Practice Essentials
Vesicoureteral reflux (VUR) is the abnormal flow of urine from the bladder into the upper urinary tract and the most common urologic disease in childhood. Its presence is pathologic, and it represents the most significant risk factor for childhood renal scarring and its sequelae. For many years, the emphasis on the investigation of the child with UTI has centered on diagnosis of VUR. Some authors have suggested that the focus should be on whether the child has renal scarring or is at risk for renal scarring. The natural tendency for VUR to resolve spontaneously during childhood warrants initial medical management of most patients with low-grade reflux. There is a documented association of VUR with congenital upper urinary tract abnormalities such as renal agenesis, multicystic dysplastic kidney, and obstruction of the ureteropelvic junction (UPJ). [1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12]
VUR is graded by the International Reflux Grading System (IRGS), which classifies VUR into 5 grades [13, 14, 15] :
-
Grade I: Reflux into ureter
-
Grade II: Reflux into non-dilated renal pelvis
-
Grade III: Reflux into mildly dilated renal pelvis
-
Grade IV: Reflux into moderately dilated renal pelvis
-
Grade V: Reflux into severely dilated renal pelvis with tortuous ureter
The majority of cases (90%) in children represent a primary congenital failure of the natural passive 1-way mechanism of the ureterovesical junction (UVJ) to maintain unidirectional urine flow. A minority of VUR cases (10%) occur secondary to abnormalities of the ureteral insertion in association with renal transplantation, ureterocele, ureteral duplication anomalies, obstruction of the bladder outlet (posterior urethral valves in boys), dysfunctional voiding, or constipation.
The average patient age at diagnosis is 2-3 years. With the advent of prenatal sonographic screening, the evaluation for hydronephrosis and possible contribution of VUR is being performed in neonates and infants. Most cases of VUR resolve by about 8 years of age, depending on the grade.
(See the images of vesicoureteral reflux below.)
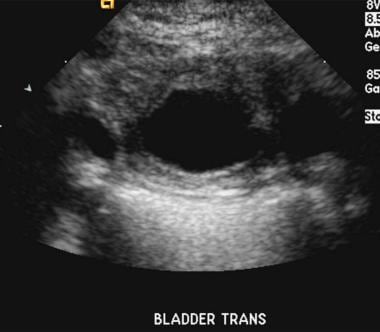
 Transverse gray-scale sonogram demonstrates a small left ureterocele in a patient with a low-grade vesicoureteral reflux. Ultrasonography may be the most helpful means to evaluate a patient for a ureterocele, as this is often difficult to visualize on early filling of the bladder during voiding cystourethrography. Patients with gross anatomic abnormalities of the urinary tract are not likely to improve without corrective surgery. In this case, the ureterocele measured less than 1 cm in all dimensions and appeared intermittently throughout the examination.
Transverse gray-scale sonogram demonstrates a small left ureterocele in a patient with a low-grade vesicoureteral reflux. Ultrasonography may be the most helpful means to evaluate a patient for a ureterocele, as this is often difficult to visualize on early filling of the bladder during voiding cystourethrography. Patients with gross anatomic abnormalities of the urinary tract are not likely to improve without corrective surgery. In this case, the ureterocele measured less than 1 cm in all dimensions and appeared intermittently throughout the examination.
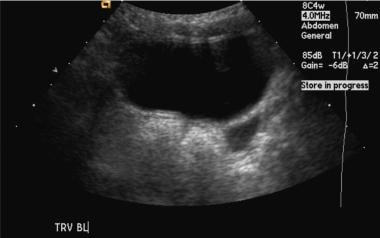
 Sonogram of a large, obstructing ureterocele in a patient with vesicoureteral reflux. The thin rim of the ureterocele is best noted on the inferior most aspect of the bladder. This ureterocele measured 4 cm in greatest dimension and is outlined by contrast material in Image 4. Note the dilated, left-sided refluxing ureter.
Sonogram of a large, obstructing ureterocele in a patient with vesicoureteral reflux. The thin rim of the ureterocele is best noted on the inferior most aspect of the bladder. This ureterocele measured 4 cm in greatest dimension and is outlined by contrast material in Image 4. Note the dilated, left-sided refluxing ureter.
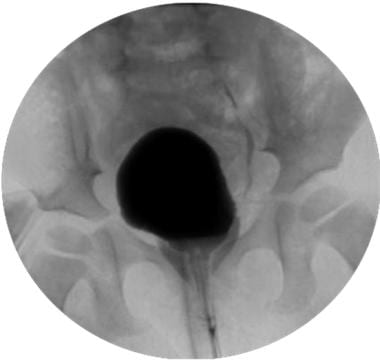
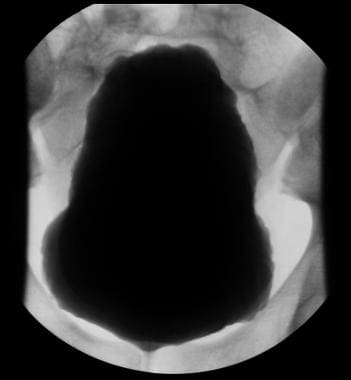
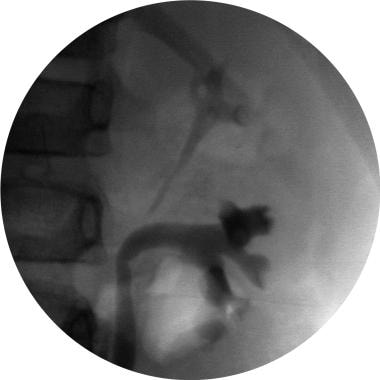
 Voiding cystourethrogram (VCUG) demonstrates a large, smooth, central filling defect peripherally outlined by contrast material. The catheter is deviated to the patient's right. This finding is consistent with a large ureterocele.
