Practice Essentials
Urolithiasis is a common disease estimated to affect 11% of men and 7% of women in their lifetime. More than 1 million patients with suspected urolithiasis present to an emergency department (ED) each year in the United States. [1] Ureterolithiasis causes severe, unilateral, colicky flank pain and patients usually present within hours of onset. The pain may radiate from the flank anteromedially toward the groin and into the genitals and may be accompanied by nausea, vomiting, and hematuria. [2] Passage of a urinary stone is the single most common cause of acute ureteral obstruction and affects as many as 12% of the population. The pain may be some of the most severe pain that humans experience and complications of stone disease may result in severe infection, renal failure, or in rare cases, death. [3]
Preferred examination
The goals of imaging of urinary calculi are to determine the presence of stones witin the urinary tract, evaluate for complications, estimate the likelihood of stone passage, confirm stone passage, assess the stone burden, and evaluate disease activity. [4] Computed tomography (CT) imaging is now performed in more than 70% of patients receiving a diagnosis of ureterolithiasis. Often, conventional radiography is initially used to screen for stones, bowel abnormalities, or free intra-abdominal air. Radiographs can also be used to monitor the passage of visible stones after a diagnosis is made.
When CT is available, it is now considered the examination of choice for the detection and localization of urinary stones. Almost all studies conducted to date show that Intravenous urography (IVU) provides no additional clinically important information after noncontrast computed tomography (NCCT) is performed. As a result of the higher radiation dose of CT, conventional or digital radiography can be used to monitor the passage of stones if radiographic follow-up studies are indicated and if the stone is visible on conventional radiographs. [5, 6, 7]
Because of the higher radiation dose with CT, conventional or digital radiography should be used to monitor the passage of stones if radiographic follow-up is indicated and if the stone is visible on conventional radiographs. Pregnant or pediatric patients may be imaged with ultrasound (US) first to avoid radiation exposure. The rare false-negative finding can be due to reader error or a protease-inhibitor CT-lucent stone. False-positive results are usually due to phleboliths adjacent to the ureter. In some cases, intravenous contrast material may be needed to opacify the ureter.
Intravenous urography (IVU) (excretory urography) provides important physiologic information regarding the degree of obstruction. It is the traditional examination for the assessment of urinary stone disease. The radiation dose is generally less than that of CT, but it is of the same order of magnitude. Intravenous contrast is required, with resultant risks of an allergic reaction or nephrotoxicity. IVU is less sensitive than CT, especially for small or nonobstructing stones.
(Images of stone disease are provided below.)
 Renal sonogram demonstrates an echogenic shadowing calculus in the renal collecting system with hydronephrosis.
Renal sonogram demonstrates an echogenic shadowing calculus in the renal collecting system with hydronephrosis.
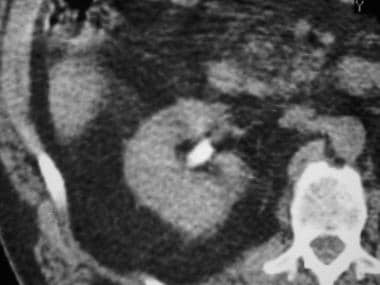
 Contrast-enhanced CT scan demonstrates an opaque staghorn calculus filling the left renal collecting system.
Contrast-enhanced CT scan demonstrates an opaque staghorn calculus filling the left renal collecting system.
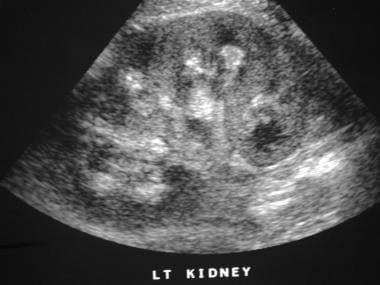 Renal longitudinal sonogram in a patient with nephrocalcinosis shows diffuse echogenic shadowing calcifications in the renal pyramids.
Renal longitudinal sonogram in a patient with nephrocalcinosis shows diffuse echogenic shadowing calcifications in the renal pyramids.
 Nonenhanced CT image shows an obstructing left proximal ureteral calculus with a slight soft-tissue rim around the stone (ie, rim sign).
