Practice Essentials
Osteochondritis dissecans (OCD) is characterized by separation of an osteochondral fragment from the articular surface. An osteochondral fragment may be present in situ, incompletely detached, or completely detached. A completely detached fragment is a loose body. OCD is limited to the articular epiphysis. Articular epiphyses fail as a result of compression. Trauma is most likely the primary insult, and ischemia a secondary injury. [1, 2, 3] Osteochondritis dissecans occurs in approximately 15 to 29 per 100,000 patients. Most of the patients are 10-20 years of age, with males affected about twice as often as females and a higher incidence occurring in young athletes. The knee, particularly the lateral aspect of the medial femoral condyle, is the most affected joint, and the elbow (capitellum) and ankle (talus) are affected to a lesser degree. [2]
On conventional radiographs, osteochondral lesions can appear as lucencies in the articular epiphysis. OCD is suggested by a loss of the sharp cortical line of the articular surface. [4, 5, 6, 7, 8, 9] Plain radiographs are limited in the ability to determine the stability of OCD lesions. MRI provides a more precise evaluation of the size of the lesion and structure of the overlying cartilage. [10]
In the ankle joint, helical CT has multiplanar capability. CT is obtained in the direct axial and coronal planes at 1.5-mm-slice thickness with sagittal reformations. The shortcomings of CT are applied radiation, especially in pediatric patients, and lack of cartilage visualization. The lack of cartilage visualization can be overcome by using intra-articular contrast material. CT scans can be used to assess the osseous integration after refixation of OCD loose fragments. [11, 12, 13, 9]
MRI detects radiographically occult lesions that may not be detected on CT. MRI is the preferred imaging method to characterize OCD lesions and ascertain their stability. Satake et al found that MRI had a sensitivity of 84% for OCD, [14] and Itsubo et al found 100% sensitivity and 80% specificity. [15, 16, 17, 18, 19, 20, 21]
Ultrasonography has been used to evaluate osteochondritis dissecans of the knee and humeral capitellum. The advantage of ultrasound is dynamic scanning with motion of the evaluated joint. [22, 20, 23, 24, 25, 26]
Scintigraphic findings are nonspecific, demonstrating a mild-to-marked increase in focal uptake in the involved bone, depending on the age of the osteochondritis dissecans. [27, 28, 2]
(See the images below.)
 Lateral radiograph of the knee reveals a calcified loose body (arrowhead) posterior to the knee and lucency (arrow) in the articular surface of the patella.
Lateral radiograph of the knee reveals a calcified loose body (arrowhead) posterior to the knee and lucency (arrow) in the articular surface of the patella.
 Anteroposterior radiograph of the knee demonstrates lucency (arrow) in the central and superior aspect of the patella.
Anteroposterior radiograph of the knee demonstrates lucency (arrow) in the central and superior aspect of the patella.
Trauma may be direct, such as impaction fracture, or repetitive microtrauma, such as excessive normal compressive stress. [29, 30] The pathology of OCD may be described in 3 stages.
In the first stage (acute injury), thickened and edematous intra-articular and periarticular soft tissues are observed. Often, the adjacent metaphysis reveals mild osteoporosis resulting from active hyperemia of the metaphysis.
In the second stage, the epiphysis reveals an irregular contour and a thinning of the subcortical zone of rarefaction. On radiography, the epiphysis may demonstrate fragmentation. Blood vessels within the epiphysis are incompetent because of thrombosis or microfractures of the trabeculae, which results in poor healing.
The third stage is the period of repair in which granulation tissue gradually replaces the necrotic tissue. Necrotic bone may lose its structural support, which results in compression and flattening of the articular surface.
Injury of the articular cartilage allows an influx of synovial fluid into the epiphysis, creating a subchondral cyst (see the images below). The subchondral cyst and increased joint pressure may prevent healing.
 Anteroposterior radiograph of the knee 1 year after injury reveals an anterior cruciate ligament reconstruction (arrowheads) and lucency (arrow) in the lateral tibial plateau.
Anteroposterior radiograph of the knee 1 year after injury reveals an anterior cruciate ligament reconstruction (arrowheads) and lucency (arrow) in the lateral tibial plateau.
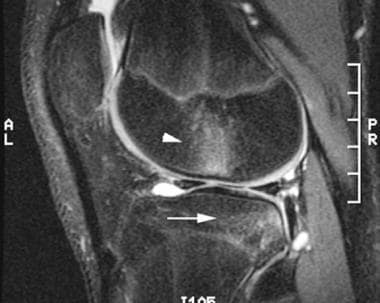 Sagittal T2-weighted image of the knee 2 weeks after injury demonstrates a kissing bone contusion in the lateral femoral condyle (arrowhead) and lateral tibial plateau (arrow).
Sagittal T2-weighted image of the knee 2 weeks after injury demonstrates a kissing bone contusion in the lateral femoral condyle (arrowhead) and lateral tibial plateau (arrow).
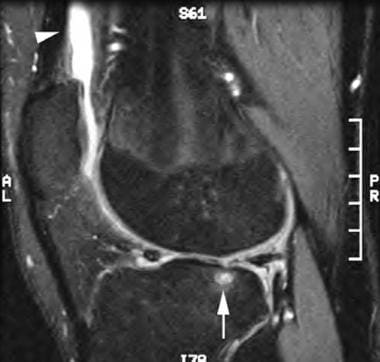 Sagittal T2-weighted image 1 year after injury reveals a subchondral cyst (arrow), an articular defect in the lateral tibial plateau, and a large knee effusion (arrowhead).
Sagittal T2-weighted image 1 year after injury reveals a subchondral cyst (arrow), an articular defect in the lateral tibial plateau, and a large knee effusion (arrowhead).
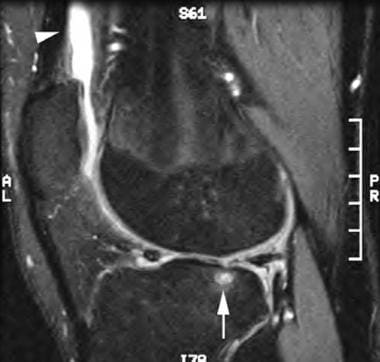
 Coronal T1-weighted image 1 year after injury demonstrates a subchondral cyst (arrowhead) in the lateral tibial plateau.
Coronal T1-weighted image 1 year after injury demonstrates a subchondral cyst (arrowhead) in the lateral tibial plateau.
