Practice Essentials
Polyarteritis nodosa (PAN) is an autoimmune systemic inflammatory vasculitis that results in transmural fibrinoid necrosis with surrounding inflammation in small and medium-size vessels. Characteristic imaging findings of PAN are microaneurysms, often involving the renal arteries (see the images below). Polyarteritis nodosa commonly affects the kidneys, heart, liver, and gastrointestinal tract, with the kidney being the organ most commonly involved (79% of cases at autopsy). [1, 2, 3] Renal involvement results in proteinuria, hematuria, and hypertension, but not glomerulonephritis. [4] Affected patients present with nonspecific systemic symptoms such as low-grade fever, malaise, arthralgia, myalgia, loss of appetite, and weight loss. [5, 6, 7, 8, 9]
PAN is a rare disease with a reported global incidence of 2.4 per million people and is most often seen in men aged 45-65 years. The etiology is not completely understood, but there have been links to the hepatitis B virus (HBV). Loss-of-function mutations in CECR1 (also known as ADA2) have been described. [10]
In addition to hepatitis B, infections that have been linked to PAN include Klebsiella, Toxoplasma, Pseudomonas, Trichinosis, parvovirus B-19, and Yersinia. PAN has also been linked to Sjogren syndrome, rheumatoid arthritis, and hairy cell leukemia. [7, 8]
For an accurate diagnosis of polyarteritis nodosa, selective arteriography is the criterion standard. Analysis of biopsy specimens from the subcutaneous nodules or skeletal muscle may be helpful in establishing the diagnosis, although biopsy has a success rate of only 20-35%. Although biopsy was used more extensively in the past, this procedure has fallen into disfavor because of sampling errors and its low success rate. Angiography can be helpful in confirming or supporting the clinical diagnosis of polyarteritis nodosa; however, this procedure is an invasive test. [11, 12, 13, 14]
CT and MRI angiograms will support the diagnosis of PAN, demonstrating aneurysms or stenosis of medium-sized muscular arteries, especially renal and mesenteric vasculature. [5]
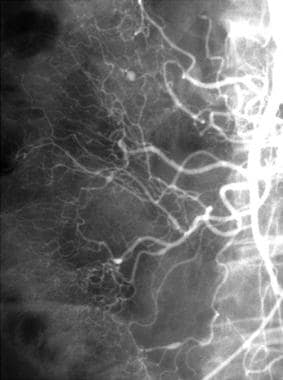
 Polyarteritis nodosa in a 47-year-old man with abdominal pain, weight loss, and an elevated erythrocyte sedimentation rate. Right renal arteriogram reveals multiple microaneurysms within the upper pole of the kidney on this selective right renal artery injection (upper pole branch).
Polyarteritis nodosa in a 47-year-old man with abdominal pain, weight loss, and an elevated erythrocyte sedimentation rate. Right renal arteriogram reveals multiple microaneurysms within the upper pole of the kidney on this selective right renal artery injection (upper pole branch).
 Polyarteritis nodosa. Superior mesenteric injection in a 56-year-old woman with arthralgias reveals a few small microaneurysms.
Polyarteritis nodosa. Superior mesenteric injection in a 56-year-old woman with arthralgias reveals a few small microaneurysms.
The differential diagnosis includes Churg-Strauss disease, Churg-Strauss syndrome, leukocytoclastic vasculitis, systemic lupus erythematosus, and Wegener granulomatosis. Other conditions that should be considered are acute glomerulonephritis, drug-induced vasculitis, and vasculitis associated with lupus, scleroderma, rheumatoid arthritis, and Wegener granulomatosis.
Transcatheter embolization should be considered only in cases involving larger aneurysms, because of the potential for rupture, and when bleeding occurs from rupture of the aneurysm.