Nonenhanced CT image shows an obstructing left proximal ureteral calculus with a slight soft-tissue rim around the stone (ie, rim sign).
Use of ultrasonography (US) for initial evaluation of suspected urinary calculi is common outside the United States. [8] US is useful in young or pregnant patients [9, 10] and in patients allergic to iodinated contrast material. US is also helpful in problem solving. Hydronephrosis, an indirect sign of an obstructing stone, can be identified on ultrasound and may correlate with stone size. [8]
US has limited sensitivity for smaller stones, and does not depict the ureters well. It should be used mainly in patients who are young, those who are pregnant, or those undergoing multiple examinations (eg, patients with spine injury).
Guidelines
The ACR guidelines for evaluation of acute onset flank pain with suspicion of urolithiasis include the following: [11]
-
Noncontrast computed tomography (NCCT) is the most accurate technique for evaluating flank pain.
-
Low-dose NCCT should be performed when evaluating for renal or ureteral stones.
-
If there is uncertainty about whether a calcific density represents a ureteral stone or a phlebolith, intravenous contrast material can be administered and excretory-phase images obtained for definitive diagnosis.
-
In pregnant patients with flank pain, ultrasonography is the best initial study.
-
Abdominal radiography combined with ultrasonography may be able to diagnose most clinically significant stones and should be considered, especially in young patients and those with known stone disease.
-
MRI could be considered to evaluate for hydronephrosis, although it is less accurate for the direct visualization of renal and ureteral stones.
The European Association of Urology (EAU) guidelines recommend that ultrasonography be used as the primary diagnostic imaging tool. The EAU notes that ultrasonography can identify stones located in the kidney and pyeloureteral and vesicoureteric junctions but that it frequently fails to detect ureteral calculi. The upper urinary tract is usually dilated in patients with ureteral stones. For all stones, US has a sensitivity of 19–93% and a specificity of 84–100%. Following thet initial ultrasound assessment, the EAU recommends that NCCT be performed to confirm stone diagnosis in patients with acute flank pain. [12]
Other key recommendations of the EAU include the following: [12]
-
If NCCT is indicated in patients with BMI < 30 kg/m2, a low-dose technique should be performed.
-
A contrast-enahnced study is recommended if stone removal is planned and the anatomy of the collecting system needs to be assessed; Contrast-enhanced CT is preferable because it enables 3D reconstruction of the collecting system. Intravenous urography may also be used.
-
For evaluation of pregnant women, ultrasonography is the imaging modality of choice; MRI may be used as a second-line imaging modality with low-dose CT restricted to select cases.
The STONE Score
The STONE score is a clinical prediction score for uncomplicated symptomatic stone that has been retrospectively derived and prospectively validated. Five factors are included, with points ranging from 0–3 for sex, timing (duration of pain from onset), origin (or race), nausea (or vomiting), and erythrocytes (presence of hematuria). A total score of 0 to 5 points is categorized as low risk (about 10%), 6 to 9 as moderate risk (about 50%), and 10 to 13 as high risk (about 90%). [13]
In an external validation, the sensitivity and specificity of a high score were 53% and 87%, with a 1.2% probability of important alternative diagnosis (upper 95% confidence interval [CI] of 3.6%). [14] Thus, the STONE score alone cannot rule in or rule out stones or exclude clinically important diagnoses. However, as further studies are conducted, it has the potential to be used as part of an algorithm for suspected urolithiasis that could reliably identify patients highly likely to have urolithiasis and may allow patients to be safely managed without imaging, or imaged with other approaches such as ultrasonography or reduced dose CT. [8, 15]
Radiography
Conventional radiography
Conventional radiography, as shown in the image below, is often performed as a preliminary examination in patients with abdominal pain possibly resulting from urinary calculi. These images should be obtained before contrast material is administered to prevent obscuring calcifications within the collecting system or calyceal diverticula. Conventional radiographs should include the entire urinary tract and two images are often required.
 Abdominal radiograph shows calcification filling the left collecting system. This finding is consistent with a staghorn calculus. For its size, the stone is relatively lucent.
Abdominal radiograph shows calcification filling the left collecting system. This finding is consistent with a staghorn calculus. For its size, the stone is relatively lucent.
