Practice Essentials
Aspiration is defined as entry of a foreign substance—solid or liquid—into the respiratory tract or inhalation of fumes and vapors. Aspiration pneumonia is an infectious process caused by aspirated oropharyngeal flora. Aspiration pneumonitis, which is caused by a direct chemical insult from the aspirated material, is technically a different entity, but it is often referred to as aspiration pneumonia. Aspiration is quite common, and the clinical outcome manifests on a spectrum ranging from no sequelae to severe respiratory distress and even death. Clinically, this condition manifests in 3 broad categories [1] :
-
Bacterial infection
-
Airway obstruction
-
Chemical pneumonitis
The clinical course depends on the nature, quantity, and duration of exposure to the aspirated material, the host's defense mechanisms in preventing aspiration, and the response to the injury. Clinical history and examination are crucial in diagnosing aspiration pneumonia.
Aspiration pneumonia is multifactorial [2] ; however, the most common predisposing factors for aspiration in adults are the following:
-
Impaired airway protection mechanisms (loss of cough/gag reflex, unable to maintain airway, alcohol intake, depressed GCS, [3] stroke, impaired glottic closure)
-
Impaired swallowing/dysphagia, enteral feeding support
-
Increased reflux, vomiting
-
Upper GI and airway interventions (endoscopy/bronchoscopy)
-
Body and head position [4]
Gastric acid suppression, though not causative of aspiration, is associated with a worse prognosis because of a loss of protective acid barrier in the stomach and, subsequently, inoculation with a higher bacterial load during aspiration of stomach juices.
Management includes antibiotics (broad-spectrum aerobic and anaerobic cover is recommended), supportive management (especially for chemical pneumonitis), and removal of the foreign object (if possible) when dealing with mechanical obstruction.
The A-DROP (age, dehydration, respiratory, disorientation, and pressure) and modified A-DROP scoring systems have been identified as being associated with in-hospital mortality in patients with aspiration pneumonia. [5]
Imaging modalities
Chest radiography is readily available and inexpensive and is by far the most commonly used imaging test to evaluate aspiration pneumonia. [6, 7, 8, 9, 10, 11] Traditionally, posteroanterior (PA) and lateral chest radiographs have been recommended for imaging aspiration pneumonia and its complications. However, because many patients are not able to cooperate for PA and lateral imaging, anteroposterior (AP) portable images have been more commonly used for diagnosis.
Computed tomography (CT) scanning is the best method for diagnosing aspiration pneumonia, an abscess, or an empyema. [12] CT scanning precisely delineates the location of the lobar or segmental opacity. A foreign body in the tracheobronchial tree and associated atelectasis or consolidation can be defined with relative ease on CT scans. Aspiration of specific material such as fat or contrast material can sometimes be determined by measuring the tissue attenuation on CT scans. Esophageal abnormalities may also be seen on CT images without the need for contrast material. CT scanning is more sensitive and specific than radiography. [13, 14] Necrosis, cavity formation, and empyema are all complications of aspiration pneumonia that are seen better and earlier with CT scanning than with plain radiography.
Magnetic resonance imaging (MRI) has been shown to be more sensitive than plain radiography and CT. Few large studies of MRI dedicated to aspiration diseases have been performed. However, results of published case studies appear to confirm the accuracy of MRI for imaging such conditions as acute inflammation, granuloma, and fibrosis. MRI performs well in defining the nature of the aspirate and the body's reactions to the aspirate. Some authors have found that MRI is superior to CT scanning in the diagnosis of lipoid aspirations. [15]
The sensitivity of MRI is expected to be high, with few false-negative results, although, as with CT scanning, false-positive results due to pathologic processes with features mimicking those of aspiration pneumonia should always be considered.
The patient's swallowing mechanism can be studied by using fluoroscopy with a contrast agent. Videofluoroscopic swallow study (VFSS) is the gold standard in evaluating swallowing difficulty. [16] This is a real-time evaluation of the swallowing process that is often performed in conjunction with speech therapy.
Ultrasonography can be an effective tool for initial diagnosis of aspiration pneumonia when chest radiography or computed tomography cannot be performed, and ultrasound may be a useful tool for monitoring and managing aspiration pneumonia. [17] A systematic review and meta-analysis by Miura et al regarding the diagnostic accuracy of ultrasonography for detecting aspiraton in patients with dysphagia reported a sensitivity and specificity of 0.82 and 0.87, respectively. These results suggest that ultrasound may have a role as a bedside screening tool when aspiration is suspected. [18]
One should always bear in mind that many factors affect the appearance on initial studies, including the patient's hydration status, his or her ability to mount an adequate inflammatory response, and the nature and amount of aspirate. Several days may pass before aspiration pneumonia is visible on imaging studies. Treatment should not be delayed in cases of clinical suspicion without radiologic confirmation.