Guidelines
According to the Revised International Chapel Hill Consensus, the presence of necrotizing small and medium-sized vessel arteritis without glomerulonephritis or vasculitis in the arterioles, capillaries, or venules, along with negative antineutrophilic cytoplasmic antibodies, suggests the diagnosis of systemic PAN. [6, 15]
According to the American College of Rheumatology, meeting 3 of the 10 following criteria establishes a diagnosis of PAN with a sensitivity of 82.2% and a specificity of 86.6%. [16]
- Weight loss >4 kg
- Llivedo reticularis
- Testicular pain or tenderness
- Myalgias, weakness, or leg tenderness
- Mononeuropathy or polyneuropathy
- Diastolic blood pressure >90 mmHg
- Elevated blood urea nitrogen >40 mg/dL or creatinine >1.5 mg/dL not attributable to dehydration or obstruction
- Presence of hepatitis B surface antigen or antibody in serum
- Arteriogram showing aneurysms or occlusions of the visceral arteries not attributable to arteriosclerosis, fibromuscular dysplasia, or other noninflammatory causes
- Biopsy of small or medium-sized artery containing polymorphonuclear neutrophils
Recommendations have also been published by the European League Against Rheumatism (EULAR) and the French Vasculitis Study Group (FVSG). [6, 17, 18, 19]
Radiography
In patients with polyarteritis nodosa, excretory urographic findings are often normal . Subtle findings can include increased renal size, ureteral dilatation, perinephric hematoma, and renal infarction. [20]
(See the image below.)
Computed Tomography
CT scan findings are nonspecific in PAN, but they include bowel wall thickening; vascular engorgement; haziness in the mesentery; ascites; ureteral dilatation; renal, hepatic, and splenic infarctions; and perinephric hematoma. [21, 22]
(See the image below.)
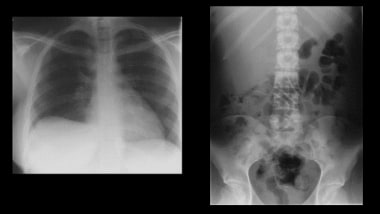 Chest and abdominal radiographs on a previously healthy 24-year-old female student who presented with a sudden onset of right upper quadrant pain. Note the elevated right hemidiaphragm with a fuzzy superior surface and a suggestion of mass in the upper left quadrant on the abdominal radiograph.
Chest and abdominal radiographs on a previously healthy 24-year-old female student who presented with a sudden onset of right upper quadrant pain. Note the elevated right hemidiaphragm with a fuzzy superior surface and a suggestion of mass in the upper left quadrant on the abdominal radiograph.
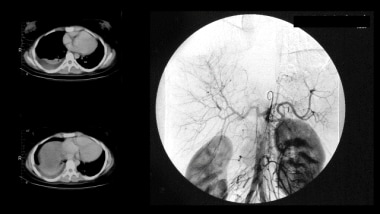 Axial contrast-enhanced CT scans and digital subtraction celiac axis angiogram of the same patient as in the previous image. The axial CT scans show an ill-defined mass in the liver under the right hemi-diaphragm associated with a right basal effusion. The angiogram show multiple micro-aneurysms within the liver.
Axial contrast-enhanced CT scans and digital subtraction celiac axis angiogram of the same patient as in the previous image. The axial CT scans show an ill-defined mass in the liver under the right hemi-diaphragm associated with a right basal effusion. The angiogram show multiple micro-aneurysms within the liver.
Angiography
Selective arteriography is the best modality for evaluating and diagnosing polyarteritis nodosa. The most striking pathognomonic finding is the appearance of aneurysms, usually microaneurysms, which are believed to be caused by rupture of a vessel wall (see the images below).
Microaneurysms are often multiple, usually numbering 10 or more in any single visceral circulation. In most patients, they are 2-5 mm in size. Saccular aneurysms (1-5 mm) of small and medium-sized vessels are typically found. Usually, microaneurysms can be identified in 60-80% of patients, and although they are considered to be pathognomonic for polyarteritis nodosa, these lesions can be encountered in other vasculitides. The aneurysms are caused by segmental occlusion of the arteries with weakening of the arterial wall, which occurs as a result of the necrotizing inflammatory process.