Stones are often found at key points of narrowing such as the ureteropelvic junction (UPJ), the ureterovesical junction (UVJ), and the point at which the ureter crosses the iliac vessels. An additional site is on the right side, where the ureter passes through the root of the mesentery. Calcium stones as small as 1–2 mm can be seen. Cystine stones as small as 3–4 mm may be depicted, but uric acid stones are usually not seen unless they have become calcified.
Typically, phleboliths are round or oval, and they may demonstrate a central lucency. However, they are often difficult to distinguish from ureteral calculi. Phleboliths in the pelvis are usually located lower than and lateral to the ureter, but they overlap with the ureter. Because gonadal veins run parallel to the upper ureters, contrast enhancement may be needed to opacify the ureter and demonstrate the extraurinary location of phleboliths in the gonadal veins.
An erect or posterior oblique radiograph obtained on the side of the calcification may help distinguish urinary stones from extraurinary calcifications. This view can also depict calcifications that are projected over the sacrum or transverse processes on the frontal view.
Preinjection renal tomography may depict additional stones, and it can be used to confirm the relationship of stones to the kidneys.
Because stones are more visible with a lower peak kilovoltage (kVp), maintaining a maximum of 60–80 kVp is best, if possible. Larger patients may require a higher peak kilovoltage for acceptable exposure and scatter. In this situation, compression of the abdomen and collimation is critical.
Mild bowel preparation may be helpful for increasing the sensitivity of conventional radiography for small stones in patients undergoing screening or follow-up observation for stones.
Intravenous urography
Intravenous urography (IVU), as shown in the images below, is useful for confirming the exact location of a stone within the urinary tract. IVU depicts anatomic abnormalities such as dilated calyces, calyceal diverticula, duplication, UPJ obstruction, retrocaval ureter, and other findings that may predispose patients to stone formation or alter therapy. Because contrast agents can obscure stones in the collecting system, scouting the entire urinary tract prior to their administration is critical.
 Magnified scout intravenous urogram shows a large, relatively lucent calculus in the lower pole of the right kidney.
Magnified scout intravenous urogram shows a large, relatively lucent calculus in the lower pole of the right kidney.
 Intravenous urogram. After the intravenous injection, contrast material in the collecting system obscures the calculus.
Intravenous urogram. After the intravenous injection, contrast material in the collecting system obscures the calculus.
 Intravenous urogram obtained 5 minutes after the intravenous injection. Contrast material in the collecting system obscures the stone.
Intravenous urogram obtained 5 minutes after the intravenous injection. Contrast material in the collecting system obscures the stone.
When an acute urinary stone is the primary consideration, compression may not be used to increase sensitivity for detection of low-grade obstruction. A caveat is that the contralateral kidney may have an abnormality that requires ureteric compression for adequate examination. In rare cases, the use of compression has been associated with forniceal rupture.
When a stone causes acute obstruction, an obstructive nephrogram may be present. This may be prolonged and hyperdense, with increasing opacity over time. The nephrogram of acute obstruction is usually homogeneous, but it may also be striated or, occasionally, not be visible on radiographs. [16]
Other signs include delayed excretion, dilatation to the point of obstruction, or blunting of the calyceal fornices. Immediately after the passage of a stone, residual mild obstruction or edema can be detected at the UVJ. Delayed images may be needed to opacify to the point of the obstruction, but using gravity to position the more opaque and more distal contrast material–laden urine is also possible by placing the patient in a prone or erect position.
Extravasation of urine at the fornices may result in pyelosinus or pyelolymphatic extravasation, which is often first indicated by blurring of the calyceal fornices. Greater extravasation may outline the collecting system, and the contrast may dissect into the perinephric space; however, if the urine is not infected, this is usually clinically insignificant.
Degree of confidence
Although 90% of urinary calculi are radiodense on abdominal radiographs, the sensitivity for the prospective identification of individual stones is only 50–60%, and the specificity is only approximately 70%. Approximately 10% of stones are radiolucent on conventional radiographs.