Extreme obesity has also been strongly associated with an increased risk of OCD overall and OCD of the elbow and ankle specifically. In addition, moderate obesity is associated with an increased risk of knee OCD. All types of OCD were also found to have a significantly greater average BMI when compared with patients without OCD. [31]
Knee
In the knee joint, the medial femoral condyle is the most commonly involved site. Potential locations are the lateral aspect of the medial femoral condyle (75%), the weight-bearing surface of the medial (10%) and lateral femoral condyles (10%), and the anterior intercondylar groove or patella (5%). Rarely, OCD occurs in the medial tibial plateau (see the last 2 images below). [32, 33, 34, 35, 36, 5, 10, 37, 13]
See the images of OCD of the knee below.
 Anteroposterior radiograph of the knee reveals osteochondritis dissecans in the lateral aspect (arrowhead) of the medial femoral condyle.
Anteroposterior radiograph of the knee reveals osteochondritis dissecans in the lateral aspect (arrowhead) of the medial femoral condyle.
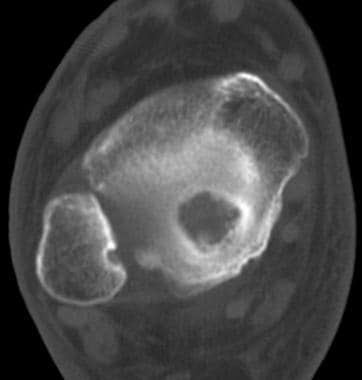
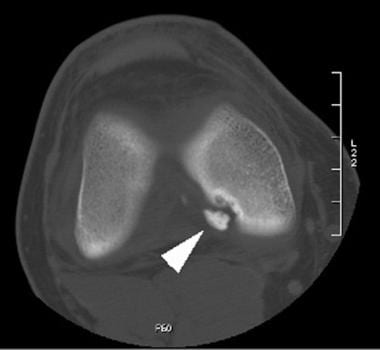 Axial CT of the knee demonstrates a completely detached osteochondral fracture (arrowhead) in the lateral aspect of the medial femoral condyle.
Axial CT of the knee demonstrates a completely detached osteochondral fracture (arrowhead) in the lateral aspect of the medial femoral condyle.
 Lateral radiograph of the knee reveals a calcified loose body (white arrowhead) in the infrapatellar fat pad and lucency in the articular surface of the patella (black arrowhead).
Lateral radiograph of the knee reveals a calcified loose body (white arrowhead) in the infrapatellar fat pad and lucency in the articular surface of the patella (black arrowhead).
 Sagittal T2-weighted image of the knee demonstrates a calcified loose body (white arrowhead) in the infrapatellar fat pad.
Sagittal T2-weighted image of the knee demonstrates a calcified loose body (white arrowhead) in the infrapatellar fat pad.
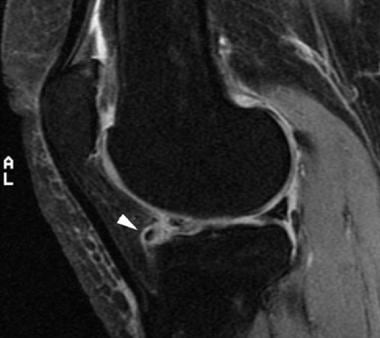
 Sagittal T2-weighted image of the knee reveals subchondral bone marrow edema (white arrowhead) and an articular cartilage defect in the patella.
Sagittal T2-weighted image of the knee reveals subchondral bone marrow edema (white arrowhead) and an articular cartilage defect in the patella.
 Coronal T1-weighted image of the knee demonstrates subchondral bone marrow edema (arrowhead) in the medial tibial plateau.
Coronal T1-weighted image of the knee demonstrates subchondral bone marrow edema (arrowhead) in the medial tibial plateau.
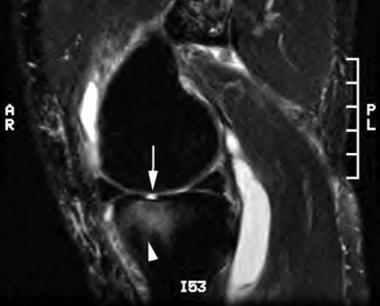 Sagittal T2-weighted image of the knee reveals an articular defect (arrow) and subchondral bone marrow edema (arrowhead) in the medial tibial plateau.
Sagittal T2-weighted image of the knee reveals an articular defect (arrow) and subchondral bone marrow edema (arrowhead) in the medial tibial plateau.
T1-weighted sequences allow a detailed analysis of the bone signal. T2-weighted sequences with fat-signal suppression are preferable over proton density-weighted sequences, because the latter are less specific for detecting fluid at the epiphyseal bone interface. Three-dimensional gradient echo sequences with various fat suppression techniques provide a detailed assessment of the cartilage and differentiate the epiphyseal cartilage from the surface cartilage by showing a thin low-signal line between the layers. [37]
Elbow
In the elbow joint, the most common site of OCD is the anterolateral aspect of the capitellum. OCD of the elbow is a subchondral bone lesion without evidence of acute trauma and is characterized by various degrees of osseous collapse, resorption, and sequestrum formation, which often involves articular cartilage delamination. [38] It is typically found in young athletes involved in overhead-throwing sports, such as baseball, at a time when the epiphyseal growth plate is open. [39, 40, 8, 14, 41, 42, 24]
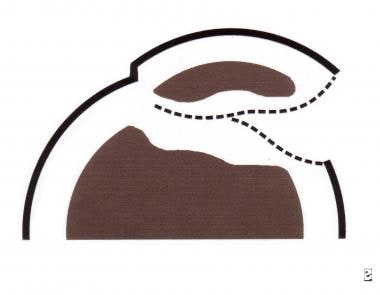
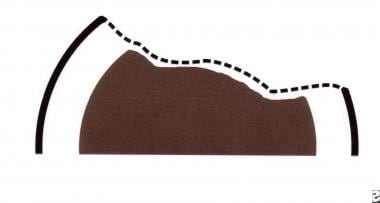
The causes of OCD of the elbow are regarded as multifactorial; they include repetitive valgus stress applied to the poorly vascularized capitellum, vascular inflammation, and genetic factors. [43] Singer and Roy proposed that repeated valgus stress and a tenuous blood supply within the capitellum explain the frequent occurrence of OCD in this location. [44] In a cadaveric study of the articular surfaces of the radiocapitellar joint, Schenck et al demonstrated significant topographic differences in the mechanical properties and thickness of cartilage in the capitellum and radial head. [45] Disparity in the mechanical properties of the central radial head and lateral capitellum probably is a factor in the initiation and localization of OCD of the capitellum (see the images below). [46, 6]
 Drawing of osteochondritis dissecans of the capitellum with localized subchondral bony flattening and a normal articular surface.