Voiding cystourethrogram (VCUG) demonstrates a large, smooth, central filling defect peripherally outlined by contrast material. The catheter is deviated to the patient's right. This finding is consistent with a large ureterocele.
 Voiding cystourethrogram (VCUG) show a large, distended bladder with irregular and trabeculated margins. This patient had posterior urethral valves.
Voiding cystourethrogram (VCUG) show a large, distended bladder with irregular and trabeculated margins. This patient had posterior urethral valves.
Preferred examination
Voiding cystourethrography (VCUG) is the screening urologic imaging study of choice. American urologists, pediatricians, and radiologists recommend this study to detect vesicoureteral reflux (VUR), ureterocele, posterior urethral valves in boys, or bladder wall thickening. [16, 17, 18] Up to 50% of children with proven urinary tract infection (UTI) undergoing VCUG have some degree of reflux. Sonography of the kidneys should be performed in conjunction with VCUG to document the size of the kidneys and to look for obstruction, hydronephrosis, or other congenital malformations. [9, 19, 20, 21] When VUR is found to distend the upper tract, postvoiding decompression at the upper tracts should be observed.
Reflux is generally intermittent and may escape detection on VCUG. This difficulty may be compounded by the desire to limit the child's exposure to ionizing radiation as much as possible. The influence of body position on the occurrence and detection of reflux has not been well studied in children. Incomplete bladder filling decreases the sensitivity of the study.
The results of sonographic evaluation for hydronephrosis or pelvicaliceal dilatation may vary greatly between the second and third trimesters. Abnormalities may not be detectable until the third trimester, later than the common second trimester screening examination.
In the prenatal period, VUR is detected more frequently in boys than in girls, with a male-to-female ratio of 5 to 1. Low-grade reflux is often associated with other prenatal urologic abnormalities. Mild pelviectasis is seen in 0.5-1% of all pregnancies. The widespread use of prenatal sonography has produced a marked increase in the early detection of urinary tract pathology in infants. The most common conditions identified are hydronephrosis and hydroureteronephrosis. Hydronephrosis is most often transient, but primary VUR is found in 10-40% of prenatally detected cases of hydronephrosis.
With the advent of prenatal sonographic screening, the evaluation for hydronephrosis, and subsequently VUR, is being performed in the neonatal period. The neonate with sonographic signs of renal pathology and possible reflux should be given prophylactic antibiotics and undergo VCUG. The risk of renal scarring from neonatal and infant reflux of infected urine is too great to ignore. [22, 23, 24, 25, 26, 27]
A study of 231 children ages 0-24 months with first time febrile UTI compared clinical, laboratory and ultrasonography findings between children with grades IV-V VUR (high‐grade VUR) and those with no or grades I-III VUR (normal or low‐grade VUR). Poor clinical appearance, presence of a uropathogen other than Escherichia coli, positive blood culture, hydroureter, and thickened renal pelvic wall were all independently associated with high‐grade VUR. The investigators concluded that if none of these 5 factors are present, VCUG is not necessary to detect high‐grade VUR; however, when more than one factor is present, VCUG is indicated. [28]
The principal techniques used in the evaluation of the renal impact of VUR include dimercaptosuccinic acid (DMSA) scanning and renal ultrasound because of their lack of need for sedation or catheterization. A patient receives a DMSA scan shortly after a UTI episode, and if abnormalities are present, VCUG is performed. [29]
Contrast-enhanced voiding urosonography (ceVUS) is an ultrasound technique that uses microbubbles to detect vesicoureteral reflux. The main benefit of ceVUS compared with VCUG is the absence of ionizing radiation, allowing it to be used for both screening and follow-up in pediatric patients. Studies have demonstrated that detection of vesicoureteral reflux ceVUS is on par with conventional VCUG. [30, 31, 32, 33, 34, 35, 36]
In ceVUS, an ultrasound contrast agent is administered intravesically via the urinary catheter, followed by continuous, alternate examination of the kidneys, urinary bladder, and retrovesical region during filling and voiding phases, as well as the urethra via transperineal or interscrotal approach during voiding phase. The diagnosis of VUR is determined by the movement of echogenic microbubbles from the contrast material during ultrasound examination of the upper urinary tract. The grading system used is as follows [30] :
-
Grade I: Microbubbles only in the ureter
-
Grade II: Microbubbles in the renal pelvis; no significant renal pelvic dilation
-
Grade III: Microbubbles in the renal pelvis + significant renal pelvic dilation + moderate calyceal dilatation
-
Grade IV: Microbubbles in the renal pelvis + significant renal pelvic dilation + significant calyceal dilatation
-
Grade V: Microbubbles in the renal pelvis + significant renal pelvic dilation and calyceal dilatation + loss of renal pelvis contour + dilated tortuous ureters
Fluoroscopically captured spot images
According to Fefferman et al, fluoroscopically captured images are adequate in documenting the absence of vesicoureteral reflux on VCUG examinations, making radiographic spot images unnecessary and thereby reducing patient exposure to radiation. The diagnostic accuracy of the fluoroscopically captured spot (FCS) images regarding binary characterization of reflux as negative or positive was 97.2%; the sensitivity of the FCS images was 92.6%; and the specificity of the FCS images was 98.6%. [3]
Screening
Menezes and Puri, in a study of 251 siblings of 215 index patients with grade III to V VUR, noted that the familial nature of VUR is well recognized but that the screening of siblings for VUR remains controversial. In their study, the authors found that the incidence of sibling VUR is maximal in patients younger than 3 years and that reflux in these patients is usually high grade and associated with a higher incidence of renal scarring. The authors recommended that screening be performed on all siblings who are younger than 3 years of index patients with grades III to V VUR. [5]
Renal scarring
Radiologic evidence of renal scarring is present in 30-60% of children with VUR, and VUR is present in almost all children (97%) with severe renal scarring. However, most kidneys (60%) with acute cortical defects do not demonstrate reflux, which highlights that ascending urinary tract infection is quite common despite the absence of demonstrated VUR.