Occasionally, false-positive findings result from extrarenal calcification, but these are usually correctly identified with IVU. Lucent stones appear as filling defects on IVU, but they are not distinguished from non–stone-filling defects such as transitional cell carcinomas or blood clots. US and CT are effective tools in making this distinction; however, much of the ureter cannot be visualized with US.
Computed Tomography
With a sensitivity of 94–97% and a specificity of 96–100%, helical CT is the most sensitive radiologic examination for the detection, localization, and characterization of urinary calcifications. Therefore, helical CT is considerably more effective than IVU. [11] Helical CT scans frequently depict nonobstructing stones that are missed on IVU. CT is faster and no contrast agent is needed in most patients.
CT easily differentiates between nonopaque stones and blood clots or tumors (compared with IVU, which may depict only a filling defect). In addition, helical CT is better than US or IVU in detecting other causes of abdominal pain. In most studies, IVU added little or no information. [17]
Rarely, pure matrix stones may demonstrate soft-tissue opacity on CT scans, and indinavir stones appear lucent. [18] However, all other stones appear opaque on CT scans. [5, 6, 7]
Individual CT signs are associated with varying degrees of confidence. False-positive results are almost exclusively the result of a phlebolith adjacent to the ureter. False-negative results are primarily due to indinavir radiolucent stones and error. CT scans often suggest an alternative or additional diagnosis when renal stone disease is clinically suspected. [19, 20]
Technique
Because stones in the collecting system may be obscured by contrast material, NCCT, as shown in the images below, is usually performed. [11] Helical CT is important to avoid missing stones because of section misregistration. A 5-mm helical technique with a pitch of 1.5:1 or less is preferred, although some radiologists choose to use a pitch of as much as 2:1. [21, 22, 23] The kidneys and, if possible, the entire abdomen should be scanned during a single breath-hold to prevent section misregistration. [24, 25, 26]
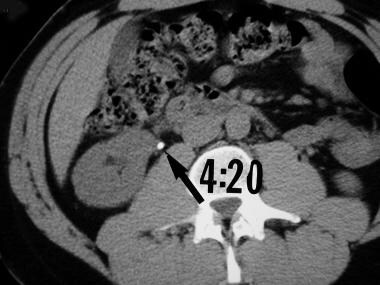 Axial nonenhanced CT section at the level of the kidney demonstrates an attenuating proximal ureteral calculus (arrow). No significant hydronephrosis is identified. CT can be performed much more rapidly than urography and without the use of intravenous contrast material.
Axial nonenhanced CT section at the level of the kidney demonstrates an attenuating proximal ureteral calculus (arrow). No significant hydronephrosis is identified. CT can be performed much more rapidly than urography and without the use of intravenous contrast material.
 Axial nonenhanced CT image at the level of the kidneys shows bilateral renal calculi, right hydronephrosis, and moderate perinephric fluid.
Axial nonenhanced CT image at the level of the kidneys shows bilateral renal calculi, right hydronephrosis, and moderate perinephric fluid.
 Axial nonenhanced CT image of the urinary bladder demonstrates an attenuating calculus at the right ureteropelvic junction.
Axial nonenhanced CT image of the urinary bladder demonstrates an attenuating calculus at the right ureteropelvic junction.
 Nonenhanced CT image of the pelvis shows dilatation of the distal left ureter and mild periureteral fluid near the left ureterovesical junction.
Nonenhanced CT image of the pelvis shows dilatation of the distal left ureter and mild periureteral fluid near the left ureterovesical junction.
 Nonenhanced CT image of the pelvis shows a small attenuating stone at the left ureterovesical junction.
Nonenhanced CT image of the pelvis shows a small attenuating stone at the left ureterovesical junction.
Because patients with stones are often young and because stone disease may recur, minimizing the radiation dose is critical. [27] A fairly high level of noise as a result of the inherently high contrast levels is tolerable in most patients. Reported radiation doses for CT are 2.8-4.5 mSv, compared with 1.3–1.5 mSv for a 3-image IVU. However, the uterine dose is approximately 0.006 Gy for 4-image IVU, compared with 0.0046 Gy for nonenhanced CT. [28]
At the authors' institution, approximately 12% (10–20%) of patients who undergo nonenhanced CT for possible urinary stones receive intravenous contrast material for further evaluation. To discern between phleboliths and urinary stones, 50 mL of low-osmolar contrast agent should be administered. After 3–5 minutes, a 5-mm helical scan is obtained through the area of concern.