Drawing of osteochondritis dissecans of the capitellum with localized subchondral bony flattening and a normal articular surface.
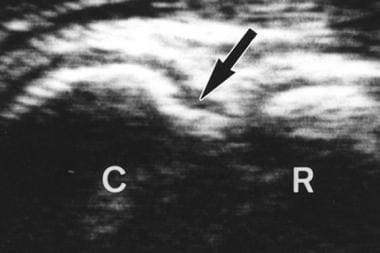
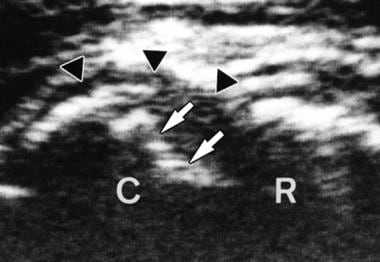 Anterior longitudinal sonogram reveals a stable lesion with localized subchondral bony flattening (arrows) and a normal outline of the articular cartilage (courtesy of Dr Masatoshi Takahara).
Anterior longitudinal sonogram reveals a stable lesion with localized subchondral bony flattening (arrows) and a normal outline of the articular cartilage (courtesy of Dr Masatoshi Takahara).
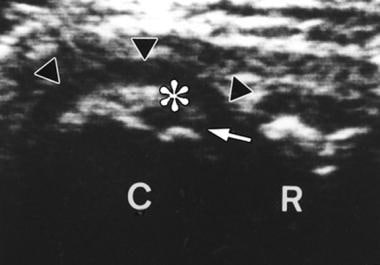 Posterior longitudinal sonogram demonstrates a stable lesion with a nondisplaced bone fragment (asterisk), intact articular surface (arrowheads), and a narrow gap formation (arrow; courtesy of Dr Masatoshi Takahara).
Posterior longitudinal sonogram demonstrates a stable lesion with a nondisplaced bone fragment (asterisk), intact articular surface (arrowheads), and a narrow gap formation (arrow; courtesy of Dr Masatoshi Takahara).
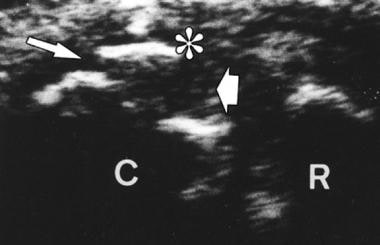 Posterior longitudinal sonogram reveals an unstable lesion with a slightly displaced fragment (asterisk) and a wide gap formation (arrows; courtesy of Dr Masatoshi Takahara).
Posterior longitudinal sonogram reveals an unstable lesion with a slightly displaced fragment (asterisk) and a wide gap formation (arrows; courtesy of Dr Masatoshi Takahara).
 Anterior longitudinal sonogram demonstrates an unstable lesion with a capitellar defect (arrow; courtesy of Dr Masatoshi Takahara).
Anterior longitudinal sonogram demonstrates an unstable lesion with a capitellar defect (arrow; courtesy of Dr Masatoshi Takahara).
Ankle
In the ankle joint, OCD occurs more frequently in the talus (see the first 9 images below) than in the tibial plafond (see the last 4 images below) and is 4-14 times more common. [11, 47] Disparity in frequency results from the biomechanical topography of the human ankle cartilage, since tibial cartilage is stiffer than talar cartilage. The usual sites of OCD of the talar dome are the posteromedial aspect (56%) and the anterolateral aspect (44%) of the talus. Occasionally, mirror-image osteochondral defects of the talus and distal tibia occur, suggesting trauma as a potential cause of both lesions. [4, 48, 49, 50, 51, 52, 53, 54]
 Anteroposterior radiograph of the leg reveals osteochondritis dissecans in the medial talar dome (arrowhead).
Anteroposterior radiograph of the leg reveals osteochondritis dissecans in the medial talar dome (arrowhead).
 Lateral radiograph of the leg demonstrates osteochondritis dissecans in the posterior aspect of the talar dome (arrowhead).
Lateral radiograph of the leg demonstrates osteochondritis dissecans in the posterior aspect of the talar dome (arrowhead).
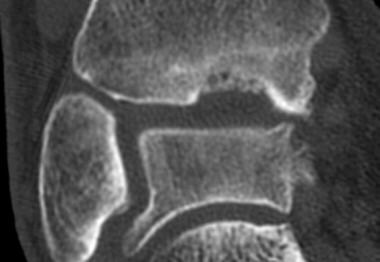
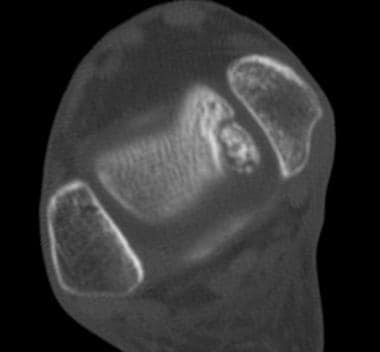 Axial CT of the ankle reveals osteochondritis dissecans in the posteromedial aspect of the talar dome.
Axial CT of the ankle reveals osteochondritis dissecans in the posteromedial aspect of the talar dome.
 Mortise view of the ankle demonstrates a linear calcified loose body (arrowhead) in the talofibular joint and lucency in the lateral talar dome (arrow).
Mortise view of the ankle demonstrates a linear calcified loose body (arrowhead) in the talofibular joint and lucency in the lateral talar dome (arrow).
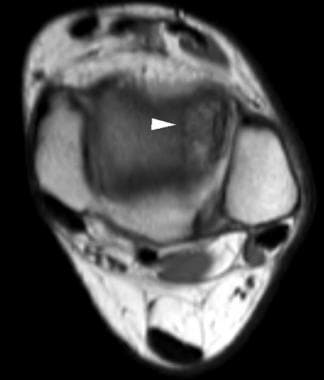 Axial T1-weighted image at the level of the ankle joint demonstrates abnormal low-signal intensity in the anterolateral aspect of the talus (arrowhead).
Axial T1-weighted image at the level of the ankle joint demonstrates abnormal low-signal intensity in the anterolateral aspect of the talus (arrowhead).
 Coronal T2-weighted image demonstrates an articular defect and abnormal high-signal intensity in the lateral talar dome consistent with osteochondritis dissecans.
Coronal T2-weighted image demonstrates an articular defect and abnormal high-signal intensity in the lateral talar dome consistent with osteochondritis dissecans.
 Lateral view of the ankle reveals loss of the sharp cortical line (arrowhead) in the posterior aspect of the tibial plafond.
Lateral view of the ankle reveals loss of the sharp cortical line (arrowhead) in the posterior aspect of the tibial plafond.