The kidney is most susceptible to scarring from intrarenal reflux in the first year of life and probably at the time of first upper tract infection. [7] Renal scars less frequently develop after 5 years of age. New renal scars develop almost exclusively in the presence of UTI and intrarenal reflux, but the presence of intrarenal reflux alone does not equate with renal scarring. Infected urine is believed to cause an exudative reaction that leads to fibrosis and scarring of papillae. Intrarenal reflux is a phenomenon that is likely underreported because of its fleeting nature and occurrence at peak reflux.
Radiography
The diagnosis of vesicoureteral reflux (VUR) is accurately established with fluoroscopic voiding cystourethrography (VCUG). This study permits assessment for the presence and extent of reflux, and it clearly delineates the bladder outline, bladder neck, and ureteral and urethral anatomy. Fluoroscopic VCUG also gives an accurate estimation of bladder capacity.
The retention of contrast material within the upper tracts after voiding without decompression suggests UPJ or ureterovesical junction (UVJ) obstruction. VUR may occur with bladder filling, during voiding, or both. Cyclical VCUG, repeated bladder filling and fluoroscopic examination, which is primarily performed in patients younger than 1 year, depicts reflux an additional 10% of the time.
In children older than 3-4 years who have signs only of lower UTI, VCUG is not recommended if renal sonograms are normal. Whether VCUG is done while the initial UTI is being treated or several weeks afterward is not important, as long as the child is responding appropriately to treatment and has normal bladder function. VCUG may be performed as soon as the urine is sterile and bladder irritability has disappeared.
VUR is graded according to the International Reflux Classification outlined by the International Reflux Study Group. [37, 38] This classification scheme is widely accepted and shown below:
-
Grade III - Reflux into the collecting system with mild dilatation, slight ureteral tortuosity, and no or slight blunting of the fornices (see the images below)
 Voiding cystourethrogram (VCUG) demonstrates grade II VUR into the upper-pole moiety of a duplex collecting system and grade III VUR to the lower-pole moiety.
Voiding cystourethrogram (VCUG) demonstrates grade II VUR into the upper-pole moiety of a duplex collecting system and grade III VUR to the lower-pole moiety.
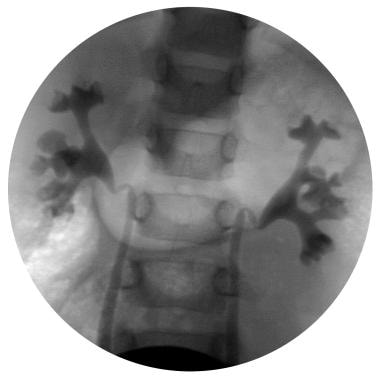
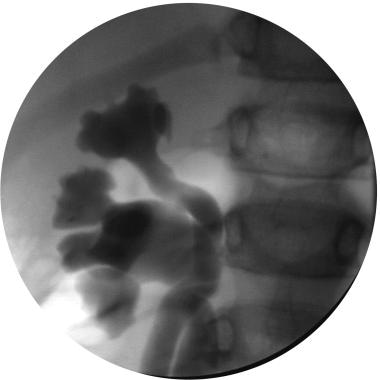
 Voiding cystourethrogram (VCUG) demonstrates bilateral grade III reflux. The renal pelvis is mildly dilated on the right. There is some mild blunting of the calyceal fornices and loss of papillary impressions in the upper poles bilaterally.
Voiding cystourethrogram (VCUG) demonstrates bilateral grade III reflux. The renal pelvis is mildly dilated on the right. There is some mild blunting of the calyceal fornices and loss of papillary impressions in the upper poles bilaterally.