Radiography
AP portable chest images may demonstrate bilateral opacities in the middle or lower lung zones. On PA and lateral images, the opacities may be localized to the posterior segments of upper lobes or to the superior segments of lower lobes. Alternatively, the radiographic abnormalities may be more extensively distributed. Traditionally, most physicians have depended on plain radiographs, which have moderate to good specificity and sensitivity. However, CT scanning has greater sensitivity and specificity and should be used to more promptly diagnose aspiration pneumonia, to determine its cause, and to detect its complications earlier.
(See the images below.)
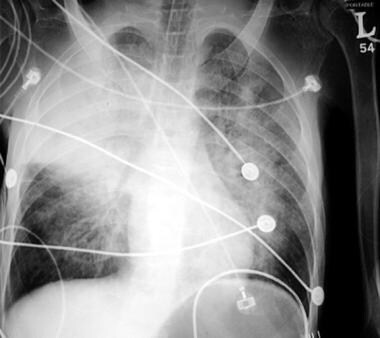 Aspiration pneumonia. A 29-year-old man with history of cerebral palsy and seizure disorder was brought to the emergency department because he had decreased responsiveness for 3 days. The patient was hypothermic, in shock and respiratory distress on arrival and was immediately intubated. Chest radiograph revealed an endotracheal tube far above the carina, bilateral opacities, and a well-defined right upper lobe consolidation.
Aspiration pneumonia. A 29-year-old man with history of cerebral palsy and seizure disorder was brought to the emergency department because he had decreased responsiveness for 3 days. The patient was hypothermic, in shock and respiratory distress on arrival and was immediately intubated. Chest radiograph revealed an endotracheal tube far above the carina, bilateral opacities, and a well-defined right upper lobe consolidation.
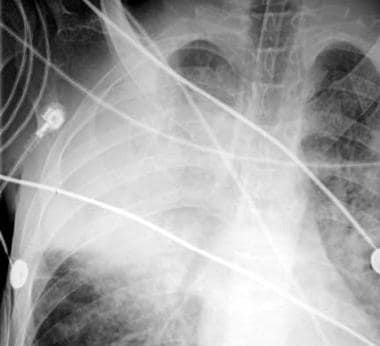 Aspiration pneumonia. Close-up image of the right upper lobe shows lung parenchymal consolidation. The clinical information and imaging data indicate aspiration pneumonia. The aspirate was cultured and demonstrated multiple organisms consistent with aspiration pneumonia.
Aspiration pneumonia. Close-up image of the right upper lobe shows lung parenchymal consolidation. The clinical information and imaging data indicate aspiration pneumonia. The aspirate was cultured and demonstrated multiple organisms consistent with aspiration pneumonia.
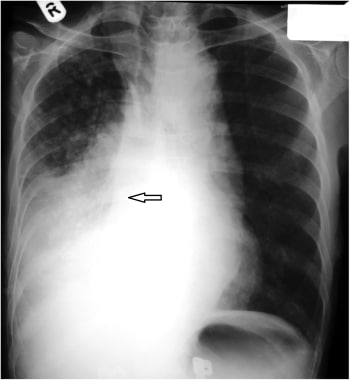
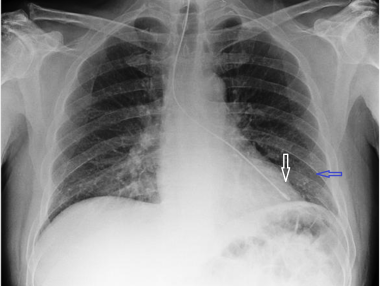
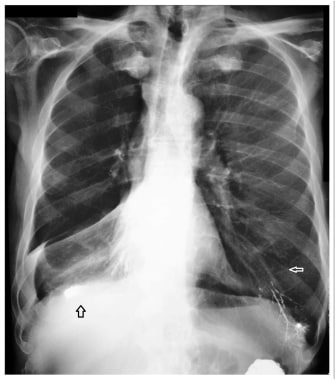
 Aspiration pneumonia. An 84-year-old man in generally good health had fever and cough. Posteroanterior radiograph demonstrates a left lower lobe opacity.
Aspiration pneumonia. An 84-year-old man in generally good health had fever and cough. Posteroanterior radiograph demonstrates a left lower lobe opacity.
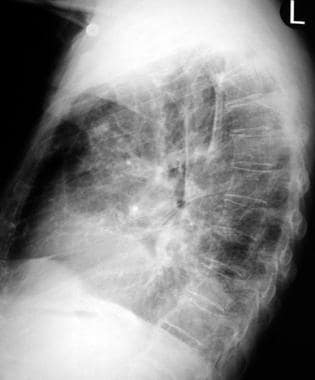 Aspiration pneumonia. Lateral radiograph in an 84-year-old patient confirms the location of an abnormality in the left lower lobe.
