Practice Essentials
Tetralogy of Fallot is the most common type of cyanotic congenital heart disease, followed by transposition of the great vessels. [1] It consists of a right ventricular outflow tract obstruction, a malalignment ventricular septal defect, an overriding aorta, and right ventricular hypertrophy, as demonstrated in the image below. Mortality in untreated patients can reach 50% by 6 years of age. However, cardiac surgery in children with simple forms of tetralogy of Fallot can result in good long-term survival with an excellent quality of life. [2, 3, 4]
Echocardiographic findings are diagnostic for tetralogy of Fallot in infants and young children, and echocardiography may be the only examination required before surgery. Conventional radiography, magnetic resonance imaging (MRI), and angiography are also helpful for complete preoperative evaluation. [2] Angiography is the traditional criterion standard and best modality for the evaluation of the pulmonary and coronary arterial morphology, as well as the morphology of the systemic collateral arteries [5, 6, 7] ; however, intracardiac catheterization may stimulate pulmonary outflow tract spasm. Noninvasive peripheral pulmonary arterial evaluation is possible with MRI. [8, 9, 10, 11, 12]
Echocardiographic findings are diagnostic of intracardiac abnormalities, but echocardiography is limited in the evaluation of the peripheral pulmonary arteries and collateral flow. If the confluence or presence of the branch pulmonary arteries is in doubt after echocardiography, MRI or angiography should be performed.
Spin-echo MRI can be used to identify the morphologic abnormalities of tetralogy of Fallot, which are as follows: right ventricular outflow tract obstruction, ventricular septal defect, right ventricular hypertrophy, and an overriding aorta. Although gradients can be measured with echocardiography, only MR flow analysis enables the accurate cross-sectional measurement of flow. [13, 14, 15, 16, 17, 18, 19, 20]
Computed tomography (CT) scanning has an infrequent role in the evaluation of tetralogy of Fallot. [21, 22] This modality is useful for the evaluation of surgical complications such as infection or pseudoaneurysm formation. Helical CT scanning can be used to identify airway compression that is caused by a large ascending aorta associated with tetralogy of Fallot.
In the postoperative evaluation, echocardiography and MRI are preferred. [10, 13, 14, 23, 24, 25, 26] The choice of imaging examination depends on availability and clinical preference.
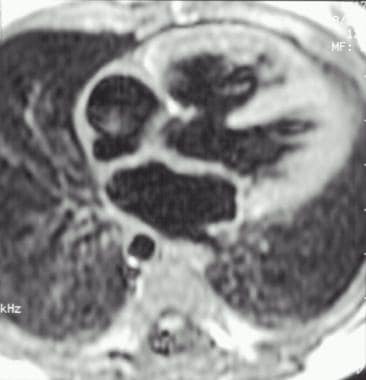 Magnetic resonance image of the heart in an infant with tetralogy of Fallot. This image shows a large ventricular septal defect and right ventricular hypertrophy. Note the descending aorta is on the right, consistent with a right-sided aortic arch.
Magnetic resonance image of the heart in an infant with tetralogy of Fallot. This image shows a large ventricular septal defect and right ventricular hypertrophy. Note the descending aorta is on the right, consistent with a right-sided aortic arch.
Fratz et al concluded that after correction of tetralogy of Fallot, when ventricular volumes are measured with cardiac MRI, axial slices offer greater reproducibility than do short-axis slices. [17] They found that volumes determined using axial slices were subject to significantly less intraobserver variation for right and left ventricular end-diastolic volumes and for left ventricular end-systolic volumes. The same was true for interobserver variation for right and left ventricular end-systolic volumes and for left ventricular end-diastolic volumes. [13]
Iriart et al compared intraobserver and interobserver variations when 3-dimensional (3D) transthoracic echocardiography (combined with a semiautomatic border detection algorithm) was used to measure right ventricular volumes and ejection fractions in patients with corrected tetralogy of Fallot. [27] The investigators found fair agreement between 3D echocardiography and MRI in the assessment of right ventricular volumes and ejection fractions; they also concluded that intraobserver and interobserver variability for 3D echocardiography was adequate. They noted, however, that 3D echocardiography displayed reduced accuracy in the measurement of larger right ventricular volumes. [23]
Kohi et al used cardiac magnetic resonance parameters to assess right ventricular function in patients with combined pulmonary stenosis and pulmonary insufficiency and patients with isolated pulmonary insufficiency following tetralogy of Fallot repair. They concluded that right ventricular function is better preserved in patients with pulmonary stenosis and insufficiency. [14]
Sadeghpour et al found a significant correlation between Doppler-derived mean strain of right ventricular free wall and the right ventricular function measured by cardiac magnetic resonance in adults after tetralogy of Fallot repair. [24]
In an assessment of right ventricular function after surgery for tetralogy of Fallot, Koca et al concluded that myocardial performance index and isovolumic acceleration findings obtained from Doppler imaging echocardiography can be used for long-term follow-up, but they did not correlate with cardiac magnetic resonance-originated right ventricle ejection fraction and pulmonary regurgitation fraction. [25]
AHA/ACC recommendations
The following recommendations were made by the American Heart Association/American College of Cardiology (AHA/ACC) regarding tetralogy of Fallot [4, 28] :
-
Experts in imaging with ultrasonography, echocardiography, and cardiac magnetic resonance imaging (CMRI) are preferred for cardiac imaging in patients with tetralogy of Fallot.