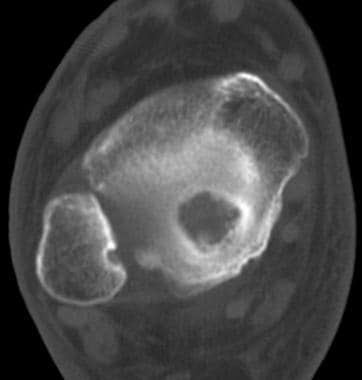 Axial CT at the level of the ankle joint demonstrates lytic defect in the central and posterior portions of the tibial plafond.
Axial CT at the level of the ankle joint demonstrates lytic defect in the central and posterior portions of the tibial plafond.
Tarsal navicular
Occasionally, OCD of the tarsal navicular (see the images below) is seen on ankle radiographs. Osteochondral fracture of the tarsal navicular is not as rare as previously reported in the radiologic literature. Radiographic findings can be subtle and, in some patients, may mimic Mueller-Weiss syndrome or stress fracture of the tarsal navicular. CT or MRI helps confirm the diagnosis. OCD of the tarsal navicular is limited to the proximal articular surface. Tarsal navicular OCD does not demonstrate the classic radiographic appearance of Mueller-Weiss syndrome, which includes comma-shaped deformity of the navicular resulting from collapse of the lateral portion of the bone, bipartite navicular resulting from fracture, or protrusion of portions of the bone or the entire navicular bone, medially or dorsally. In addition, tarsal OCD does not demonstrate either partial or complete sagittal fracture line on CT or MRI. [12]
 Lateral radiograph of the ankle reveals a cortical depression and loss of the sharp cortical line in the proximal articular surface of the tarsal navicular (arrowhead).
Lateral radiograph of the ankle reveals a cortical depression and loss of the sharp cortical line in the proximal articular surface of the tarsal navicular (arrowhead).
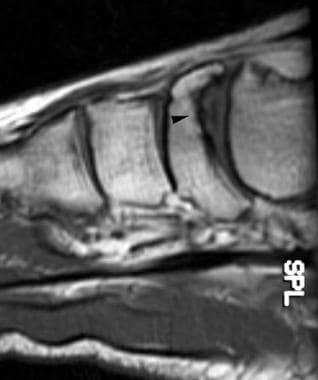 Sagittal T1-weighted image of the ankle confirms osteochondritis dissecans of the tarsal navicular (arrowhead).
Sagittal T1-weighted image of the ankle confirms osteochondritis dissecans of the tarsal navicular (arrowhead).
 Coronal T2-weighted image of the ankle reveals a central depression in the tarsal navicular (arrowhead) consistent with osteochondritis dissecans.
Coronal T2-weighted image of the ankle reveals a central depression in the tarsal navicular (arrowhead) consistent with osteochondritis dissecans.
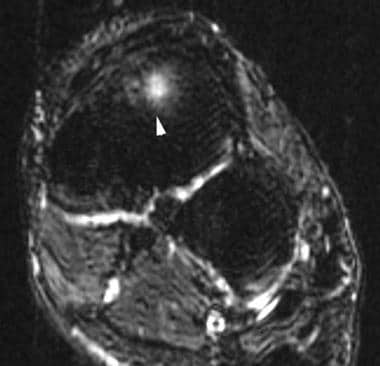
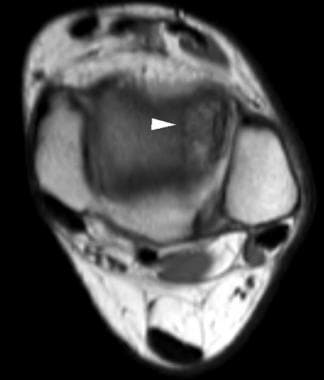
 Axial T2-weighted image of the ankle demonstrates subchondral bone marrow edema (arrowhead) in the proximal aspect of the tarsal navicular.
Axial T2-weighted image of the ankle demonstrates subchondral bone marrow edema (arrowhead) in the proximal aspect of the tarsal navicular.
Hip joint
In the hip joint, OCD occurs overwhelmingly in the femoral capital epiphysis. Only case reports exist of patients with OCD of the acetabulum. Many patients with OCD of the femoral capital epiphysis have a prior history of Legg-Calve-Perthes Disease. OCD is observed in approximately 3% of adults who had Legg-Calvé-Perthes disease as children. However, this complication cannot be predicted during the early stages of the Legg-Calvé-Perthes process and may present years later. [50, 55, 56, 57, 58]
Shoulder joint
OCD rarely occurs in the shoulder joint, where it involves either the humeral head or the glenoid. In 7 patients with OCD of the humeral head (all males ranging in age from 12 to 44 year), 5 of the patients (71%) demonstrated lesions in the right shoulder, suggesting an association with right-handedness. Locations of involvement were the anterosuperior, posterosuperior, posteromedial, superior, and medio-inferior aspects of the humeral head. [59, 22, 60, 61]
Glenoid
OCD of the glenoid is best detected on MRI. A developmental defect of the glenoid is a normal variant that may be mistaken for OCD of the glenoid (see the first 2 images below). Developmental defect of the glenoid is a small focal defect within the center of the glenoid and without associated subchondral bone marrow edema. OCD of the glenoid is usually a much larger and eccentrically located lesion (see the last 4 images below).
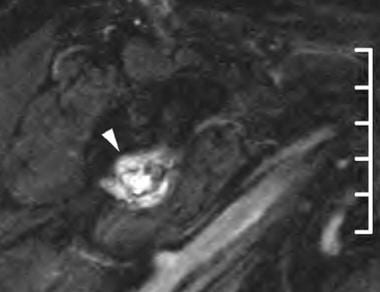
 Oblique, coronal T2-weighted image of the right shoulder demonstrates a developmental defect in the glenoid filled with fluid (arrowhead). Note the central location and absence of subchondral bone marrow edema. This is a normal variant. [49]
Oblique, coronal T2-weighted image of the right shoulder demonstrates a developmental defect in the glenoid filled with fluid (arrowhead). Note the central location and absence of subchondral bone marrow edema. This is a normal variant. [49]
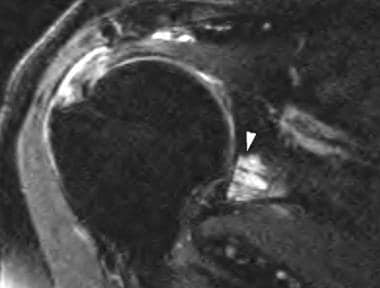
 Sagittal T2-weighted image of the right shoulder reveals a central depression within the glenoid (arrowhead) without associated subchondral bone marrow edema. This is a normal variant. [49]
Sagittal T2-weighted image of the right shoulder reveals a central depression within the glenoid (arrowhead) without associated subchondral bone marrow edema. This is a normal variant. [49]
 Oblique sagittal T2-weighted fat-suppression image reveals a large lesion in the anterior and inferior aspects of glenoid.