Aspiration pneumonia. Lateral radiograph in an 84-year-old patient confirms the location of an abnormality in the left lower lobe.
False-negative findings are associated with subtle or early findings in a clinical course. False-positive findings usually occur when the clinical history is unclear. The findings in aspiration pneumonia are not specific; pulmonary edema, pneumonias from other causes, and neoplasms are included in the differential diagnosis.
Computed Tomography
CT scanning is superior to plain radiography for defining the nature, extent, and complications of aspiration, demonstrating abnormal lung opacities earlier and in more detail than plain chest radiographs. [19] An intratracheal or intrabronchial foreign body can be identified on CT scans, as can any associated atelectasis/consolidation or effect of partial obstruction, such as focal overaeration. Specific aspirates such as fat, low-density organic material (eg, mineral oil), or opaque material can be identified and even measured on CT images.
(See the images below.)
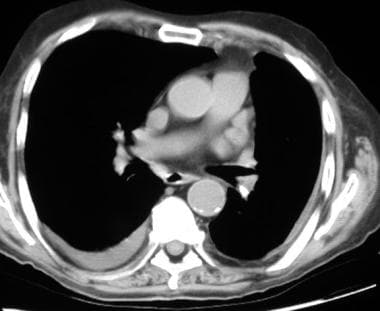
 Aspiration pneumonia. CT scan through the lower lobes on a pulmonary window demonstrates a round opacity in the left lower lobe, which was believed to represent a neoplasm.
Aspiration pneumonia. CT scan through the lower lobes on a pulmonary window demonstrates a round opacity in the left lower lobe, which was believed to represent a neoplasm.
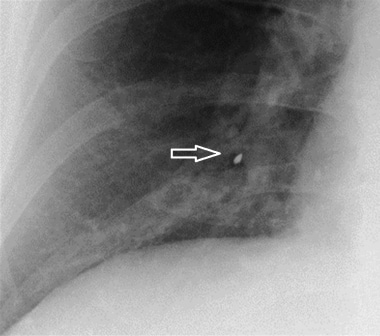
 Aspiration pneumonia. CT scan through the lower-lobe bronchi demonstrates a metallic object in the left lower-lobe bronchus. The patient had aspirated a filling, which had fallen out of one of his teeth. The patient underwent bronchoscopy, and the foreign body was removed. The patient was treated with antibiotics for the pneumonia, which eventually resolved. Incidentally, a small pleural effusion on the right side was due to minimal congestive heart failure (CHF).
Aspiration pneumonia. CT scan through the lower-lobe bronchi demonstrates a metallic object in the left lower-lobe bronchus. The patient had aspirated a filling, which had fallen out of one of his teeth. The patient underwent bronchoscopy, and the foreign body was removed. The patient was treated with antibiotics for the pneumonia, which eventually resolved. Incidentally, a small pleural effusion on the right side was due to minimal congestive heart failure (CHF).
CT or ultrasonographic guidance is useful for localization of abnormalities for biopsy or aspiration/drainage.
Complications from aspiration pneumonia (eg, abscess formation, lung necrosis, empyema) are well depicted on CT scans. Long-term complications, such as obliterative bronchiolitis, are diagnosed best with high-resolution CT (HRCT).
HRCT findings in patients with exogenous lipoid pneumonia may include air-space consolidations with fatty or nonspecific but low attenuation values, areas of ground-glass opacities, septal lines, and centrilobular interstitial thickening. [20, 21, 22, 23] HRCT may also demonstrate a crazy-paving pattern, either isolated or surrounding a pulmonary consolidation.
Multidetector CT (MDCT) has proved to be effective in the evaluation of pneumonia from aspirated foreign bodies or liquid. [24] In patients with suspected foreign body aspiration, virtual bronchoscopy, in conjunction with MDCT, can delineate the precise location of an obstructing foreign body, thereby facilitating conventional bronchoscopy; it can also obviate bronchoscopy by providing an alternative diagnosis. [25]
CT scanning can also define anatomic abnormalities in the head, neck, and chest areas. These findings may be helpful in detailing the underlying causes of aspiration, such as fistulas or tumors in the pharynx, larynx, or esophagus. CT scans may also reveal esophageal strictures, including achalasia.
CT scanning is considered to provide a higher degree of confidence than a single AP, PA, or lateral plain radiograph. However, some of the same diseases that mimic radiographic findings of aspiration can also confound the diagnostic interpretation of CT scans.
