Practice Essentials
Mesenteric lymphadenitis (mesenteric adenitis) is a self-limited inflammatory process that affects the mesenteric lymph nodes in the right lower quadrant. Its clinical presentation mimics that of acute appendicitis. [1] Mesenteric lymphadenitis has been a reported finding in approximately a third of patients with multisystem inflammatory syndrome in children (MIS-C), a rare delayed, posinfectious complication of COVID-19. [2] MIS-C is associated with increased risk of hospitalization and ICU admission. [3]
Enlarged, hypoechoic mesenteric lymph nodes and the absence of a thickened blind-ending tubular structure (inflamed appendix) on ultrasonography is diagnostic of mesenteric adenitis. The distinction between normal and abnormal mesenteric lymph nodes by ultrasound is largely dependent on the size of the mesenteric lymph nodes, with at least one node measuring 8 mm or more in short-axis diameter. [4, 5]
Cross-sectional imaging is routinely applied in the examination of patients and may help avoid unnecessary surgery in cases of mesenteric lymphadenitis. Previously, the diagnosis was most frequently made when laparotomy performed to assess presumed appendicitis yielded negative findings. [6, 7, 8, 9, 10, 11]
(See images of mesenteric adenitis below.)
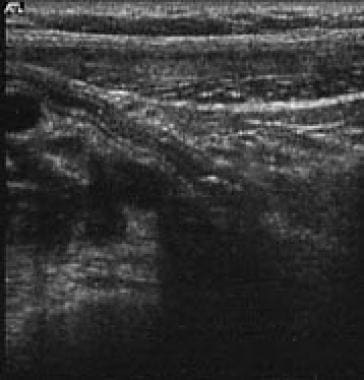
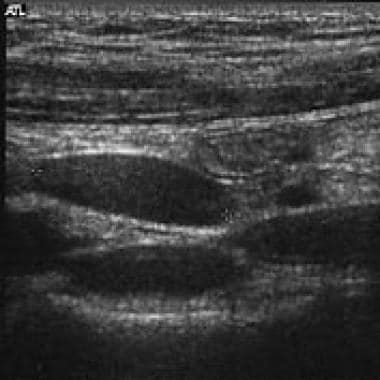
 Sonogram of normal mesenteric lymph nodes shows that they are ovoid, with a prominent fatty hilum and a short-axis diameter less than 5 mm.
Sonogram of normal mesenteric lymph nodes shows that they are ovoid, with a prominent fatty hilum and a short-axis diameter less than 5 mm.
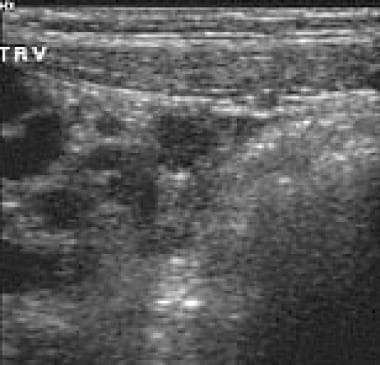
 A thickened ileum and cecum and a normal appendix are depicted adjacent to an enlarged lymph node in this patient with mesenteric adenitis and terminal ileocolitis.
A thickened ileum and cecum and a normal appendix are depicted adjacent to an enlarged lymph node in this patient with mesenteric adenitis and terminal ileocolitis.
Ultrasonography (see the images below) of the right lower quadrant with graded compression has been the mainstay of diagnosis in children. [12, 13, 14, 15, 16] The American College of Radiology (ACR) recommends this procedure as the most appropriate for children with intermediate clinical risk and pregnant women with fever and leukocytosis. [17, 18]
The ACR notes that abdominal CT (see the images below) with intravenous contrast may be useful as the initial imaging modality in children at high clinical risk for appendicitis. This technique is considered most appropriate in children when ultrasound findings are equivocal or nondiagnostic and when initial imaging or clinical suspicion points to complications such as abscess or bowel obstruction. [17] For adults, the ACR recommends this procedure as the most appropriate initial imaging modality for patients with right lower quadrant pain and for nonpregnant patients with fever, leukocytosis, and suspected appendicitis. [18] CT is especially useful for evaluation of possible appendicitis in men and in patients in whom visualization of the appendix may be compromised by body habitus.