Oblique sagittal T2-weighted fat-suppression image reveals a large lesion in the anterior and inferior aspects of glenoid.
 Oblique coronal T1-weighted image demonstrates a hypointense lesion in the inferior half of the glenoid.
Oblique coronal T1-weighted image demonstrates a hypointense lesion in the inferior half of the glenoid.
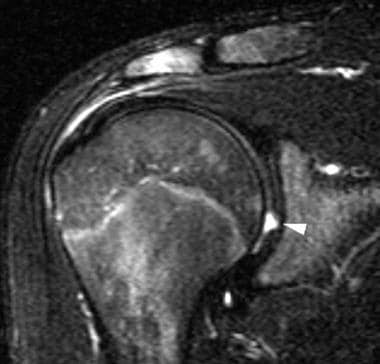
 Oblique coronal T2-weighted fat-suppression image demonstrates a hyperintense osteochondral lesion in the inferior half of the glenoid. Note the fluid in the subacromial/subdeltoid bursa and the supraspinatus tendon tear.
Oblique coronal T2-weighted fat-suppression image demonstrates a hyperintense osteochondral lesion in the inferior half of the glenoid. Note the fluid in the subacromial/subdeltoid bursa and the supraspinatus tendon tear.
Wrist joint
OCD of the wrist joint is rare and primarily occurs in the scaphoid. It may occur in either the distal or proximal pole and in either the distal or proximal articular surface of the scaphoid and may be bilateral. OCD of the scaphoid has been observed in bakers, boxers, pelota players, acrobats, and pneumatic drill workers, all of whom are subjected to repeated minor trauma of the wrist. [62, 63, 64, 65]
Classifications
Staging classifications of osteochondral lesions have been described best in the talus. Arthroscopic classifications of osteochondral lesions are the criterion standard. Two arthroscopic classifications of osteochondral lesions of the talus are the Pritsch and Cheng surgical classifications, which are based on the appearance of the overlying articular cartilage as seen on arthroscopy
The Pritsch arthroscopic staging of osteochondral lesions of the talus is as follows [66] :
-
Grade I - Intact, firm, shiny articular cartilage
-
Grade II - Intact but soft articular cartilage
-
Grade III - Frayed articular cartilage
The Cheng arthroscopic staging of osteochondral lesions of the talus is as follows [67] :
-
Grade A - Articular cartilage is smooth and intact but may be soft or ballottable
-
Grade B - Articular cartilage has a rough surface
-
Grade C - Articular cartilage has fibrillations or fissures
-
Grade D - Articular cartilage with a flap or exposed bone
-
Grade E - Loose, nondisplaced osteochondral fragment
-
Grade F - Displaced osteochondral fragment
Radiographic findings correspond with arthroscopic staging in 56% of patients, because fibrosis may provide stability in osseous separation. MRI correlates best with surgical staging. Differentials include Brodie abscess, chondroblastoma, enchondroma, and geode.
Radiography
On conventional radiographs, osteochondral lesions may appear normal. When detectable, osteochondral lesions appear as lucencies in the articular epiphysis. Osteochondritis dissecans is suggested by a loss of the sharp cortical line of the articular surface (see the images below). [4, 5, 6, 8, 10, 9]
 Lateral radiograph of the knee reveals a calcified loose body (arrowhead) posterior to the knee and lucency (arrow) in the articular surface of the patella.
Lateral radiograph of the knee reveals a calcified loose body (arrowhead) posterior to the knee and lucency (arrow) in the articular surface of the patella.
 Anteroposterior radiograph of the knee 1 year after injury reveals an anterior cruciate ligament reconstruction (arrowheads) and lucency (arrow) in the lateral tibial plateau.
Anteroposterior radiograph of the knee 1 year after injury reveals an anterior cruciate ligament reconstruction (arrowheads) and lucency (arrow) in the lateral tibial plateau.
 Anteroposterior radiograph of the knee reveals osteochondritis dissecans in the lateral aspect (arrowhead) of the medial femoral condyle.
Anteroposterior radiograph of the knee reveals osteochondritis dissecans in the lateral aspect (arrowhead) of the medial femoral condyle.
 Anteroposterior radiograph of the leg reveals osteochondritis dissecans in the medial talar dome (arrowhead).
Anteroposterior radiograph of the leg reveals osteochondritis dissecans in the medial talar dome (arrowhead).
 Lateral view of the ankle reveals loss of the sharp cortical line (arrowhead) in the posterior aspect of the tibial plafond.
Lateral view of the ankle reveals loss of the sharp cortical line (arrowhead) in the posterior aspect of the tibial plafond.
 Lateral radiograph of the ankle reveals a cortical depression and loss of the sharp cortical line in the proximal articular surface of the tarsal navicular (arrowhead).
Lateral radiograph of the ankle reveals a cortical depression and loss of the sharp cortical line in the proximal articular surface of the tarsal navicular (arrowhead).
The Berndt and Harty radiographic classification of osteochondral lesions of the talus is as follows [68] :
-
Stage I - Normal radiograph (subchondral compression fracture of the talus with no ligamentous sprain)
-
Stage II - Partially detached osteochondral fragment
-
Stage III - Complete, nondisplaced fracture remaining within the bony crater
-
Stage IV - Detached, loose osteochondral fragment
Computed Tomography
In the ankle joint, helical CT has multiplanar capability. CT is obtained in the direct axial and coronal planes at 1.5-mm-slice thickness with sagittal reformations (see the images below). Cystic lesion of the talar dome, cortical depression, or a loose bony fragment within the osteochondral defect may be demonstrated. [11, 12, 9] The shortcomings of CT are applied radiation, especially in pediatric patients, and lack of cartilage visualization. The lack of cartilage visualization can be overcome by using intra-articular contrast material. CT scans can be used to assess the osseous integration after refixation of OCD loose fragments. [13]
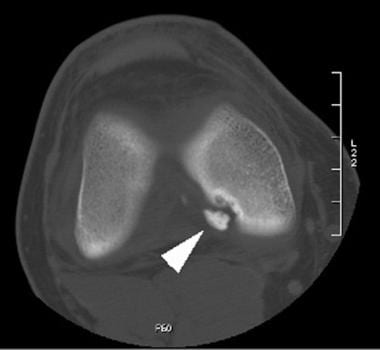 Axial CT of the knee demonstrates a completely detached osteochondral fracture (arrowhead) in the lateral aspect of the medial femoral condyle.