Nuclear Imaging
A radionuclide salivagram can demonstrate the aspiration of saliva. [26] Salivagrams can document salivary aspiration as the source of recurrent pneumonia, often in children with neurologic impairment. [27]
Exogenous lipoid pneumonia mimicking malignancy on positron emission tomography (PET) scan has been reported. [28]
A technetium-99m-labeled sulfur colloid scan given orally can demonstrate reflux and micro-aspiration.
(See the images below.)
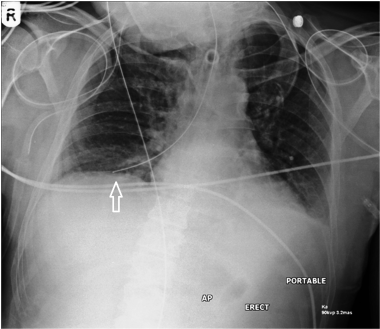
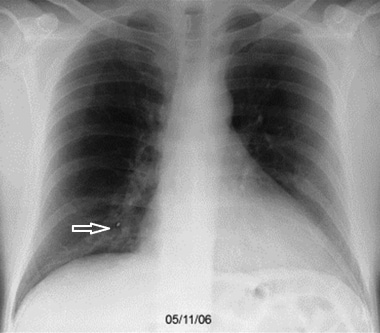
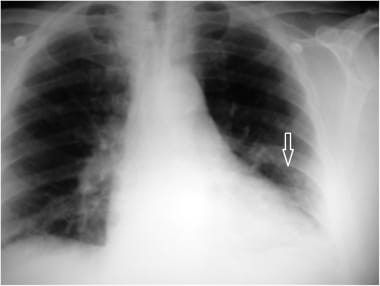 A case of micro-aspiration (1 of 3 images). This patient had micro-aspiration pneumonia (white arrow) that was subsequently investigated by CT and Tc-99M-labeled sulphur colloid swallow study.
A case of micro-aspiration (1 of 3 images). This patient had micro-aspiration pneumonia (white arrow) that was subsequently investigated by CT and Tc-99M-labeled sulphur colloid swallow study.
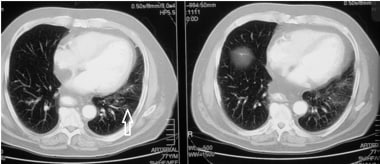 A case of micro-aspiration (2 of 3 images). CT of the chest clearly demonstrates left lung micro-aspiration pneumonia (white arrow).
A case of micro-aspiration (2 of 3 images). CT of the chest clearly demonstrates left lung micro-aspiration pneumonia (white arrow).
Aspiration Pneumonia Cases
A case of a perforated esophagus leading to aspiration pneumonia is described in the images below.
 A case of esophageal perforation (1 of 2 images). This patient developed aspiration pneumonia as a consequence of esophageal perforation. This x-ray shows leakage of the water-soluble contrast from the esophagus (white arrow).
A case of esophageal perforation (1 of 2 images). This patient developed aspiration pneumonia as a consequence of esophageal perforation. This x-ray shows leakage of the water-soluble contrast from the esophagus (white arrow).
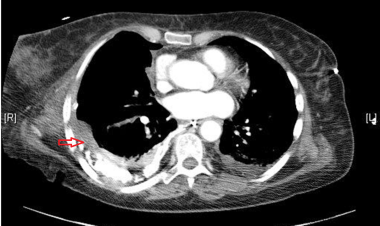 A case of esophageal perforation (2 of 2 images). This patient had esophageal perforation. CT shows aspiration pneumonia in the right lower lobe (red arrow).
A case of esophageal perforation (2 of 2 images). This patient had esophageal perforation. CT shows aspiration pneumonia in the right lower lobe (red arrow).
A case of fatal Gastrografin (diatrizoate meglumine and diatrizoate sodium) aspiration is described in the images below.
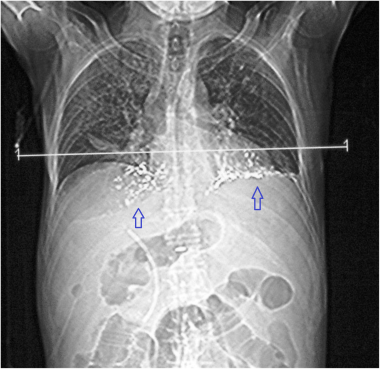 A case of fatal gastrografin aspiration (1 of 2 images). This patient had fatal gastrografin aspiration. The hyperdense aspirates are visible bilaterally on this CT scout film (blue arrows).
A case of fatal gastrografin aspiration (1 of 2 images). This patient had fatal gastrografin aspiration. The hyperdense aspirates are visible bilaterally on this CT scout film (blue arrows).