-
Use a standard 12-lead ECG in adults with CHD with serial assessment based on the specific CHD AP classification or when symptoms develop or worsen. Use ambulatory ECG monitoring in patients with CHD who are at risk for tachyarrhythmia, bradyarrhythmia or heart block, of when symptoms of a potential arrhythmic etiology develop.
-
Use ECG to measure QRS duration in patients following repair of tetralogy of Fallot and as part of the evaluation for cardiac resynchronization therapy (CRT).
-
Cardiac MRI, cardiac computed tomography (CCT) scanning, transesophageal echocardiography (TEE), and/or cardiac catherization may be superior to transthoracic echocardiography (TTE) in the assessment of right ventricular (RV) size and function in repaired tetralogy of Fallot, systemic RVs, and other conditions associated with RV volume and pressure overload.
ACR Appropriateness Criteria
The following recommendations have been provided by the American College of Cardiology Appropriateness Criteria for known or suspected congenital heart disease in adults [29] :
-
TTE and MRI are frontline modalities for evaluating heart function and morphology and provide complementary information in diagnosing or assessing adult CHD.
-
Heart CT (CT heart function and morphology with contrast) may be an alternative to MRI and TEE/TTE for evaluating heart function and anatomy. The high spatial resolution of CT is helpful in evaluating smaller and tortuous vessels commonly seen in some disorders. Heart CT does not provide information regarding vessel flow.
-
Although noninvasive methods have reduced some of the need for cardiac catheterization, it remains an important adjunct to noninvasive imaging for hemodynamic measurements and for intervention.
-
MRA of the chest and CTA of the chest provide anatomic information regarding the great vessels and their relationship to each other and the trachea and provide information on extracardiac anatomy.
-
CTA of the coronary arteries is an important adjunctive modality for evaluating coronary anatomy and anomalies or atherosclerosis in the adult patient.
Radiography
The chest radiograph may be normal, or it may show cardiomegaly and prominent right ventricular (RV) shadowing. Although the hallmark of tetralogy of Fallot in infants is the classic boot-shaped heart (see the image below), in which diminished vascularity in the lungs and diminished prominence of the pulmonary arteries become apparent, this classic shape of the heart is not always seen in tetralogy of Fallot. The boot-shaped heart is overlabeled in neonates, who normally have right ventricular hypertrophy. If the chest radiograph shows lordosis, a normal heart may appear boot shaped.
The use of echocardiography has reduced the importance of chest radiography in the initial diagnosis of congenital heart disease. Echocardiography should be used to confirm radiographic findings that are suggestive of tetralogy of Fallot.
In neonates preoperatively, the chest radiograph is used primarily to assess pulmonary vascularity and degree of pulmonary blood flow. Over time, the cardiac silhouette will progress to the boot-shaped heart. Following surgery, the chest radiograph may show cardiac enlargement or differential blood flow to various lung segments. [2, 3, 30]
Typically, the appearance of the vascularity of the pulmonary artery is reduced, but it can also be normal. Decreased pulmonary vascularity is frequently difficult for the general radiologist to appreciate. Large collaterals may give the appearance of normal vascularity.