Fewer contrast-enhanced studies are needed with increasing experience. Soft tissue around the rim of a calculus can differentiate it from a phlebolith. A phlebolith may have a comet tail of soft tissue extending from it; this finding differentiates it from a calculus. [29] On CT scans, phleboliths do not have radiolucent centers, as is often seen on plain radiographs. [30, 31]
When contrast-enhanced scans, as shown in the images below, are required to evaluate pain not related to stones, routine abdominal and/or pelvic CT should be performed. [32] In this situation, 100–150 mL of a low-osmolar oral and rectal contrast agent is used, and a 5-mm helical CT scan is obtained with a pitch of 1.5:1. Patient selection determines the number of examinations needed.
 Contrast-enhanced CT section reveals a dense calculus in the right kidney, but the hydronephrosis has resolved.
Contrast-enhanced CT section reveals a dense calculus in the right kidney, but the hydronephrosis has resolved.
 Axial contrast-enhanced CT scan. The excretory phase image through the kidneys shows extravasation of contrast material in and near the renal pelvis and surrounding the proximal ureter, which is opacified. The finding is consistent with fornix rupture.
Axial contrast-enhanced CT scan. The excretory phase image through the kidneys shows extravasation of contrast material in and near the renal pelvis and surrounding the proximal ureter, which is opacified. The finding is consistent with fornix rupture.
 Axial contrast-enhanced CT image through the ureterovesical junction confirms the stone within a left ureterocele. A Foley catheter balloon is visible in the bladder.
Axial contrast-enhanced CT image through the ureterovesical junction confirms the stone within a left ureterocele. A Foley catheter balloon is visible in the bladder.
Stones at the UVJ may be difficult to distinguish from stones that have already passed into the bladder. If the distinction changes therapy, a repeat scan through the UVJ in the prone position may be helpful. Stones that have already passed into the bladder will drop into a dependent location. [33]
CT may depict the following: [34, 35]
-
Stones in the ureter
-
Enlarged kidneys
-
Hydronephrosis (83% sensitive, 94% specific)
-
Perinephric fluid (82% sensitive, 93% specific)
-
Ureteral dilatation (90% sensitive, 93% specific)
The amount of perinephric fluid is correlated with the degree of obstruction seen on IVU, and as with the obstruction, the amount of fluid is correlated with the likelihood of stone passage. Normal hyperattenuating renal pyramids are sometimes seen. These indicate that significant obstruction is not present. However, this finding has been seen with proven ureteral calculi and is often absent in patients without stones. For this reason, the usefulness of IVU is limited. If contrast material is administered, a delayed or hyperattenuating nephrogram may also be visible on CT scans if the ureter has an obstruction.
Conventional radiography may be helpful in visualizing larger stones, once they are identified on CT scans, to provide a baseline to follow passage of the stone. If kidney, ureter, and bladder radiographs fail to depict the stone, CT may be needed to follow its passage.
Approximately 40–55% of stones are not visible on abdominal radiographs. Almost no stones with attenuation values of less than 200 HU are visible. Repeat CT scans are usually required if passage of the stone is to be followed. Cystine and urate stones have an attenuation of 100–500 HU. Calcium stones usually demonstrate attenuation higher than 700 HU. Considerable overlap exists in the CT attenuation values of calcium stones.
Special concerns
In the diagnosis and treatment of kidney stones, special concerns exist in patients who are pregnant, in those who have contraindications to the use of contrast media, and in those with renal insufficiency.
Pregnancy does not predispose patients to stone formation; however, stone formation is a complication in as many as 0.05% of pregnancies, and the diagnosis may be difficult to establish with imaging because of the displacement and obscuration of organs by the enlarged uterus and fetus. [9] Consider using US first in a pregnant patient, especially in the first trimester. IVU can be used, but the views should be limited to scout and 10- to 30-minute images if possible. [36]
CT can also be useful, and the radiation dose may be justified (especially if the clinical picture is confusing), because any fetal damage is unlikely at the typical radiation doses. Minimize the dose by increasing the pitch and decreasing the milliamperage. MRI may be a useful tool for problem solving.