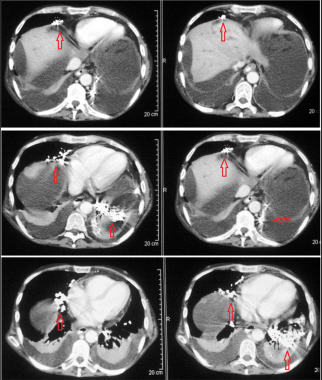 A case of fatal gastrografin aspiration (2 of 2 images). CT makes it easier to identify the gastrografin aspirates. Red arrows show extensive hyperdense aspirates present bilaterally, more so in the left lung.
A case of fatal gastrografin aspiration (2 of 2 images). CT makes it easier to identify the gastrografin aspirates. Red arrows show extensive hyperdense aspirates present bilaterally, more so in the left lung.
A case of micro-aspiration is described in the images below.
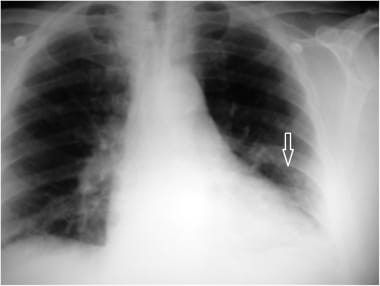 A case of micro-aspiration (1 of 3 images). This patient had micro-aspiration pneumonia (white arrow) that was subsequently investigated by CT and Tc-99M-labeled sulphur colloid swallow study.
A case of micro-aspiration (1 of 3 images). This patient had micro-aspiration pneumonia (white arrow) that was subsequently investigated by CT and Tc-99M-labeled sulphur colloid swallow study.
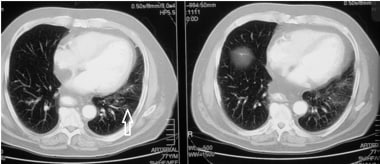 A case of micro-aspiration (2 of 3 images). CT of the chest clearly demonstrates left lung micro-aspiration pneumonia (white arrow).
A case of micro-aspiration (2 of 3 images). CT of the chest clearly demonstrates left lung micro-aspiration pneumonia (white arrow).
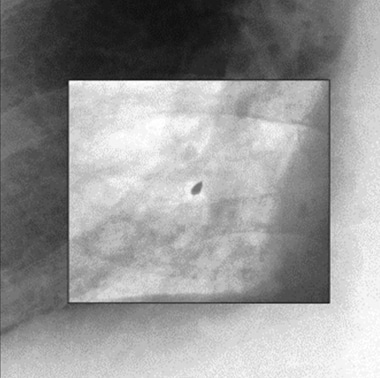
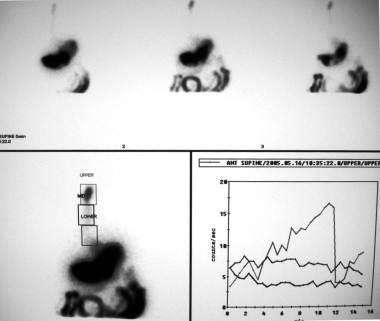 A case of micro-aspiration (3 of 3 images). Micro-aspiration elegantly shown by a Tc-99M-labeled sulphur colloid swallow study.
A case of micro-aspiration (3 of 3 images). Micro-aspiration elegantly shown by a Tc-99M-labeled sulphur colloid swallow study.
Examples of misplaced tubes are shown in the images below. If not identified early, these misplaced tubes may lead to aspiration pneumonia.
 A case of misplaced nasogastric tube. Note the position of the NG tube in right lower bronchus (white arrow).
A case of misplaced nasogastric tube. Note the position of the NG tube in right lower bronchus (white arrow).
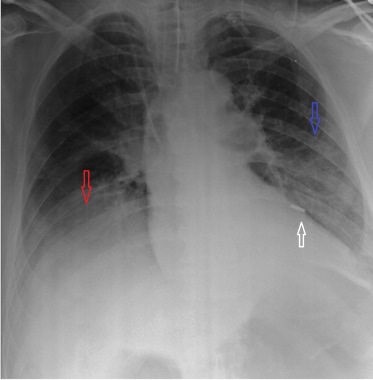 A case of misplaced nasogastric tube. Note the position of the NG tube (white arrow), left-sided pneumonia (blue arrow) and a parapneumonic effusion of the right lung (red arrow).
A case of misplaced nasogastric tube. Note the position of the NG tube (white arrow), left-sided pneumonia (blue arrow) and a parapneumonic effusion of the right lung (red arrow).
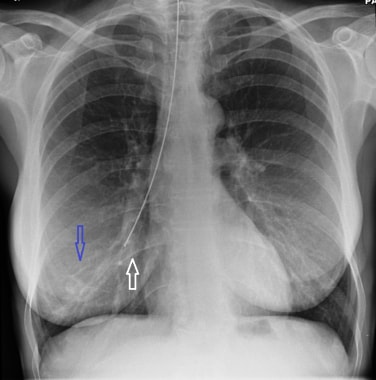 A case of misplaced nasogastric tube. Note the position of the NG tube (white arrow), and mild right aspiration pneumonia (blue arrow).