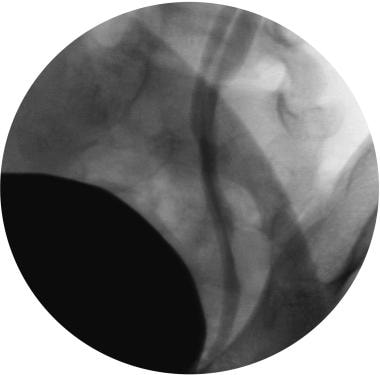
 Voiding cystourethrogram (VCUG) of lower ureter and ureterovesical junction in a patient with grade III reflux. The ureteral insertion on the left is between the 3- and 6-o'clock positions. There is a small bladder diverticulum at the ureteral insertion.
Voiding cystourethrogram (VCUG) of lower ureter and ureterovesical junction in a patient with grade III reflux. The ureteral insertion on the left is between the 3- and 6-o'clock positions. There is a small bladder diverticulum at the ureteral insertion.
-
Grade IV - Moderate dilatation and/or tortuosity of the ureter and moderate dilatation of the renal pelvis and calyces, with complete obliteration of the sharp angle of the fornices but maintenance of the papillary impressions in the majority of calyces (see the image below).
-
Grade V - Gross dilatation and tortuosity of the ureter, with gross dilatation of the renal pelvis and calyces and nonmaintained papillary impressions (see the images below).
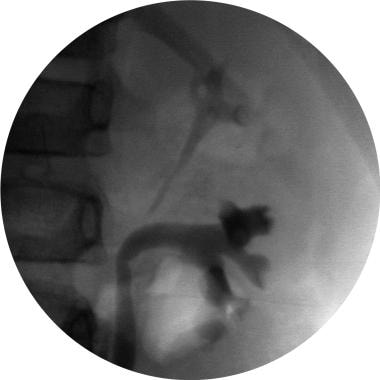
 Voiding cystourethrogram (VCUG) demonstrates a tortuous, dilated ureter in a patient with grade V vesicoureteral reflux.
Voiding cystourethrogram (VCUG) demonstrates a tortuous, dilated ureter in a patient with grade V vesicoureteral reflux.
Intrarenal reflux appears as contrast medium extending from the calyces into the polar renal collecting tubules in the form of striations. This can be identified most often in neonates and infants with moderate or severe reflux (5-15%). The presence of intrarenal reflux does not change the grade or treatment of VUR.
Nuclear imaging and sonography have replaced excretory urography (EU) as the preferred radiologic examination of the upper urinary tract. EU can demonstrate renal scarring but is less sensitive than DMSA or GH scintigraphy. The use of EU is exceptional and indicated only in those cases presenting with confusing collecting system anatomy or where demonstration of the calyces is important.
On excretory urograms, the scars of reflux nephropathy are typically detected about 2 years after infection. When uncomplicated, they have characteristic imaging features that include a deformed (clubbed) calyx and thinning of the overlying renal parenchyma, often with a notch in the surface of the kidney immediately opposite the affected calyx. Ureteral dilatation suggesting VUR may also be seen.
Computed Tomography
Although CT can provide excellent anatomic and functional information in children with reflux nephropathy, it does not have a primary role in the usual diagnostic algorithm or follow-up of such children. Still, hydronephrosis and ureteral dilatation are easily seen in patients with vesicoureteral reflux (VUR) who happen to undergo CT examination. At times in severe pyelonephritis, CT with intravenous contrast enhancement may be helpful in assessing for intrarenal suppuration and extrarenal extension of infection.
(See the images below.)
 Nonenhanced CT scan at a level just above ureteral insertion demonstrates bilateral, markedly dilated ureters in a patient with grade V vesicoureteral reflux.
Nonenhanced CT scan at a level just above ureteral insertion demonstrates bilateral, markedly dilated ureters in a patient with grade V vesicoureteral reflux.
 Nonenhanced CT scan in a 12-year-old boy demonstrates marked hydronephrosis and cortical thinning in a patient with grade V vesicoureteral reflux and a history of a posterior urethral valve. Note the free fluid in the pararenal space consistent with forniceal rupture after minor trauma to the abdomen (from football practice).
Nonenhanced CT scan in a 12-year-old boy demonstrates marked hydronephrosis and cortical thinning in a patient with grade V vesicoureteral reflux and a history of a posterior urethral valve. Note the free fluid in the pararenal space consistent with forniceal rupture after minor trauma to the abdomen (from football practice).
Ultrasonography
The widespread use of prenatal sonography has produced a marked increase in the early detection of urinary tract pathology in infants. The most common conditions identified are hydronephrosis and hydroureteronephrosis. Hydronephrosis is most often transient, but primary VUR is found in 10-40% of prenatally detected cases of hydronephrosis. [19, 39, 24]
Ultrasonography is best used in conjunction with screening VCUG to assess for renal size; upper tract abnormalities, such as hydronephrosis and ureteral dilatation; obvious scarring; ureteral ectopia or bladder abnormalities, such as ureterocele; and bladder wall thickening.