Nonenhanced CT results are usually diagnostic, [37] but if contrast material is needed, actions can be taken to decrease the risk of an adverse reaction in patients. The patient can be premedicated with steroids and histamine blockers. Use of a low-osmolar contrast agent also helps. Use of iodinated contrast agents should be avoided in patients who have had previous life-threatening reactions. Nonenhanced CT is usually sufficient with the aid of US and MRI as problem-solving tools. Nuclear scintigraphy may also be helpful in confirming obstruction. [38]
Usually, in patients with renal insufficiency, nonenhanced CT is sufficient. Very poor renal function results in a failure to opacify the collecting system. As in pregnant patients, US, MRI, and scintigraphy can be useful as problem-solving tools.
If contrast material is used for IVU or for problem solving with CT, nephrotoxicity and allergy-like reactions are possible.
Radiation exposure should be minimized in pregnant women, and female patients should be questioned carefully. If needed, a pregnancy test should be performed prior to CT scanning or radiography. CT may be indicated to confirm or diagnose urinary stone disease and exclude other pelvic pathology in pregnant women. [39]
Magnetic Resonance Imaging
Stones are not directly visible on MRI because they produce no signal. However, they may be indirectly visualized as a filling defect in the ureter or collecting system on heavily T2-weighted images or on gadolinium-enhanced T1-weighted images. [40, 41, 42, 43] MRI can be useful as a problem-solving tool if the use of iodinated contrast material or radiation is contraindicated (eg, due to a contast allergy or during pregnancy). [44]
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
Ultrasonography
On sonograms, stones are demonstrated as bright echogenic foci with posterior acoustic shadowing. Stones are visualized fairly well with US in the kidneys and the distal ureter at or near the UVJ, especially if dilatation is present. US is good for the visualization of complications such as hydronephrosis (or other signs of obstruction); however, some patients with acute obstruction have little or no dilation. [45, 46, 47, 48, 49]
In particular, US is helpful in evaluating those with renal insufficiency or contraindications for the use of contrast media; however, US is often skipped in favor of nonenhanced CT. [50]
In addition, US is good for characterizing lucent filling defects that are visualized as stones on IVU. However, US does not provide direct physiologic information regarding the degree of obstruction. Doppler imaging may demonstrate a high resistive index in acute obstruction, but this may not occur immediately or after forniceal rupture. Absence of the ureteral jet, as visualized with color Doppler on the symptomatic side, is presumptive evidence for a high-grade obstruction in a well-hydrated patient. [51, 52, 53, 54, 55]
US is very insensitive for stones, especially stones smaller than 2 mm, stones at the UPJ, or stones in the mid ureter. Fowler et. al. suggest that US has a sensitivity as low as 24%, compared with nonenhanced CT. Furthermore, estimations of stone size may not be accurate. Compared with nonenhanced CT, US is more dependent on the operator's ability and more time consuming.
US is fairly specific when stones are seen, with a specificity as high as 90%. With US, matrix or Indinavir stones may have soft tissue echogenicity without shadowing. False-positive findings may result from renal vascular calcifications. False-positive diagnoses of hydronephrosis also result from dilated vascular structures in the renal hilum. Doppler imaging is helpful in distinguishing dilated vascular structures from hydronephrosis.
Nuclear Imaging
Nuclear medicine studies may demonstrate the retention of activity in the cortex or collecting system when the obstruction is ongoing. Nuclear medicine tests are useful in determining differential renal function for treatment planning and for assessing how much renal function might return after the obstruction is relieved. [56, 38] For example, a kidney with very little function might be removed if very little function persists after a trial of drainage. Occasionally, confirming the obstruction with nuclear medicine studies is useful if the administration of iodinated contrast material is contraindicated.
Renal function evaluation is not reliable in the presence of ongoing obstruction. Conversely, imaging findings may be normal with low-grade obstruction.
-
Magnified scout intravenous urogram shows a large, relatively lucent calculus in the lower pole of the right kidney.