 Polyarteritis nodosa in a 47-year-old man with abdominal pain, weight loss, and an elevated erythrocyte sedimentation rate. Right renal arteriogram reveals multiple microaneurysms within the upper pole of the kidney on this selective right renal artery injection (upper pole branch).
Polyarteritis nodosa in a 47-year-old man with abdominal pain, weight loss, and an elevated erythrocyte sedimentation rate. Right renal arteriogram reveals multiple microaneurysms within the upper pole of the kidney on this selective right renal artery injection (upper pole branch).
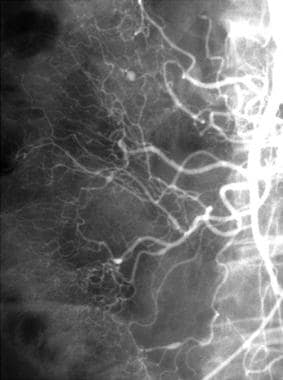 Polyarteritis nodosa. Superior mesenteric injection in a 56-year-old woman with arthralgias reveals a few small microaneurysms.
Polyarteritis nodosa. Superior mesenteric injection in a 56-year-old woman with arthralgias reveals a few small microaneurysms.
The most common sites of involvement of polyarteritis nodosa are the branching points and bifurcations of arteries. Common sequelae of this condition are intravascular thrombosis, aneurysm rupture, and arterial occlusion with resultant infarctions. In the kidneys, these sequelae can cause ischemic atrophy and hemorrhage. The hemorrhage is usually intrarenal, perinephric, subcapsular, or retroperitoneal.
Other angiographic features of polyarteritis nodosa include tortuous vessels with irregular lumina, segmental luminal narrowing or dilatation, infarctions, vascular irregularity, segmental occlusions, and hypervascularity in regions of PAN. [11, 12, 13]
Although angiographic findings of microaneurysm, ectasia, and/or occlusive disease suggest the diagnosis of polyarteritis nodosa, these findings may be seen in other vasculitides, including rheumatoid vasculitis, Churg-Strauss syndrome, necrotizing angiitis associated with drug abuse, and systemic lupus erythematosus. Correlation with the clinical evaluation is important.
-
Polyarteritis nodosa in a 47-year-old man with abdominal pain, weight loss, and an elevated erythrocyte sedimentation rate. Right renal arteriogram reveals multiple microaneurysms within the upper pole of the kidney on this selective right renal artery injection (upper pole branch).
-
Polyarteritis nodosa. Superior mesenteric injection in a 56-year-old woman with arthralgias reveals a few small microaneurysms.
-
Axial non-contrast CT scan through the liver on 36-year-old female patient with known Systemic Lupus Erythematosus who presented with a sudden onset of right upper quadrant pain and a drop in hemoglobin. A contrast scan was not undertaken at the time because of a raised EGFR. Note the peripheral crescentic mixed attenuation along the lateral surface of the liver secondary to a hematoma.
-
A celiac axis angiogram shows multiple micro-aneurysms within the liver and relatively hypovascular area due to a hematoma. Angiography was carried out to (or “intending to”) embolization of bleeding point. The procedure was not done as there was no active bleeding.
-
Hepatic angiography shows a bleeding microaneurysm in polyarteritis nodosa. Note hematoma in the peripheral right lower edge of the liver. The next figure shows pre-and post-embolization in superselective hepatic angiography.
-
Superselective hepatic angiography in polyarteritis nodosa shows post-embolization angiogram indicating a cessation of bleeding.
-
Chest and abdominal radiographs on a previously healthy 24-year-old female student who presented with a sudden onset of right upper quadrant pain. Note the elevated right hemidiaphragm with a fuzzy superior surface and a suggestion of mass in the upper left quadrant on the abdominal radiograph.
-
Axial contrast-enhanced CT scans and digital subtraction celiac axis angiogram of the same patient as in the previous image. The axial CT scans show an ill-defined mass in the liver under the right hemi-diaphragm associated with a right basal effusion. The angiogram show multiple micro-aneurysms within the liver.