Contrast-enhanced voiding urosonography (ceVUS) is an ultrasound technique that uses microbubbles to detect vesicoureteral reflux. The main benefit of ceVUS compared with VCUG is the absence of ionizing radiation, allowing it to be used for both screening and follow-up in pediatric patients. Studies have demonstrated that detection of vesicoureteral reflux ceVUS is on par with conventional VCUG. [30, 31, 32, 33, 34, 35, 36]
In ceVUS, an ultrasound contrast agent is administered intravesically via the urinary catheter, followed by continuous, alternate examination of the kidneys, urinary bladder, and retrovesical region during filling and voiding phases, as well as the urethra via transperineal or interscrotal approach during voiding phase. The diagnosis of VUR is determined by the movement of echogenic microbubbles from the contrast material during ultrasound examination of the upper urinary tract. The grading system used is as follows [30] :
-
Grade I: Microbubbles only in the ureter
-
Grade II: Microbubbles in the renal pelvis; no significant renal pelvic dilation
-
Grade III: Microbubbles in the renal pelvis + significant renal pelvic dilation + moderate calyceal dilatation
-
Grade IV: Microbubbles in the renal pelvis + significant renal pelvic dilation + significant calyceal dilatation
-
Grade V: Microbubbles in the renal pelvis + significant renal pelvic dilation and calyceal dilatation + loss of renal pelvis contour + dilated tortuous ureters
(See the images below.)
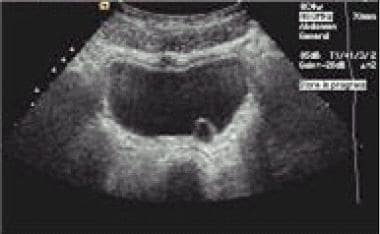
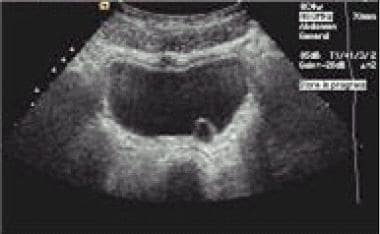 Transverse gray-scale sonogram demonstrates a small left ureterocele in a patient with a low-grade vesicoureteral reflux. Ultrasonography may be the most helpful means to evaluate a patient for a ureterocele, as this is often difficult to visualize on early filling of the bladder during voiding cystourethrography. Patients with gross anatomic abnormalities of the urinary tract are not likely to improve without corrective surgery. In this case, the ureterocele measured less than 1 cm in all dimensions and appeared intermittently throughout the examination.
Transverse gray-scale sonogram demonstrates a small left ureterocele in a patient with a low-grade vesicoureteral reflux. Ultrasonography may be the most helpful means to evaluate a patient for a ureterocele, as this is often difficult to visualize on early filling of the bladder during voiding cystourethrography. Patients with gross anatomic abnormalities of the urinary tract are not likely to improve without corrective surgery. In this case, the ureterocele measured less than 1 cm in all dimensions and appeared intermittently throughout the examination.
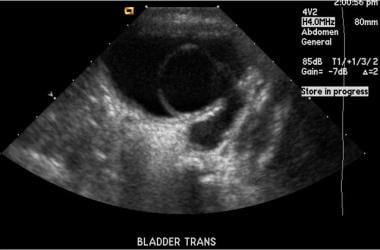
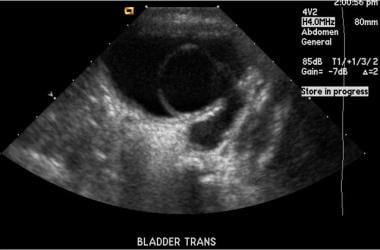 Sonogram of a large, obstructing ureterocele in a patient with vesicoureteral reflux. The thin rim of the ureterocele is best noted on the inferior most aspect of the bladder. This ureterocele measured 4 cm in greatest dimension and is outlined by contrast material in Image 4. Note the dilated, left-sided refluxing ureter.
Sonogram of a large, obstructing ureterocele in a patient with vesicoureteral reflux. The thin rim of the ureterocele is best noted on the inferior most aspect of the bladder. This ureterocele measured 4 cm in greatest dimension and is outlined by contrast material in Image 4. Note the dilated, left-sided refluxing ureter.
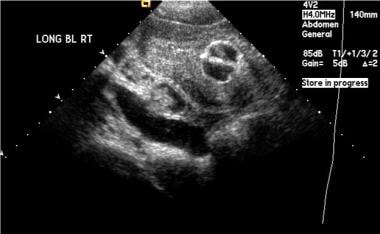
 Longitudinal sonogram corresponding to a voiding cystourethrogram (VCUG) of a grade III vesicoureteral reflux. Note the mild pelviectasis. The degree of pelviectasis or caliectasis does not correlate with the degree of reflux seen on the VCUG.
Longitudinal sonogram corresponding to a voiding cystourethrogram (VCUG) of a grade III vesicoureteral reflux. Note the mild pelviectasis. The degree of pelviectasis or caliectasis does not correlate with the degree of reflux seen on the VCUG.
 Sagittal sonogram of the bladder. A Foley catheter is surrounded by thickened, hypertrophied bladder wall, the sequelae of posterior urethral valves in this boy with bilateral grade V vesicoureteral reflux. Note the dilated right ureter.