A case of misplaced nasogastric tube. Note the position of the NG tube (white arrow), and mild right aspiration pneumonia (blue arrow).
 A case of misplaced nasogastric tube. Note the position of the NG tube (white arrow), and mild left aspiration pneumonia (blue arrow).
A case of misplaced nasogastric tube. Note the position of the NG tube (white arrow), and mild left aspiration pneumonia (blue arrow).
 A case of misplaced endotracheal tube. Note the position of the ET tube (white arrow) and aspiration pneumonia of right lower lobe (blue arrow).
A case of misplaced endotracheal tube. Note the position of the ET tube (white arrow) and aspiration pneumonia of right lower lobe (blue arrow).
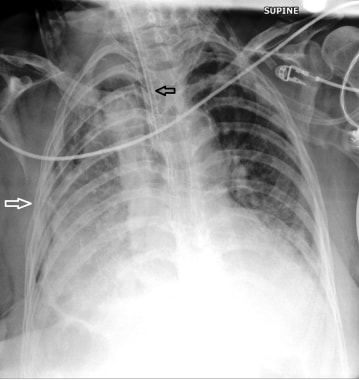 A case of misplaced endotracheal tube. Note the position of the ET tube (black arrow) and the resulting right hemithorax aspiration pneumonia (white arrow).
A case of misplaced endotracheal tube. Note the position of the ET tube (black arrow) and the resulting right hemithorax aspiration pneumonia (white arrow).
Chemical aspiration pneumonitis is displayed in the image below.
Cases of foreign body aspiration are shown in the images below. The foreign bodies may lead to aspiration pneumonia or airway collapse/atelectasis.
 A case of dentures (1 of 3 images). This patient had swallowed his dentures, which impacted in the upper airway (red arrow) as visualised in this digital x-ray. Subsequently, this patient developed aspiration pneumonia.
A case of dentures (1 of 3 images). This patient had swallowed his dentures, which impacted in the upper airway (red arrow) as visualised in this digital x-ray. Subsequently, this patient developed aspiration pneumonia.
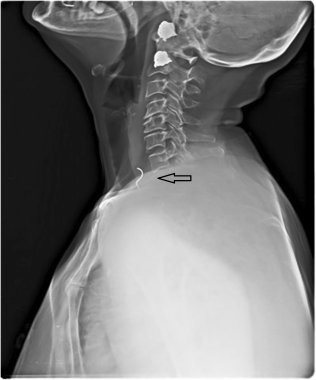 A case of dentures (2 of 3 images). A lateral x-ray of the soft tissues of the neck of the same patient. Note the dentures are impacted in the upper esophagus.
A case of dentures (2 of 3 images). A lateral x-ray of the soft tissues of the neck of the same patient. Note the dentures are impacted in the upper esophagus.
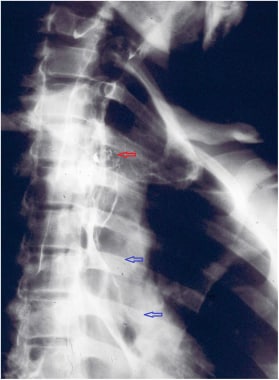 A case of dentures (3 of 3 images). Note the dentures in the upper esophagus (red arrow) and aspiration of a water-soluble contrast agent (blue arrows) past the impacted dentures.
A case of dentures (3 of 3 images). Note the dentures in the upper esophagus (red arrow) and aspiration of a water-soluble contrast agent (blue arrows) past the impacted dentures.
 A case of foreign body aspiration (1 of 3 images). This chest x-ray shows aspiration of a radio-opaque foreign body, present in the right lower bronchus (white arrow).
A case of foreign body aspiration (1 of 3 images). This chest x-ray shows aspiration of a radio-opaque foreign body, present in the right lower bronchus (white arrow).
 A case of foreign body aspiration (3 of 3 images). Enhanced inverted color image makes the foreign body more prominent.
A case of foreign body aspiration (3 of 3 images). Enhanced inverted color image makes the foreign body more prominent.
A case of evolving aspiration pneumonia due to tracheostomy is shown and described in the images below.