The enlarged aorta in children with a right-sided arch can cause airway compression that can be identified on chest radiographs, as demonstrated in the images below. A right-sided arch is present in 25% of children with tetralogy of Fallot, and it can be identified by means of direct visualization, with displacement of the trachea to the left or with increased opacity of the spinal pedicles on the ipsilateral side of the aortic arch. The position of the aortic arch influences surgical planning because Blalock-Taussig shunts are more easily placed on the contralateral side of the aortic arch. Modified Blalock-Taussig shunts can be placed bilaterally.
 Radiograph of an infant with tetralogy of Fallot (same patient as in the previous image). Note the anterior compression of the trachea by the large ascending aorta.
Radiograph of an infant with tetralogy of Fallot (same patient as in the previous image). Note the anterior compression of the trachea by the large ascending aorta.
Degree of confidence
Confidence in conventional chest radiographic findings increases with the radiologist's reading experience. The use of echocardiography has reduced the importance of chest radiography in the initial diagnosis of congenital heart disease.
A right-sided aortic arch in a child with congenital heart disease is most commonly associated with tetralogy of Fallot. Children with a large right-sided aortic arch may have a double aortic arch or an aberrant left subclavian artery without congenital heart disease. Other forms of cyanotic heart disease that are associated with a right-sided aortic arch are usually hypervascular and associated with cardiomegaly (eg, truncus arteriosus, transposition of the great arteries).
Although cyanosis and a right-sided aortic arch are associated with tetralogy of Fallot, the presence of cardiomegaly and increased pulmonary vascularity make an admixture lesion the more likely diagnosis. Transposition of the great vessels or truncus arteriosus is associated with increased pulmonary vascularity, cardiomegaly, and cyanosis, as well as a right-sided arch. Approximately one third of children with truncus arteriosus have a right-sided aortic arch. Only 5% of children with transposition of the great vessels have a right-sided aortic arch, but this is a more common form of congenital heart disease than truncus arteriosus.
Computed Tomography
Multidetector cardiac CT can provide spatial and reasonable temporal resolution, producing static and cine imaging as well as 3D reconstructions. Disadvantages of CT include the inability to provide reliable flow rate or velocity data and the use of ionizing radiation. Cardiac CT assessment in tetralogy of Fallot can include visualization of pulmonary artery anatomy, size, and arborization, especially in patients with aortopulmonary shunts, as well as measurement of the lumen and wall thickness of the ascending aorta in older patients. [2, 3, 7, 30]
Magnetic Resonance Imaging
Spin-echo MRI can be used to identify the morphologic abnormalities of tetralogy of Fallot, which are as follows: right ventricular outflow tract obstruction, ventricular septal defect, right ventricular hypertrophy, and an overriding aorta. (Examples of these features are seen in the image below.) [15, 16] Experienced operators are required for a high-quality MRI evaluation. If properly performed, MRI can replace preoperative angiography, which is more invasive. Oblique imaging with thin sections may be necessary to verify pulmonary arterial confluence and identify hypoplastic pulmonary arteries in neonates and infants. Flow analysis of pulmonary regurgitation is susceptible to aliasing if the velocity encoding is too low.
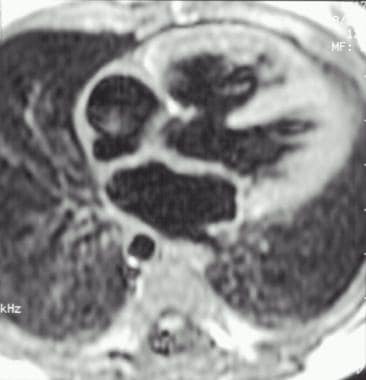 Magnetic resonance image of the heart in an infant with tetralogy of Fallot. This image shows a large ventricular septal defect and right ventricular hypertrophy. Note the descending aorta is on the right, consistent with a right-sided aortic arch.
Magnetic resonance image of the heart in an infant with tetralogy of Fallot. This image shows a large ventricular septal defect and right ventricular hypertrophy. Note the descending aorta is on the right, consistent with a right-sided aortic arch.
The confluence, presence, and size of the branch pulmonary arteries can be identified (see the image below). MRI measurements of the size of the pulmonary and branch pulmonary arteries are as accurate as angiographic measurements, and they can be used to calculate the McGoon ratio and the Nakata index.