Although the findings are frequently nonspecific, abdominal radiographs occasionally reveal findings and permit alternative diagnoses (eg, appendicoliths). [19, 20, 21]
In some centers, CT is performed for the evaluation of appendicitis without intravenous and/or oral contrast enhancement. This approach reduces the sensitivity of CT for bowel wall thickening and mesenteric adenopathy, especially in small children with a paucity of intraperitoneal fat.
The normal appendix is sonographically occult in a significant subset of patients. When lymph node enlargement is detected on sonographic examination in these patients, excluding appendicitis as a cause of reactive adenopathy is difficult. [19, 20]
With any imaging modality, the finding of lymph node enlargement as an isolated finding is nonspecific; it can be observed in association with several inflammatory processes. Occasionally, nodes exceeding the normal-size threshold are observed in children who have no demonstrable disease. [14, 21, 22]
In the context of concerns about the radiation dose associated with pediatric CT, tailoring the examination protocol to the patient is prudent to minimize exposure during studies for benign and self-limited conditions such as mesenteric lymphadenitis. In this respect, sonography is favored as the initial diagnostic test.
Radiography
Findings on supine and upright abdominal radiographs are often normal. Nonspecific findings include a regional ileus or evidence of bowel wall thickening in the right lower quadrant. Plain radiographic findings can never indicate a specific diagnosis in mesenteric adenitis, but they can occasionally confirm an alternative diagnosis. Cross-sectional imaging may be indicated regardless of the plain radiographic findings.
 Supine abdominal radiograph shows a mild localized ileus and suggests nodular thickening of the terminal ileum.
Supine abdominal radiograph shows a mild localized ileus and suggests nodular thickening of the terminal ileum.
Computed Tomography
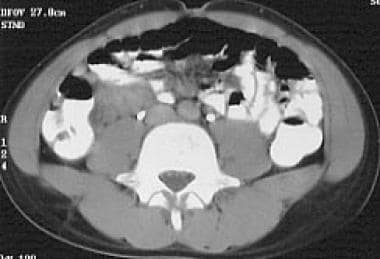
Diagnostic features on CT include enlarged mesenteric lymph nodes, with or without associated ileal or ileocecal wall thickening, in the setting of a normal appendix.
Rao et al specified the criterion of 3 or more nodes with a short-axis diameter of at least 5 mm, clustered in the right lower quadrant (see the images below). In the prospective study, none of the 18 patients with the aforementioned CT criterion had surgical or clinical evidence of appendicitis, whereas appendicitis was correctly diagnosed in 56. [23]
Further imaging is generally not indicated, although a definitive diagnosis might not be made in a case with equivocal findings until laparotomy performed for the evaluation of appendicitis reveals negative findings. Nonopacified bowel may be mistaken for enlarged lymph nodes, especially in thin patients or small children. Bowel wall thickness is difficult to determine in this setting.
Lymph nodes are generally larger, more numerous, and more widely distributed in mesenteric adenitis than in appendicitis. Ileal thickening is diagnosed when the wall is thicker than 3 mm over at least 5 cm of the bowel despite bowel lumen opacification and distention (see the image below).
 A thickened ileum and cecum and a normal appendix are depicted adjacent to an enlarged lymph node in this patient with mesenteric adenitis and terminal ileocolitis.
A thickened ileum and cecum and a normal appendix are depicted adjacent to an enlarged lymph node in this patient with mesenteric adenitis and terminal ileocolitis.
Ultrasonography
In patients with fever, abdominal tenderness, and a normal appendix, adenopathy that predominantly involves, but is not limited to, the right lower quadrant suggests the diagnosis (see the images below).
