately 2:1. In children, opacities most commonly involve the lower lobes. Lung opacities may be patchy or confluent; they may be subsegmental, segmental, or nonsegmental (see the images below). The radiographic appearance is similar to that seen with community acquired pneumonia; slow improvement, lack of change, or even progression of disease over time should raise the possibility of granulomatous infection.
In a single-institution retrospective study, by Rozovsky et al, of 36 pediatric patients (age 0-18 yr) with pulmonary blastomycosis who underwent chest imaging, the most common pattern of lung involvement was a combination of consolidations (94.4%) with bilateral lung nodules (50%) and reticulonodular opacification (41.2%). The upper (70.6%) and middle (47.1%) lobes were most often affected. [24]
 A patient visited central Canada several months ago. He developed cough, fever, and dyspnea. Chest radiograph demonstrates focal patchy opacity in the lingula. Blastomyces dermatitidis was identified on bronchoscopy.
A patient visited central Canada several months ago. He developed cough, fever, and dyspnea. Chest radiograph demonstrates focal patchy opacity in the lingula. Blastomyces dermatitidis was identified on bronchoscopy.
 Lateral chest radiograph (same patient as in the previous image) reveals the ill-defined lingular opacity and an absence of pleural effusions.
Lateral chest radiograph (same patient as in the previous image) reveals the ill-defined lingular opacity and an absence of pleural effusions.
The next most common radiographic presentation (occurring in as many as 30% of patients) is that of a focal discrete mass, either single or multiple. The mass is usually well circumscribed; such masses are variable in size and occasionally contain air-bronchograms. When solitary, a mass may mimic primary carcinoma, especially when associated with unilateral lymph node enlargement or bone destruction (see the images below).
 Chest radiograph demonstrates a spiculated mass overlying the left hilum. This radiographic finding mimics that of bronchogenic carcinoma; thus, a biopsy is needed for tissue diagnosis.
Chest radiograph demonstrates a spiculated mass overlying the left hilum. This radiographic finding mimics that of bronchogenic carcinoma; thus, a biopsy is needed for tissue diagnosis.
 Lateral chest radiograph (same patient as in the previous image) reveals the central mass overlying the left hilum.
Lateral chest radiograph (same patient as in the previous image) reveals the central mass overlying the left hilum.
Cavitation occurs less commonly in patients with blastomycosis than in patients with tuberculosis or chronic histoplasmosis; the reported incidence is approximately 15-20% (see the images below).
 Chest radiograph from a patient with pulmonary blastomycosis demonstrates multiple nodular lesions, some of which are cavitating, in the left lower lobe. Cavitation occurs in 15-20% of patients with blastomycosis.
Chest radiograph from a patient with pulmonary blastomycosis demonstrates multiple nodular lesions, some of which are cavitating, in the left lower lobe. Cavitation occurs in 15-20% of patients with blastomycosis.
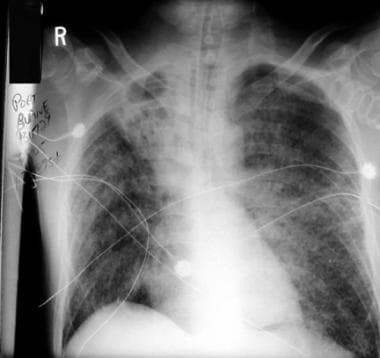 Chest radiograph from a patient with disseminated blastomycosis demonstrates diffuse miliary infiltrates associated with respiratory failure that required mechanical ventilation. In this patient, dense opacification with cavitation is seen in the right upper lobe. In a minority of patients, a diffuse micronodular pattern is seen; such a pattern results from hematogenous spread of the disease.
Chest radiograph from a patient with disseminated blastomycosis demonstrates diffuse miliary infiltrates associated with respiratory failure that required mechanical ventilation. In this patient, dense opacification with cavitation is seen in the right upper lobe. In a minority of patients, a diffuse micronodular pattern is seen; such a pattern results from hematogenous spread of the disease.
In a minority of patients, a miliary or diffuse interstitial disease pattern is seen at presentation; patients have respiratory failure and need mechanical ventilation. This pattern may be observed in previously healthy immunocompromised patients. In many patients, the focal lung opacities or mass may be observed in association with the diffuse interstitial pattern, a finding that supports the hypothesis that pulmonary dissemination occurs from a focal pulmonary site (see the image below).
 Chest radiograph from a patient with blastomycosis reveals left hilar lymphadenopathy, an uncommon finding in patients with blastomycosis.
Chest radiograph from a patient with blastomycosis reveals left hilar lymphadenopathy, an uncommon finding in patients with blastomycosis.
In contrast to histoplasmosis, hilar and mediastinal adenopathy and calcification are uncommon (occurring in 10-20% of cases).