-
Scout intravenous urogram shows a smooth, dense, round calculus in the left kidney.
-
Intravenous urogram. After the intravenous injection, contrast material in the collecting system obscures the calculus.
-
Scout intravenous urogram shows a smooth stone in the right kidney.
-
Intravenous urogram obtained 5 minutes after the intravenous injection. Contrast material in the collecting system obscures the stone.
-
This intravenous urogram was obtained 10 minutes after the intravenous injection of contrast medium. Additional contrast material is present in the collecting system, and the stone is seen as a relatively lucent filling defect.
-
Renal sonogram demonstrates an echogenic shadowing calculus in the renal collecting system with hydronephrosis.
-
Contrast-enhanced CT section reveals a dense calculus in the right kidney, but the hydronephrosis has resolved.
-
Abdominal radiograph shows calcification filling the left collecting system. This finding is consistent with a staghorn calculus. For its size, the stone is relatively lucent.
-
Contrast-enhanced CT scan demonstrates an opaque staghorn calculus filling the left renal collecting system.
-
Scout intravenous urogram shows innumerable small calcifications in the region of the renal pyramids in a patient with nephrocalcinosis.
-
Scout intravenous urogram demonstrates innumerable calcifications over the medullary region of the left kidney in a patient with nephrocalcinosis.
-
Renal longitudinal sonogram in a patient with nephrocalcinosis shows diffuse echogenic shadowing calcifications in the renal pyramids.
-
Intravenous urogram. Prospectively, no stone was seen on the scout radiograph. In retrospect, a stone in the distal left ureter is projected over the lateral edge of the mid sacrum.
-
This intravenous urogram was obtained 5 minutes after the intravenous injection of contrast agent. A prolonged hyperintense left nephrogram demonstrates delayed contrast material excretion into the left collecting system due to ureteral obstruction.
-
This intravenous urogram was obtained 10 minutes after the intravenous injection of contrast material. Mild left hydronephrosis and hydroureter extend to the level of the stone in the true pelvis.
-
Scout intravenous urogram demonstrates a small, focal, almost triangular, radiopaque calculus on the left side of the pelvis. Another pelvic calcification with central lucency is a typical phlebolith.
-
Scout intravenous urogram was obtained 5 minutes after the intravenous injection of contrast agent. A prolonged hyperintense nephrogram and moderate hydronephrosis are present in the left kidney. The right kidney and collecting system are normal.
-
Intravenous urogram was obtained 10 minutes after the intravenous injection of contrast agent. A column of contrast material in the left ureter extends down to the calculus noted on the scout radiograph. The small phlebolith can barely be seen projecting slightly off the ureter.
-
Intravenous urogram (30-minute delay image) of the right kidney shows a moderately hydronephrotic collecting system to the level of a proximal ureteral stone (arrow).
-
Axial nonenhanced CT section at the level of the kidney demonstrates an attenuating proximal ureteral calculus (arrow). No significant hydronephrosis is identified. CT can be performed much more rapidly than urography and without the use of intravenous contrast material.
-
Scout intravenous urogram demonstrates several calcifications in the left hemipelvis.
-
Intravenous urogram was obtained 10 minutes after the intravenous injection of contrast agent. A prolonged hyperintense nephrogram and mild hydronephrosis are present.
-
Intravenous urogram, delayed radiograph, reveals a large amount of contrast material extravasation (likely a fornix rupture with pyelosinus backflow) in the region of the left renal pelvis. Contrast agent fills the distal ureter.
-
Intravenous urogram, magnified view, shows extravasated contrast agent from a fornix rupture and pyelosinus backflow.
-
Axial nonenhanced CT image at the level of the kidneys shows bilateral renal calculi, right hydronephrosis, and moderate perinephric fluid.
-
Axial nonenhanced CT image of the urinary bladder demonstrates an attenuating calculus at the right ureteropelvic junction.
-
Axial contrast-enhanced CT scan. The excretory phase image through the kidneys shows extravasation of contrast material in and near the renal pelvis and surrounding the proximal ureter, which is opacified. The finding is consistent with fornix rupture.
-
Scout intravenous urogram demonstrates radiopaque left renal calculi in the mid kidney and lower pole.