The definition of pathologic lymphadenopathy varies. Some studies suggest use of a longest diameter greater than 10 mm as pathologic, whereas some use the term mesenteric lymphadenitis only when the short‐axis diameter of the enlarged lymph node exceeds 10 mm. However, even small lymph nodes less than 5 mm in short‐axis diameter may be symptomatic. [24] Usually, 5 or more nodes are present and are often clustered. Nodal tenderness in response to transducer pressure is typical. Nodes are more rounded and hypoechoic than normal. Abnormal nodes have a short-axis diameter of at least 5 mm, and the diameter can exceed 1 cm. The nodes are typically larger and more numerous with mesenteric lymphadenitis than with appendicitis (see the images below). [14]
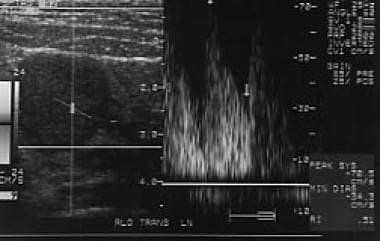
The demonstration of hyperemia within the node and surrounding mesentery with Doppler imaging is variably reported. Other findings include intestinal hyperperistalsis, which is seldom observed in appendicitis; nodular or circumferential thickening of the bowel wall; mesenteric thickening; fluid-filled loops; cecal involvement; and free fluid (see the images below). [25] Occasionally, a fluid-filled appendix is seen, but the lumen is readily compressible. [26]
Increased echogenicity of intra-abdominal fat has been reported as a nonspecific marker for right lower quadrant inflammatory disease, seen in appendicitis, mesenteric lymphadenitis, and other illnesses. [15] Similarly, increased echogenicity of renal parenchyma has been noted in children with mesenteric lymphadenitis, as well as appendicitis and other acute illness; it is a transient feature and does not necessarily indicate renal disease. [25]
Although nodal size and number are generally greater in mesenteric lymphadenitis than in appendicitis, overlap does occur. In Simonovsky's large series of 609 patients, 426 had appendicitis, and 81 had mesenteric lymphadenitis. [27] The inflamed appendix was missed in 2 of the latter cases.
Puylaert stated that in adult patients with right lower quadrant pain in whom the sole findings are enlarged mesenteric lymph nodes, the risk of appendicitis is 64%. [28] Therefore, the diagnosis of mesenteric lymphadenitis is hazardous when the appendix is not visualized; correlative CT may be beneficial in this setting.
In mesenteric lymphadenitis and lymphoma, the size, shape, distribution, and Doppler imaging characteristics of the lymph nodes overlap considerably, although the clinical context is useful in narrowing the differential diagnosis. [29]
Mesenteric lymph nodes that exceed the normal-size threshold may be visualized in the absence of disease, although these are usually nontender. Enlarged mesenteric lymph nodes can also be seen in giardiasis, Crohn disease, and AIDS. Lymph nodes that are matted, lack a normal hilum, or are massively enlarged may be signals of other conditions, such as tuberculosis, other mycobacterium infections, or lymphoma. Since viral gastroenteritis may clinically resemble appendicitis or mesenteric adenitis, consider evaluation of the proximal jejunum and terminal ileum for the presence of wall thickening that would suggest enteritis. [24]
Superb microvascular imaging