 Magnetic resonance image of tetralogy of Fallot in an infant. This image shows a large ascending aorta and the presence of pulmonary atresia. The oval shape of the descending aorta is secondary to large collateral vessels.
Magnetic resonance image of tetralogy of Fallot in an infant. This image shows a large ascending aorta and the presence of pulmonary atresia. The oval shape of the descending aorta is secondary to large collateral vessels.
Cine imaging can be used to identify pulmonary stenosis or regurgitation, which is depicted as flow voids. Right ventricular enlargement is best quantified with MRI. Flow-analysis quantification of pulmonary regurgitation is unique to MRI. Although gradients can be measured with echocardiography, only MR flow analysis enables the accurate cross-sectional measurement of flow. [13]
Ultrasonography
Echocardiography is the primary imaging method for examining a child in whom tetralogy of Fallot is suspected. [11, 12, 23] Intracardiac anomalies, including pulmonary infundibular and valvular stenosis and the position of the aortic root overriding the ventricular septal defect, are identified with 2-dimensional echocardiography. The origins of the coronary arteries can also be identified.
Doppler ultrasonographic examination of the pulmonary outflow tract can be used to measure the velocity gradient in the right ventricular outflow tract and to differentiate severe stenosis from atresia. Continuity of the branch pulmonary artery with the main pulmonary artery can be identified, and the size of the branch pulmonary arteries can be measured. The initial placement of palliative shunts is likely in children who have small branch pulmonary arteries in order to allow the pulmonary arteries to grow before corrective surgery. The full length of the shunts may not be visible; however, Doppler ultrasonography can be used to verify shunt patency, even when the entire length of the shunt cannot be imaged.
Degree of confidence
Intracardiac and central pulmonary artery abnormalities are identified in the presurgical patient with a high degree of confidence. Ultrasonographic windows in the older child and young adult limit the usefulness of echocardiography in postoperative follow-up imaging. Postoperative fibrosis in the mediastinum also reduces the effectiveness of echocardiography.
The pulmonary arteries and systemic-pulmonary arterial shunts are difficult to evaluate after surgery in children. Pulmonary regurgitation, a common complication of corrective surgery, is better evaluated with MRI.
Angiography
Angiography is the traditional criterion standard and best modality for the evaluation of the pulmonary and coronary arterial morphology, as well as the morphology of the systemic collateral arteries. [5, 6, 7] The branch pulmonary arteries have a characteristic seagull appearance (as seen in the image below). Pulmonary arterial measurements for the calculation of the McGoon ratio and Nakata index are critical to surgical planning. An aortic root injection is used to evaluate the position and number of coronary arteries. [16]
 Angiogram in an infant with tetralogy of Fallot and a right-sided aortic arch. This image shows the pulmonary artery is hypoplastic, and the branch pulmonary arteries have a characteristic seagull appearance.
Angiogram in an infant with tetralogy of Fallot and a right-sided aortic arch. This image shows the pulmonary artery is hypoplastic, and the branch pulmonary arteries have a characteristic seagull appearance.
Degree of confidence
Catheter studies remain the criterion standard for blood pressure measurements and morphologic imaging of the coronary and branch pulmonary arteries. Noninvasive techniques are preferred when they are available, so that vascular access for potential future interventional procedures is preserved.
Unlike inherently tomographic studies such as echocardiography, MRI, and CT scanning, angiography may be limited by overlapping structures that may obscure other structures, despite the use of multiple planes.
-
Magnetic resonance image of the heart in an infant with tetralogy of Fallot. This image shows a large ventricular septal defect and right ventricular hypertrophy. Note the descending aorta is on the right, consistent with a right-sided aortic arch.
-
Radiograph of a boot-shaped heart in an infant with tetralogy of Fallot.
-
Radiograph of an infant with tetralogy of Fallot and a right-sided aortic arch.
-
Radiograph of an infant with tetralogy of Fallot (same patient as in the previous image). Note the anterior compression of the trachea by the large ascending aorta.
-
Magnetic resonance image of tetralogy of Fallot in an infant. This image shows a large ascending aorta and the presence of pulmonary atresia. The oval shape of the descending aorta is secondary to large collateral vessels.
-
Angiogram in an infant with tetralogy of Fallot and a right-sided aortic arch. This image shows the pulmonary artery is hypoplastic, and the branch pulmonary arteries have a characteristic seagull appearance.