Sagittal sonogram of the bladder. A Foley catheter is surrounded by thickened, hypertrophied bladder wall, the sequelae of posterior urethral valves in this boy with bilateral grade V vesicoureteral reflux. Note the dilated right ureter.
 Transverse sonogram in a boy with grade V vesicoureteral reflux and posterior urethral valves. Image demonstrates a thickened bladder wall.
Transverse sonogram in a boy with grade V vesicoureteral reflux and posterior urethral valves. Image demonstrates a thickened bladder wall.
 Renal sonogram in a patient with high-grade vesicoureteral reflux secondary to a posterior urethral valve demonstrates moderate hydronephrosis and cortical thinning.
Renal sonogram in a patient with high-grade vesicoureteral reflux secondary to a posterior urethral valve demonstrates moderate hydronephrosis and cortical thinning.
 Sonogram of the right kidney in a patient with grade V vesicoureteral reflux. Hydronephrosis and increased echogenicity indicating renal dysplasia secondary to reflux nephropathy. This kidney measured 6.7 cm, while the left one measured 8.3 cm.
Sonogram of the right kidney in a patient with grade V vesicoureteral reflux. Hydronephrosis and increased echogenicity indicating renal dysplasia secondary to reflux nephropathy. This kidney measured 6.7 cm, while the left one measured 8.3 cm.
 Transverse sonogram of the bladder demonstrates left ureteral dilatation near the level of the ureteral insertion.
Transverse sonogram of the bladder demonstrates left ureteral dilatation near the level of the ureteral insertion.
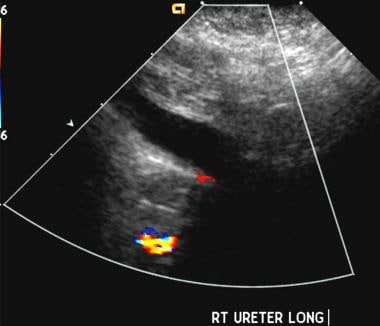 Longitudinal sonogram demonstrates dilatation of the mid aspect of the ureter. The ureter could be visualized in its entirety and was dilated throughout.
Longitudinal sonogram demonstrates dilatation of the mid aspect of the ureter. The ureter could be visualized in its entirety and was dilated throughout.
 Longitudinal sonogram of the left kidney in a patient with grade V vesicoureteral reflux and a duplex collecting system. There is hydronephrosis of the lower pole moiety and dilatation of the proximal ureter. The upper pole of the kidney was normal on ultrasonography and did not demonstrate reflux on voiding cystourethrography (VCUG).
Longitudinal sonogram of the left kidney in a patient with grade V vesicoureteral reflux and a duplex collecting system. There is hydronephrosis of the lower pole moiety and dilatation of the proximal ureter. The upper pole of the kidney was normal on ultrasonography and did not demonstrate reflux on voiding cystourethrography (VCUG).
Prenatally detected primary vesicoureteral reflux is found in males (male-to-female ratio, 5:1) most of whom have bilateral high-grade reflux. [10] Low-grade reflux is often associated with other prenatal urologic abnormalities. Mild pelviectasis is seen in 0.5-1% of all pregnancies. The significance of mild pelvic and/or pelvicaliceal dilatation as a marker of VUR is poorly validated, but dilatation beyond 15 mm has proven to be significant and should prompt a thorough search for other urologic abnormalities.
The neonate with sonographic signs of renal pathology and possible reflux should be given prophylactic antibiotics and examined with voiding cystourethrography (VCUG). The risk of renal scarring from neonatal and infant pyelonephritis is too great to ignore.
Generally speaking, ultrasonography is an unreliable modality for the detection of VUR. It cannot be used as the sole means to exclude clinically significant VUR, even when the results are normal. Nevertheless, clues to the presence of VUR can be inferred from certain sonographic findings—namely, complete duplication, peristaltic ureteral dilatation, and calyceal dilatation. Sonographic measurement of kidney size is an important aspect of the screening examination. An abnormally small kidney in the child suggests parenchymal thinning, even in the absence of visible scar.
Obtaining reproducible sonograms is highly operator dependent. Full assessment of the bladder and urethra can sometimes be difficult. Smaller scars are less well visualized with sonography than with technetium-99m dimercaptosuccinic acid (DMSA) or glucoheptonate (GH) cortical scanning.
Sonography has been proposed for follow-up of patients with reflux or for detecting reflux in siblings. New techniques involve instilling carbonated solutions or sonicated albumin into the bladder. The false-negative rate associated with this procedure is high, and it is not recommended as a routine test for VUR.
Approximately 74% of kidneys with reflux at VCUG are normal on sonograms obtained on the same day, and approximately 25% of the refluxing kidneys that are missed have reflux of grade III or worse.
The results of sonographic evaluation for hydronephrosis or pelvicaliceal dilatation may vary greatly between the second and third trimesters. Abnormalities may not be detectable until the third trimester, later than the common second trimester screening examination.
Nuclear Imaging
Direct radionuclide cystography with a 99mTc-labeled agent (sulfur colloid, diethylenetriamine penta-acetate [DTPA], or pertechnetate) is a well-accepted alternative to fluoroscopic VCUG for screening asymptomatic siblings or offspring, for follow-up examination of children with vesicoureteral reflux (VUR), for postoperative evaluation after ureteral reimplantation, and for excluding VUR when it is not seriously considered (especially in girls).