Axial CT of the knee demonstrates a completely detached osteochondral fracture (arrowhead) in the lateral aspect of the medial femoral condyle.
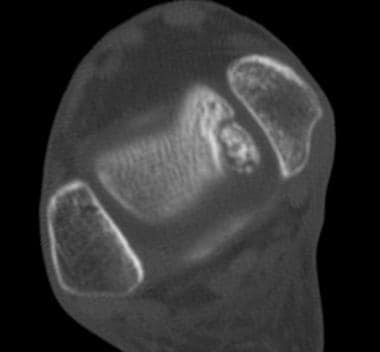 Axial CT of the ankle reveals osteochondritis dissecans in the posteromedial aspect of the talar dome.
Axial CT of the ankle reveals osteochondritis dissecans in the posteromedial aspect of the talar dome.
 Axial CT at the level of the ankle joint demonstrates lytic defect in the central and posterior portions of the tibial plafond.
Axial CT at the level of the ankle joint demonstrates lytic defect in the central and posterior portions of the tibial plafond.
The Ferkel and Sgaglione CT classification of osteochondral lesions of the talus is as follows [50] :
-
Stage I - Cystic lesion of the talar dome with an intact roof
-
Stage IIa - Cystic lesion with communication to the talar dome surface
-
Stage IIb - Open articular surface lesion with an overlying, nondisplaced fragment
-
Stage III - Nondisplaced lesion with lucency
-
Stage IV - Displaced osteochondral fragment
Magnetic Resonance Imaging
MRI detects radiographically occult lesions that may not be detected on CT. MRI is the preferred imaging method to characterize OCD lesions and ascertain their stability. In patients with capitellar OCD, MRI is particularly helpful for identifying cartilaginous foreign bodies that are usually missed by plain radiographs. [16] A short tau-inversion recovery sequence is the most sensitive. [16, 39, 46, 69, 70, 17, 18, 15, 19, 20, 21]
T1-weighted sequences allow a detailed analysis of the bone signal. T2-weighted sequences with fat-signal suppression are preferable over proton density-weighted sequences, because the latter are less specific for detecting fluid at the epiphyseal-bone interface. Three-dimensional gradient echo sequences with fat suppression provide clear assessment of the cartilage and differentiate the epiphyseal cartilage from the surface cartilage with a thin low signal line between the layers. [37]
Kijowski et al retrospectively compared the sensitivity and specificity of previously described MRI criteria for the detection of instability in patients with juvenile or adult osteochondritis dissecans of the knee, with arthroscopic findings as the reference standard. The authors concluded from their findings that previously described MR imaging criteria for OCD instability have high specificity for adult but not juvenile lesions of the knee. [71, 71]
Satake et al found that MRI had a sensitivity of 84% for OCD, [14] and Itsubo et al found 100% sensitivity and 80% specificity. [15]
(See the images below.)
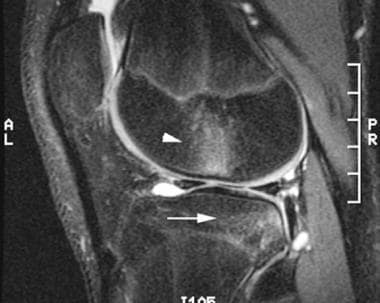 Sagittal T2-weighted image of the knee 2 weeks after injury demonstrates a kissing bone contusion in the lateral femoral condyle (arrowhead) and lateral tibial plateau (arrow).
Sagittal T2-weighted image of the knee 2 weeks after injury demonstrates a kissing bone contusion in the lateral femoral condyle (arrowhead) and lateral tibial plateau (arrow).
 Sagittal T2-weighted image 1 year after injury reveals a subchondral cyst (arrow), an articular defect in the lateral tibial plateau, and a large knee effusion (arrowhead).
Sagittal T2-weighted image 1 year after injury reveals a subchondral cyst (arrow), an articular defect in the lateral tibial plateau, and a large knee effusion (arrowhead).
 Coronal T1-weighted image 1 year after injury demonstrates a subchondral cyst (arrowhead) in the lateral tibial plateau.
Coronal T1-weighted image 1 year after injury demonstrates a subchondral cyst (arrowhead) in the lateral tibial plateau.
 Axial T1-weighted image at the level of the ankle joint demonstrates abnormal low-signal intensity in the anterolateral aspect of the talus (arrowhead).
Axial T1-weighted image at the level of the ankle joint demonstrates abnormal low-signal intensity in the anterolateral aspect of the talus (arrowhead).
 Coronal T2-weighted image demonstrates an articular defect and abnormal high-signal intensity in the lateral talar dome consistent with osteochondritis dissecans.
Coronal T2-weighted image demonstrates an articular defect and abnormal high-signal intensity in the lateral talar dome consistent with osteochondritis dissecans.
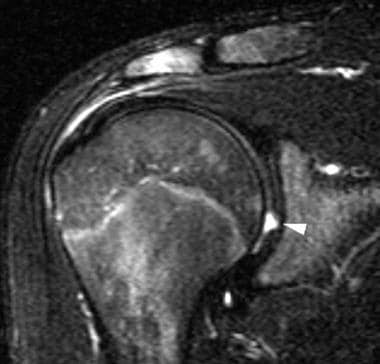 Oblique, coronal T2-weighted image of the right shoulder demonstrates a developmental defect in the glenoid filled with fluid (arrowhead). Note the central location and absence of subchondral bone marrow edema. This is a normal variant. [49]
Oblique, coronal T2-weighted image of the right shoulder demonstrates a developmental defect in the glenoid filled with fluid (arrowhead). Note the central location and absence of subchondral bone marrow edema. This is a normal variant. [49]
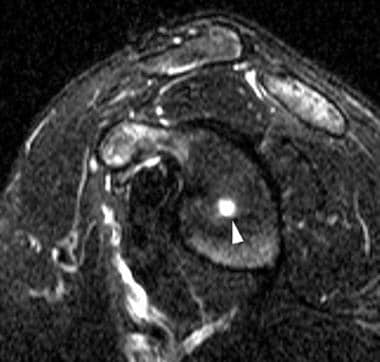 Sagittal T2-weighted image of the right shoulder reveals a central depression within the glenoid (arrowhead) without associated subchondral bone marrow edema. This is a normal variant. [49]
Sagittal T2-weighted image of the right shoulder reveals a central depression within the glenoid (arrowhead) without associated subchondral bone marrow edema. This is a normal variant. [49]
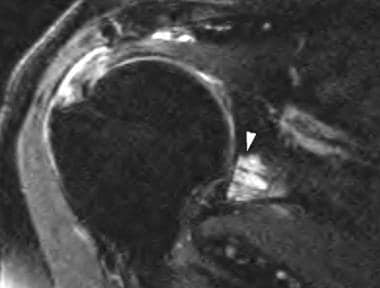 Oblique coronal T2-weighted fat-suppression image demonstrates a hyperintense osteochondral lesion in the inferior half of the glenoid. Note the fluid in the subacromial/subdeltoid bursa and the supraspinatus tendon tear.