Pleural involvement and significant effusion are uncommon (20%). Rarely, lung or pleural involvement extends into adjacent bones or soft tissues. Pleural thickening without free effusion is a more common radiographic finding.
Osteolytic lesions in the skeleton usually are associated with superficial abscesses. Rarely, mediastinal involvement results in superior vena cava obstruction or brachial plexopathy.
Computed Tomography
Computed tomography (CT) scan findings of thoracic blastomycosis are variable. As with chest radiography, nonspecific lung parenchymal opacification is most commonly observed, followed by mass lesions (see the images below).
 A patient on mechanical ventilation because of acute respiratory distress secondary to diffuse blastomycosis. Bilateral pneumothoraces are the result of barotrauma. Right chest wall subcutaneous emphysema resulted from chest tube placement.
A patient on mechanical ventilation because of acute respiratory distress secondary to diffuse blastomycosis. Bilateral pneumothoraces are the result of barotrauma. Right chest wall subcutaneous emphysema resulted from chest tube placement.
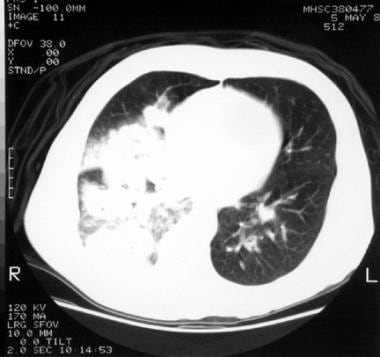 Chest CT image reveals patchy, dense lung opacification in the right middle and lower lobes. This is the most common presentation of blastomycosis. Lung opacities may be patchy or confluent and subsegmental or nonsegmental.
Chest CT image reveals patchy, dense lung opacification in the right middle and lower lobes. This is the most common presentation of blastomycosis. Lung opacities may be patchy or confluent and subsegmental or nonsegmental.
 Chest CT reveals a thick wall cavity in the left lower lobe with surrounding focal parenchymal disease; needle biopsy of this lesion confirmed blastomycosis. Cavitation occurs in 15-20% of patients with blastomycosis.
Chest CT reveals a thick wall cavity in the left lower lobe with surrounding focal parenchymal disease; needle biopsy of this lesion confirmed blastomycosis. Cavitation occurs in 15-20% of patients with blastomycosis.
In a review of CT findings in 16 patients with pulmonary blastomycosis, Winer-Muram et al reported the following [25] :
-
A localized mass - 14 patients
-
Consolidation - 9 patients
-
Masses ranging from 3-16 cm in diameter (mean, 8 cm)
-
A majority of masses containing air bronchograms - 12 of 14 patients
-
Unilateral abnormalities - 11 patients
-
Abnormalities involving both lung - 5 patients
In addition, no lobar predominance was noted. Cavitation was observed in 2 patients; calcified hilar nodes was observed in 7 patients; and enlarged noncalcified nodes was observed in 1 patient.
-
A patient visited central Canada several months ago. He developed cough, fever, and dyspnea. Chest radiograph demonstrates focal patchy opacity in the lingula. Blastomyces dermatitidis was identified on bronchoscopy.
-
Lateral chest radiograph (same patient as in the previous image) reveals the ill-defined lingular opacity and an absence of pleural effusions.
-
A patient on mechanical ventilation because of acute respiratory distress secondary to diffuse blastomycosis. Bilateral pneumothoraces are the result of barotrauma. Right chest wall subcutaneous emphysema resulted from chest tube placement.
-
Chest CT image reveals patchy, dense lung opacification in the right middle and lower lobes. This is the most common presentation of blastomycosis. Lung opacities may be patchy or confluent and subsegmental or nonsegmental.
-
Chest radiograph demonstrates a spiculated mass overlying the left hilum. This radiographic finding mimics that of bronchogenic carcinoma; thus, a biopsy is needed for tissue diagnosis.
-
Lateral chest radiograph (same patient as in the previous image) reveals the central mass overlying the left hilum.
-
Chest radiograph from a patient with pulmonary blastomycosis demonstrates multiple nodular lesions, some of which are cavitating, in the left lower lobe. Cavitation occurs in 15-20% of patients with blastomycosis.
-
Chest CT reveals a thick wall cavity in the left lower lobe with surrounding focal parenchymal disease; needle biopsy of this lesion confirmed blastomycosis. Cavitation occurs in 15-20% of patients with blastomycosis.
-
Chest radiograph from a patient with disseminated blastomycosis demonstrates diffuse miliary infiltrates associated with respiratory failure that required mechanical ventilation. In this patient, dense opacification with cavitation is seen in the right upper lobe. In a minority of patients, a diffuse micronodular pattern is seen; such a pattern results from hematogenous spread of the disease.
-
Chest radiograph from a patient with blastomycosis reveals left hilar lymphadenopathy, an uncommon finding in patients with blastomycosis.