Direct radionuclide cystography is more sensitive than VCUG. It can depict as little as 1 mL of refluxed urine. Grade I reflux affects the ureter only, grade II reflux involves the kidney with no pelvic dilatation, and grade III reflux is reflux with pelvic dilatation. Renal cortical scintigraphy demonstrates twice as many scars as sonography and 4 times as many scars as EU.
The advantages of this study include continuous monitoring and imaging, high sensitivity, and a decreased radiation dose for a voiding imaging study. The dose to the pelvic organs was significantly lower when the study was popularized in the screen film cassette spot film era of former fluoroscopic equipment. With modern digital fluoroscopy units that reduce dose by pulsed fluoroscopy or other dose reduction strategy combined with video frame grabbing spot images, the dose reduction advantage of the isotope cystogram is only marginal.
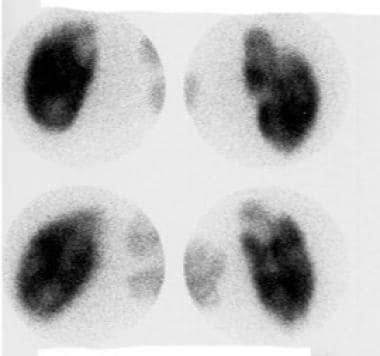
Patients with VUR are typically followed up with serial radionuclide cystography every 12-24 months (see the image below). The International Classification of Reflux is not commonly applied to radionuclide studies, but the amount of activity that appears in the upper urinary tracts can be quantified into 1 of 3 levels of severity and used as a basis of comparison in serial follow-up examinations.
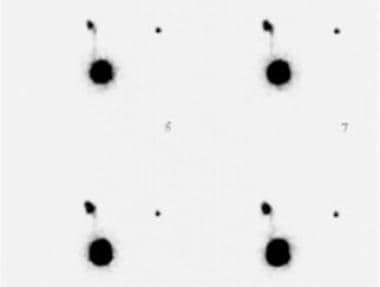 Nuclear cystograms demonstrate grade III reflux. Reflux to the left kidney is shown, with dilatation of the renal pelvis.
Nuclear cystograms demonstrate grade III reflux. Reflux to the left kidney is shown, with dilatation of the renal pelvis.
The indirect radionuclide cystogram (no catheterization) using 99mTc mercaptoacetyltriglycine (MAG3) can be performed in the toilet-trained child, but its specificity is decreased. [40] It is not recommended as a routine screening procedure for evaluating VUR.
The most accurate evaluation of renal scarring and renal function is performed with intravenously injected 99mTc DMSA or GH. DMSA (see the image below) accumulates in the distal tubular cells and provides excellent visualization of the renal cortex, correlating with histopathologic findings in 95% of experimental animals. [41, 42]
 Dimercaptosuccinic acid (DMSA) scans demonstrate photopenia at the right superior pole consistent with scarring in this patient with vesicoureteral reflux.
Dimercaptosuccinic acid (DMSA) scans demonstrate photopenia at the right superior pole consistent with scarring in this patient with vesicoureteral reflux.
Single photon emission computed tomography (SPECT) is superior to planar imaging techniques, especially in children younger than 3 years. Renal scars detected with DMSA scintigraphy appear as focal or generalized areas of diminished radioisotope uptake associated with loss or contraction of functioning renal cortex. This may appear as thinning or flattening of the cortex in some kidneys, while in others renal scars appear as classic discrete wedge-shaped parenchymal defects.
About 63-75% of patients with acute inflammatory changes on the initial DMSA renal scans do not have VUR, and reflux is present in only 25-50% of kidneys that develop new renal scarring. Although not a prerequisite for acquired renal scarring, VUR is still a risk factor that cannot be discounted and should be evaluated.
If a DMSA or GH study is being performed to detect reflux nephropathy with scar formation, it should be undertaken at least 6 months after a documented UTI because an upper tract infection causes an abnormal appearance on DMSA or GH scans. Abnormalities resulting from infection are transient, whereas scars result in a permanent abnormality.
In the setting of acute infection, granulocyte aggregation, complement activation, and compression of the renal microcirculation from interstitial edema cause ischemia. Overall, the effect is of reduced regional blood flow and radiotracer uptake. Although this may be a transient phenomenon, it cannot be distinguished from scarring in the acute setting.
Balestraci et al performed a retrospective study of late DMSA renal scans in identifying high-grade (III-V) VUR in children older than 3 years with a febrile UTI history that was not timely investigated. They found that the normal late DMSA scan predicted the absence of high-grade VUR, potentially obviating the need for a VCUG. Sensitivity, specificity, negative predictive values, and positive predictive values of late DMSA scans for all grades of VUR were 93.1%, 75%, 92.3% and 77.1%, respectively. [42]
-
Transverse gray-scale sonogram demonstrates a small left ureterocele in a patient with a low-grade vesicoureteral reflux. Ultrasonography may be the most helpful means to evaluate a patient for a ureterocele, as this is often difficult to visualize on early filling of the bladder during voiding cystourethrography. Patients with gross anatomic abnormalities of the urinary tract are not likely to improve without corrective surgery. In this case, the ureterocele measured less than 1 cm in all dimensions and appeared intermittently throughout the examination.