-
Scout intravenous urogram obtained after lithotripsy shows absence of the previously seen calcification over the mid kidney and linear group of calcifications in the path of the distal left ureter (steinstrasse, from the German, meaning "stone street").
-
Intravenous urogram, magnified view, was obtained after lithotripsy and shows a steinstrasse appearance.
-
Intravenous urogram, 10-minute delay image, demonstrates delayed excretion and a slightly hyperopaque left nephrogram due to obstruction by distal ureteral stone fragments. Stents are often placed to prevent obstruction after lithotripsy.
-
Intravenous urogram, scout radiograph. Large radiopaque calculus overlies the left hemipelvis near the expected location of the ureterovesical junction. Two adjacent phleboliths are noted lateral and caudal to the stone.
-
Intravenous urogram. Magnified view of the scout radiograph reveals faintly lamellated pelvic calcification at the expected location of the left ureterovesical junction.
-
Intravenous urogram (10-min delay). Contrast-enhanced study demonstrates the left ureterocele as a slightly lucent halo around the previously noted pelvic calcification.
-
Intravenous urogram (10-min delay) Magnified view of the left ureterocele with a large stone in it.
-
Axial contrast-enhanced CT image through the ureterovesical junction confirms the stone within a left ureterocele. A Foley catheter balloon is visible in the bladder.
-
Intravenous urogram (tomogram) shows enlarged relatively lucent right kidney with no excretion of contrast material.
-
Intravenous urogram (5-min renal view) shows enlarged relatively lucent right kidney with no excretion of contrast.
-
Longitudinal sonogram of the right kidney demonstrates marked dilatation of the calyces. No calculi are apparent.
-
Sonogram shows marked dilatation of the calyces and communication with the renal pelvis, which confirms severe hydronephrosis.
-
Nonenhanced CT image of the kidneys demonstrates left hydronephrosis and strands of perinephric fluid but no dense calculus.
-
Nonenhanced CT image of the pelvis shows dilatation of the distal left ureter and mild periureteral fluid near the left ureterovesical junction.
-
Nonenhanced CT image of the pelvis shows a small attenuating stone at the left ureterovesical junction.
-
Nonenhanced CT image shows slightly hyperattenuating renal pyramids, most notably on the left. This is a secondary sign and indicates a lack of obstruction of the collecting system.
-
Nonenhanced CT image shows a nonobstructing calculus just above the left ureterovesical junction.
-
Contrast-enhanced CT image of the kidneys shows mild hydronephrosis, perinephric fluid, and delayed enhancement. The perinephric fluid indicates obstruction and correlates with the likelihood of the passage of the stone.
-
Contrast-enhanced CT image of the lower abdomen shows a tiny, obstructing, left ureteral calculus.
-
Magnified nonenhanced CT image of the right kidney shows slightly hyperattenuating renal pyramids in the right kidney despite the mild hydronephrosis.
-
Nonenhanced CT image shows an obstructing right ureteral calculus. A slight rim of soft tissue is noted around the stone (ie, rim sign).
-
Nonenhanced CT image of the right kidney shows slight perinephric fluid but no stone or hydronephrosis.
-
Contrast-enhanced CT image shows a patchy area of hypo-opacity consistent with pyelonephritis.
-
Nonenhanced CT image of the pelvis shows a small calculus in the bladder near the left ureterovesical junction.
-
Prone nonenhanced CT image shows that the stone in the left ureterovesical junction does not move to the dependent portion of the bladder. This finding indicates that it is still in the distal ureter at the ureterovesical junction and that it has not passed into the bladder.
-
Contrast-enhanced CT image of the right kidney shows a cluster of calyceal calculi without hydronephrosis.
-
Nonenhanced CT image shows calcification in a calyceal diverticulum. Calyceal diverticula predispose patients to calculus formation as a result of relative stasis of the urine in the diverticula.
-
Nonenhanced CT image shows nonobstructing right renal calculus, moderate left hydronephrosis, and slight perinephric fluid.
-
Nonenhanced CT image shows an obstructing left proximal ureteral calculus with a slight soft-tissue rim around the stone (ie, rim sign).