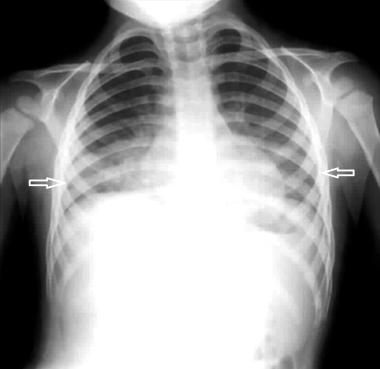
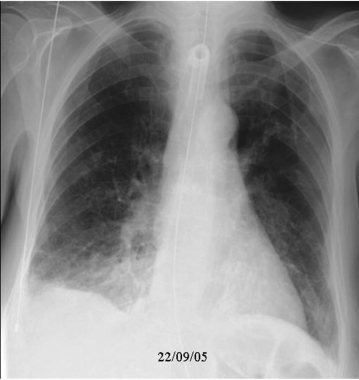
 A case of evolving aspiration pneumonia (1 of 4 images). This patient had a tracheostomy, followed by development of bilaterial aspiration pneumonia. The following images show the evolving aspiration pneumonia over the next few days and, subsequently, its resolution following appropriate treatment.
A case of evolving aspiration pneumonia (1 of 4 images). This patient had a tracheostomy, followed by development of bilaterial aspiration pneumonia. The following images show the evolving aspiration pneumonia over the next few days and, subsequently, its resolution following appropriate treatment.
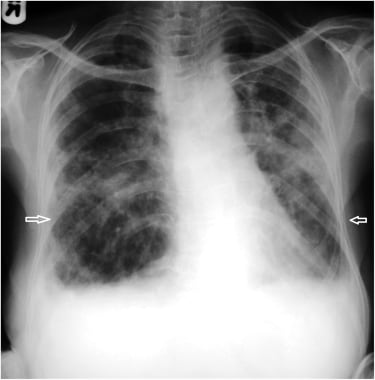
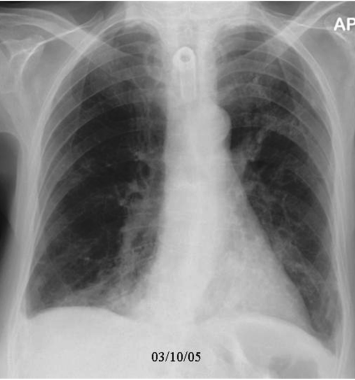
 A case of evolving aspiration pneumonia (2 of 4 images). Day 2 x-ray shows bilateral lower zone changes have worsened, more so on the right side.
A case of evolving aspiration pneumonia (2 of 4 images). Day 2 x-ray shows bilateral lower zone changes have worsened, more so on the right side.
 A case of evolving aspiration pneumonia (3 of 4 images). Day 6 x-ray shows worsening bilateral lower zone changes; worse on the right with some parapneumonic effusion as well.
A case of evolving aspiration pneumonia (3 of 4 images). Day 6 x-ray shows worsening bilateral lower zone changes; worse on the right with some parapneumonic effusion as well.
 A case of evolving aspiration pneumonia (4 of 4 images). Day 16 x-ray shows marked recovery after treatment.
A case of evolving aspiration pneumonia (4 of 4 images). Day 16 x-ray shows marked recovery after treatment.
Images of cases of miscellaneous aspiration pneumonia, caused by barium, bulbar palsy, esophageal stricture, and seizure, are shown below.
 Barium aspiration. Note the barium outlining the left lobe bronchi (white arrow) and pneumonic changes at right lung base (black arrow), associated with a mild pleural effusion.
Barium aspiration. Note the barium outlining the left lobe bronchi (white arrow) and pneumonic changes at right lung base (black arrow), associated with a mild pleural effusion.
-
Aspiration pneumonia. A 29-year-old man with history of cerebral palsy and seizure disorder was brought to the emergency department because he had decreased responsiveness for 3 days. The patient was hypothermic, in shock and respiratory distress on arrival and was immediately intubated. Chest radiograph revealed an endotracheal tube far above the carina, bilateral opacities, and a well-defined right upper lobe consolidation.
-
Aspiration pneumonia. Close-up image of the right upper lobe shows lung parenchymal consolidation. The clinical information and imaging data indicate aspiration pneumonia. The aspirate was cultured and demonstrated multiple organisms consistent with aspiration pneumonia.
-
Aspiration pneumonia. An 84-year-old man in generally good health had fever and cough. Posteroanterior radiograph demonstrates a left lower lobe opacity.
-
Aspiration pneumonia. Lateral radiograph in an 84-year-old patient confirms the location of an abnormality in the left lower lobe.
-
Aspiration pneumonia. CT scan through the lower lobes on a pulmonary window demonstrates a round opacity in the left lower lobe, which was believed to represent a neoplasm.
-
Aspiration pneumonia. CT scan through the lower-lobe bronchi demonstrates a metallic object in the left lower-lobe bronchus. The patient had aspirated a filling, which had fallen out of one of his teeth. The patient underwent bronchoscopy, and the foreign body was removed. The patient was treated with antibiotics for the pneumonia, which eventually resolved. Incidentally, a small pleural effusion on the right side was due to minimal congestive heart failure (CHF).