-
Sonogram of a large, obstructing ureterocele in a patient with vesicoureteral reflux. The thin rim of the ureterocele is best noted on the inferior most aspect of the bladder. This ureterocele measured 4 cm in greatest dimension and is outlined by contrast material in Image 4. Note the dilated, left-sided refluxing ureter.
-
Voiding cystourethrogram (VCUG) demonstrates a large, smooth, central filling defect peripherally outlined by contrast material. The catheter is deviated to the patient's right. This finding is consistent with a large ureterocele.
-
Excretory urogram demonstrates the classic cobra-head appearance of a ureterocele.
-
Voiding cystourethrogram (VCUG) demonstrates a posterior urethral valve.
-
Voiding cystourethrogram (VCUG) shows grade I left VUR. Incidentally noted is vaginal reflux.
-
Voiding cystourethrogram (VCUG) demonstrates grade II VUR into the upper-pole moiety of a duplex collecting system and grade III VUR to the lower-pole moiety.
-
Grade II vesicoureteral reflux in a patient with ureteral duplication.
-
Voiding cystourethrogram (VCUG) demonstrates bilateral grade III reflux. The renal pelvis is mildly dilated on the right. There is some mild blunting of the calyceal fornices and loss of papillary impressions in the upper poles bilaterally.
-
Voiding cystourethrogram (VCUG) of lower ureter and ureterovesical junction in a patient with grade III reflux. The ureteral insertion on the left is between the 3- and 6-o'clock positions. There is a small bladder diverticulum at the ureteral insertion.
-
Voiding cystourethrogram (VCUG)demonstrates bilateral grade III vesicoureteral reflux.
-
Longitudinal sonogram corresponding to a voiding cystourethrogram (VCUG) of a grade III vesicoureteral reflux. Note the mild pelviectasis. The degree of pelviectasis or caliectasis does not correlate with the degree of reflux seen on the VCUG.
-
Voiding cystourethrogram (VCUG) demonstrates high-grade IV vesicoureteral reflux in a patient with a duplicated collecting system.
-
Grade III vesicoureteral reflux and periureteral-type diverticulum.
-
Voiding cystourethrogram (VCUG) of the left kidney demonstrates grade V vesicoureteral reflux.
-
Voiding cystourethrogram (VCUG) demonstrates a tortuous, dilated ureter in a patient with grade V vesicoureteral reflux.
-
Unilateral grade V vesicoureteral reflux secondary to a posterior urethral valve. There is gross dilatation of the renal pelvis and calyces. Papillary impressions are not visible. Gross intrarenal reflux is also identified.
-
Nuclear cystograms demonstrate grade III reflux. Reflux to the left kidney is shown, with dilatation of the renal pelvis.
-
Dimercaptosuccinic acid (DMSA) scans demonstrate photopenia at the right superior pole consistent with scarring in this patient with vesicoureteral reflux.
-
Nonenhanced CT scan at a level just above ureteral insertion demonstrates bilateral, markedly dilated ureters in a patient with grade V vesicoureteral reflux.
-
Nonenhanced CT scan in a 12-year-old boy demonstrates marked hydronephrosis and cortical thinning in a patient with grade V vesicoureteral reflux and a history of a posterior urethral valve. Note the free fluid in the pararenal space consistent with forniceal rupture after minor trauma to the abdomen (from football practice).
-
Sagittal sonogram of the bladder. A Foley catheter is surrounded by thickened, hypertrophied bladder wall, the sequelae of posterior urethral valves in this boy with bilateral grade V vesicoureteral reflux. Note the dilated right ureter.
-
Transverse sonogram in a boy with grade V vesicoureteral reflux and posterior urethral valves. Image demonstrates a thickened bladder wall.
-
Renal sonogram in a patient with high-grade vesicoureteral reflux secondary to a posterior urethral valve demonstrates moderate hydronephrosis and cortical thinning.
-
Sonogram of the right kidney in a patient with grade V vesicoureteral reflux. Hydronephrosis and increased echogenicity indicating renal dysplasia secondary to reflux nephropathy. This kidney measured 6.7 cm, while the left one measured 8.3 cm.
-
Transverse sonogram of the bladder demonstrates left ureteral dilatation near the level of the ureteral insertion.
-
Longitudinal sonogram demonstrates dilatation of the mid aspect of the ureter. The ureter could be visualized in its entirety and was dilated throughout.
-
Longitudinal sonogram of the left kidney in a patient with grade V vesicoureteral reflux and a duplex collecting system. There is hydronephrosis of the lower pole moiety and dilatation of the proximal ureter. The upper pole of the kidney was normal on ultrasonography and did not demonstrate reflux on voiding cystourethrography (VCUG).
-
Voiding cystourethrogram (VCUG) show a large, distended bladder with irregular and trabeculated margins. This patient had posterior urethral valves.
-
Excretory urogram demonstrates the position of surgically reimplanted ureters after correction of vesicoureteral reflux.
-
Vesicoureteral reflux assessment and treatment algorithm.