Superb microvascular imaging (SMI) has been studied in the pediatric population to diagnose mesenteric lymphadenitis. SMI aims to show low-velocity blood flow and small diameter blood vessel flow with better image resolution when compared to color Doppler flow imaging. Unlike conventional color and power Doppler imaging, SMI can suppress noise caused by motion artifacts without removing the weak signal arising from small vessel blood flow, hence potentially achieving greater sensitivity. With SMI, it is possible to visualize small vessels, including their branches, which has been possible only with contrast-enhanced imaging. [4, 30, 31, 5]
In a study by Zu et al of 27 children with lympadenitis, parameters of lymph node vascularity were compared using grayscale ultrasound, color Doppler flow imaging (CDFI), and SMI. SMI identified 92.6% of abnormal mesenteric lymph nodes, whereas CDFI detected 85.2%. US combined with SMI had the highest sensitivity (81.5%) and specificity (78.9%), compared with US alone (sensitivity, 63.0%; specificity, 64.9%) and compared with US combined with CDFI (sensitivity, 74.1%; specificity, 75.4%). [5]
Magnetic Resonance Imaging
MRI has emerged as an alternative for the evaluation of patients presenting with abdominal pain, because it has the safety-related advantage of avoiding exposure to ionizing radiation and because of its high sensitivity for inflammation without exposure to IV contrast medium. The expanding access to MRI has increased emergency department use as a primary cross-sectional imaging tool for suspected appendicitis, especially in children and pregnant women. [32]
Two separate systematic reviews and meta-analyses evaluating the accuracy of MRI for the diagnosis of acute appendicitis concluded that MRI has a high sensitivity (96-97%) and specificity (96%)—similar to that reported previously for CT. [33, 34]
When fat suppression is used, coronal contrast-enhanced sequences can be used for visualization of mesenteric lymphadenopathy. The balanced steady-state free precession sequence (called fast imaging employment steady-state acquisition on GE Healthcare systems, true fast imaging with steady-state precession on Siemens Healthcare systems, and balanced fast-field echo on Philips Healthcare systems) is relatively insensitive to motion and may be used as a primary sequence for patients with reduced compliance, such as pediatric patients and patients in severe pain. [35]
In a single institution review of MRI in the evaluation of 510 pediatric patients presenting with suspected appendicitis, mesenteric lymphadenitis was diagnosed in 2.2% of patients. [36]
-
Sonogram of normal mesenteric lymph nodes shows that they are ovoid, with a prominent fatty hilum and a short-axis diameter less than 5 mm.
-
Supine abdominal radiograph shows a mild localized ileus and suggests nodular thickening of the terminal ileum.
-
Abdominal CT scan shows a cluster of enlarged nodes in the right lower quadrant.
-
Mesenteric thickening associated with right lower quadrant adenopathy.
-
A thickened ileum and cecum and a normal appendix are depicted adjacent to an enlarged lymph node in this patient with mesenteric adenitis and terminal ileocolitis.
-
Typical sonographic appearance of a normal appendix.
-
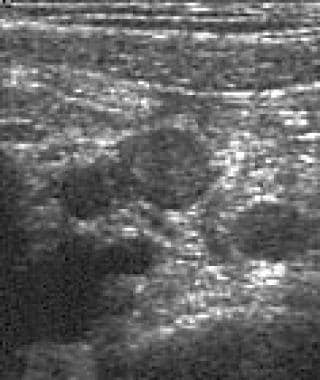
Typical sonographic appearance of a lymph node.
-
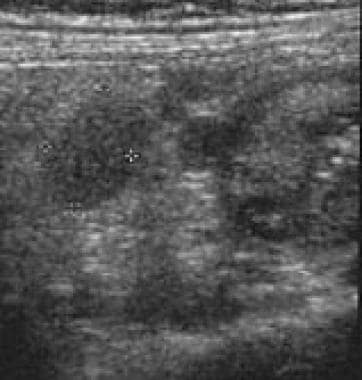
Lymph node clustering in the right lower quadrant.
-
Distended appendix with an appendicolith in acute appendicitis.
-
Reactive lymph nodes in acute appendicitis.
-
Color sonogram demonstrates nodal hyperemia.
-
Spectral Doppler sonogram demonstrates nodal hyperemia.
-
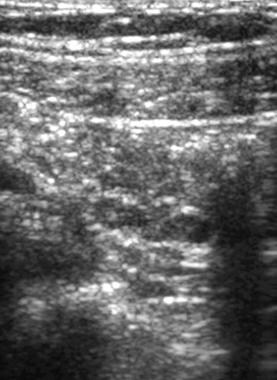
Circumferential thickening of the ileal wall and associated nodal enlargement.