Oblique coronal T2-weighted fat-suppression image demonstrates a hyperintense osteochondral lesion in the inferior half of the glenoid. Note the fluid in the subacromial/subdeltoid bursa and the supraspinatus tendon tear.
The Anderson MRI classification of osteochondral lesions of the talus is as follows [72] :
-
Stage I - Bone marrow edema (subchondral trabecular compression; radiograph results are negative with positive bone-scan findings)
-
Stage IIa - Subchondral cyst
-
Stage IIb - Incomplete separation of the osteochondral fragment
-
Stage III - Fluid around an undetached, undisplaced osteochondral fragment
-
Stage IV - Displaced osteochondral fragment
Griffith MRI classification of osteochondral lesions of the talus, showing the grade description of osteochondral lesions, is as follows [73] :
-
Grade 1a - Bone marrow change (edema, cystic change) with no collapse of subchondral bone area and no osteochondral junction separation and intact cartilage
-
Grade 1b - Similar to grade 1a, although with cartilage fracture
-
Grade 2a - Variable collapse of subchondral bone area with osteochondral separation through intact cartilage
-
Grade 2b - Similar to grade 2a, although with cartilage fracture
-
Grade 3a - Variable collapse of subchondral bone area with no osteochondral separation with or without variable cartilage hypertrophy
-
Grade 3b - Similar to grade 3a, although with cartilage fracture
-
Grade 4a - Separation within or at edge of bone component, with intact overlying cartilage
-
Grade 4b - Similar to grade 4a, although with cartilage fracture; unstable lesion, with level of instability related to extent of cartilage fracture
-
Grade 5 - Complete detachment of osteochondral lesion; unstable lesion
Grades 2b, 4b, and 5 are classified as unstable lesions of variable severity.
Ultrasonography
Ultrasonography has been used to evaluate osteochondritis dissecans of the knee and humeral capitellum (see the images below). The advantage of ultrasound is dynamic scanning with motion of the evaluated joint. In one study, sonographic assessment of OCD of the humeral capitellum agreed with radiographic assessment in 23 of 27 patients (85%), MRI assessment in 9 of 10 (90%), and surgical findings in 14 of 15 (93%). The sonographic appearance of OCD of the capitellum is as follows: stable—localized, subchondral bony flattening and normal articular surface; stable—lesion with nondisplaced osteochondral fragment; unstable—capitellar osteochondral defect with loose intra-articular fragment; unstable—lesion with slightly displaced osteochondral fragment. [74, 22, 20, 23, 24, 25, 26]
Kida et al reported 100% positive predictive value for ultrasound screening for OCD and suggested that a distinctive loss of the smooth articular surface on ultrasound was a good indicator of an osteochondral lesion. [75]
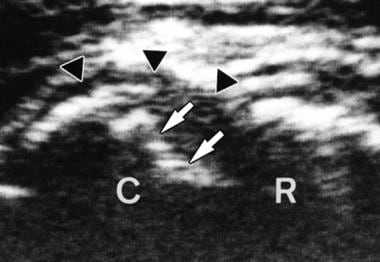 Anterior longitudinal sonogram reveals a stable lesion with localized subchondral bony flattening (arrows) and a normal outline of the articular cartilage (courtesy of Dr Masatoshi Takahara).
Anterior longitudinal sonogram reveals a stable lesion with localized subchondral bony flattening (arrows) and a normal outline of the articular cartilage (courtesy of Dr Masatoshi Takahara).
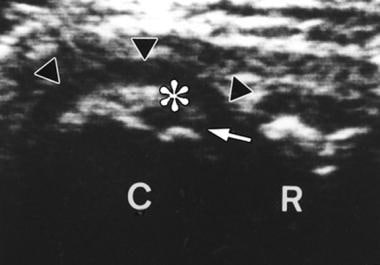 Posterior longitudinal sonogram demonstrates a stable lesion with a nondisplaced bone fragment (asterisk), intact articular surface (arrowheads), and a narrow gap formation (arrow; courtesy of Dr Masatoshi Takahara).
Posterior longitudinal sonogram demonstrates a stable lesion with a nondisplaced bone fragment (asterisk), intact articular surface (arrowheads), and a narrow gap formation (arrow; courtesy of Dr Masatoshi Takahara).
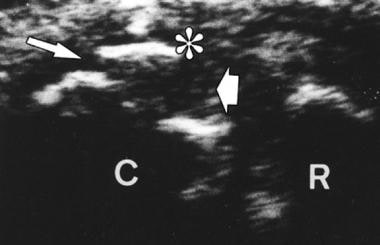 Posterior longitudinal sonogram reveals an unstable lesion with a slightly displaced fragment (asterisk) and a wide gap formation (arrows; courtesy of Dr Masatoshi Takahara).
Posterior longitudinal sonogram reveals an unstable lesion with a slightly displaced fragment (asterisk) and a wide gap formation (arrows; courtesy of Dr Masatoshi Takahara).
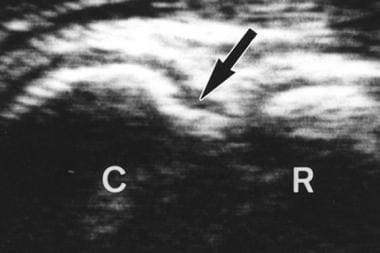 Anterior longitudinal sonogram demonstrates an unstable lesion with a capitellar defect (arrow; courtesy of Dr Masatoshi Takahara).
Anterior longitudinal sonogram demonstrates an unstable lesion with a capitellar defect (arrow; courtesy of Dr Masatoshi Takahara).
Nuclear Imaging
Scintigraphic findings are nonspecific, demonstrating a mild-to-marked increase in focal uptake in the involved bone, depending on the age of the osteochondritis dissecans. Dynamic bone scintigraphy is twice as sensitive as static scintigraphy in the detection of OCD of the femoral condyles. The scintigraphic appearance is probably a result of the slow repair process around an OCD, involving only the bone tissue surrounding the lesion, and is not a result of the OCD itself. [27, 28]
-
Lateral radiograph of the knee reveals a calcified loose body (arrowhead) posterior to the knee and lucency (arrow) in the articular surface of the patella.