-
This patient had bilateral paraffin pneumonitis (chemical aspiration pneumonitis).
-
A case of dentures (1 of 3 images). This patient had swallowed his dentures, which impacted in the upper airway (red arrow) as visualised in this digital x-ray. Subsequently, this patient developed aspiration pneumonia.
-
A case of dentures (2 of 3 images). A lateral x-ray of the soft tissues of the neck of the same patient. Note the dentures are impacted in the upper esophagus.
-
A case of dentures (3 of 3 images). Note the dentures in the upper esophagus (red arrow) and aspiration of a water-soluble contrast agent (blue arrows) past the impacted dentures.
-
A case of evolving aspiration pneumonia (1 of 4 images). This patient had a tracheostomy, followed by development of bilaterial aspiration pneumonia. The following images show the evolving aspiration pneumonia over the next few days and, subsequently, its resolution following appropriate treatment.
-
A case of evolving aspiration pneumonia (2 of 4 images). Day 2 x-ray shows bilateral lower zone changes have worsened, more so on the right side.
-
A case of evolving aspiration pneumonia (3 of 4 images). Day 6 x-ray shows worsening bilateral lower zone changes; worse on the right with some parapneumonic effusion as well.
-
A case of evolving aspiration pneumonia (4 of 4 images). Day 16 x-ray shows marked recovery after treatment.
-
A case of foreign body aspiration (1 of 3 images). This chest x-ray shows aspiration of a radio-opaque foreign body, present in the right lower bronchus (white arrow).
-
A case of foreign body aspiration (2 of 3 images). Close-up view of the radio-opaque foreign body.
-
A case of foreign body aspiration (3 of 3 images). Enhanced inverted color image makes the foreign body more prominent.
-
A case of fatal gastrografin aspiration (1 of 2 images). This patient had fatal gastrografin aspiration. The hyperdense aspirates are visible bilaterally on this CT scout film (blue arrows).
-
A case of fatal gastrografin aspiration (2 of 2 images). CT makes it easier to identify the gastrografin aspirates. Red arrows show extensive hyperdense aspirates present bilaterally, more so in the left lung.
-
A case of micro-aspiration (1 of 3 images). This patient had micro-aspiration pneumonia (white arrow) that was subsequently investigated by CT and Tc-99M-labeled sulphur colloid swallow study.
-
A case of micro-aspiration (2 of 3 images). CT of the chest clearly demonstrates left lung micro-aspiration pneumonia (white arrow).
-
A case of micro-aspiration (3 of 3 images). Micro-aspiration elegantly shown by a Tc-99M-labeled sulphur colloid swallow study.
-
A case of misplaced endotracheal tube. Note the position of the ET tube (black arrow) and the resulting right hemithorax aspiration pneumonia (white arrow).
-
A case of misplaced endotracheal tube. Note the position of the ET tube (white arrow) and aspiration pneumonia of right lower lobe (blue arrow).
-
A case of misplaced nasogastric tube. Note the position of the NG tube (white arrow), and mild left aspiration pneumonia (blue arrow).
-
A case of misplaced nasogastric tube. Note the position of the NG tube (white arrow), and mild right aspiration pneumonia (blue arrow).
-
A case of misplaced nasogastric tube. Note the position of the NG tube (white arrow), left-sided pneumonia (blue arrow) and a parapneumonic effusion of the right lung (red arrow).
-
A case of misplaced nasogastric tube. Note the position of the NG tube in right lower bronchus (white arrow).
-
A case of esophageal perforation (1 of 2 images). This patient developed aspiration pneumonia as a consequence of esophageal perforation. This x-ray shows leakage of the water-soluble contrast from the esophagus (white arrow).
-
A case of esophageal perforation (2 of 2 images). This patient had esophageal perforation. CT shows aspiration pneumonia in the right lower lobe (red arrow).
-
Barium aspiration. Note the barium outlining the left lobe bronchi (white arrow) and pneumonic changes at right lung base (black arrow), associated with a mild pleural effusion.
-
Bilateral aspiration pneumonia (white arrows) due to Bulbar palsy.
-
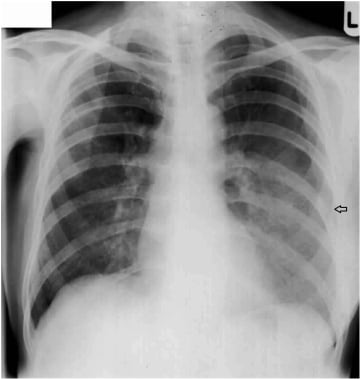
Left aspiration pneumonia (black arrow) due to an esophageal stricture.
-
Moderate to severe right-sided aspiration pneumonia (black arrow) in a patient following a seizure.