-
Anteroposterior radiograph of the knee demonstrates lucency (arrow) in the central and superior aspect of the patella.
-
Anteroposterior radiograph of the knee is unremarkable.
-
Anteroposterior radiograph of the knee 1 year after injury reveals an anterior cruciate ligament reconstruction (arrowheads) and lucency (arrow) in the lateral tibial plateau.
-
Sagittal T2-weighted image of the knee 2 weeks after injury demonstrates a kissing bone contusion in the lateral femoral condyle (arrowhead) and lateral tibial plateau (arrow).
-
Sagittal T2-weighted image 1 year after injury reveals a subchondral cyst (arrow), an articular defect in the lateral tibial plateau, and a large knee effusion (arrowhead).
-
Coronal T1-weighted image 2 weeks after injury is unremarkable.
-
Coronal T1-weighted image 1 year after injury demonstrates a subchondral cyst (arrowhead) in the lateral tibial plateau.
-
Anteroposterior radiograph of the knee reveals osteochondritis dissecans in the lateral aspect (arrowhead) of the medial femoral condyle.
-
Axial CT of the knee demonstrates a completely detached osteochondral fracture (arrowhead) in the lateral aspect of the medial femoral condyle.
-
Lateral radiograph of the knee reveals a calcified loose body (white arrowhead) in the infrapatellar fat pad and lucency in the articular surface of the patella (black arrowhead).
-
Sagittal T2-weighted image of the knee demonstrates a calcified loose body (white arrowhead) in the infrapatellar fat pad.
-
Sagittal T2-weighted image of the knee reveals subchondral bone marrow edema (white arrowhead) and an articular cartilage defect in the patella.
-
Coronal T1-weighted image of the knee demonstrates subchondral bone marrow edema (arrowhead) in the medial tibial plateau.
-
Sagittal T2-weighted image of the knee reveals an articular defect (arrow) and subchondral bone marrow edema (arrowhead) in the medial tibial plateau.
-
Drawing of osteochondritis dissecans of the capitellum with localized subchondral bony flattening and a normal articular surface.
-
Drawing of osteochondritis dissecans of the capitellum with a nondisplaced osteochondral fragment.
-
Drawing of osteochondritis dissecans of the capitellum with a slightly displaced fragment.
-
Drawing of osteochondritis dissecans of the capitellum with a capitellar defect.
-
Anterior longitudinal sonogram reveals a stable lesion with localized subchondral bony flattening (arrows) and a normal outline of the articular cartilage (courtesy of Dr Masatoshi Takahara).
-
Posterior longitudinal sonogram demonstrates a stable lesion with a nondisplaced bone fragment (asterisk), intact articular surface (arrowheads), and a narrow gap formation (arrow; courtesy of Dr Masatoshi Takahara).
-
Posterior longitudinal sonogram reveals an unstable lesion with a slightly displaced fragment (asterisk) and a wide gap formation (arrows; courtesy of Dr Masatoshi Takahara).
-
Anterior longitudinal sonogram demonstrates an unstable lesion with a capitellar defect (arrow; courtesy of Dr Masatoshi Takahara).
-
Anteroposterior radiograph of the leg reveals osteochondritis dissecans in the medial talar dome (arrowhead).
-
Lateral radiograph of the leg demonstrates osteochondritis dissecans in the posterior aspect of the talar dome (arrowhead).
-
Axial CT of the ankle reveals osteochondritis dissecans in the posteromedial aspect of the talar dome.
-
Coronal CT of the ankle demonstrates a nondisplaced osteochondral fragment.
-
Sagittal reformatted image of the ankle reveals a nondisplaced osteochondral fragment.
-
Mortise view of the ankle demonstrates a linear calcified loose body (arrowhead) in the talofibular joint and lucency in the lateral talar dome (arrow).
-
Lateral view of the ankle reveals a linear calcified loose body (arrowhead).
-
Axial T1-weighted image at the level of the ankle joint demonstrates abnormal low-signal intensity in the anterolateral aspect of the talus (arrowhead).
-
Coronal T2-weighted image demonstrates an articular defect and abnormal high-signal intensity in the lateral talar dome consistent with osteochondritis dissecans.
-
Mortise view of the ankle reveals lucency in the central portion of the tibial plafond (arrowhead).
-
Lateral view of the ankle reveals loss of the sharp cortical line (arrowhead) in the posterior aspect of the tibial plafond.
-
Axial CT at the level of the ankle joint demonstrates lytic defect in the central and posterior portions of the tibial plafond.
-
Coronal CT of the ankle demonstrates a cortical depression in the tibial plafond.
-
Lateral radiograph of the ankle reveals a cortical depression and loss of the sharp cortical line in the proximal articular surface of the tarsal navicular (arrowhead).
-
Sagittal T1-weighted image of the ankle confirms osteochondritis dissecans of the tarsal navicular (arrowhead).
-
Coronal T2-weighted image of the ankle reveals a central depression in the tarsal navicular (arrowhead) consistent with osteochondritis dissecans.
-
Axial T2-weighted image of the ankle demonstrates subchondral bone marrow edema (arrowhead) in the proximal aspect of the tarsal navicular.
-
Oblique, coronal T2-weighted image of the right shoulder demonstrates a developmental defect in the glenoid filled with fluid (arrowhead). Note the central location and absence of subchondral bone marrow edema. This is a normal variant. [49]
-
Sagittal T2-weighted image of the right shoulder reveals a central depression within the glenoid (arrowhead) without associated subchondral bone marrow edema. This is a normal variant. [49]
-
Oblique sagittal T2-weighted fat-suppression image reveals a large lesion in the anterior and inferior aspects of glenoid.
-
Oblique coronal T1-weighted image demonstrates a hypointense lesion in the inferior half of the glenoid.
-
Oblique coronal T2-weighted fat-suppression image demonstrates a hyperintense osteochondral lesion in the inferior half of the glenoid. Note the fluid in the subacromial/subdeltoid bursa and the supraspinatus tendon tear.
-
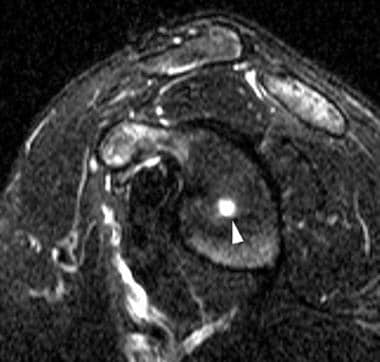
Axial-gradient recall image reveals an osteochondral lesion in the anterior half of the glenoid.