Practice Essentials
Medullary sponge kidney (MSK) is a developmental abnormality occurring in the medullary pyramids of the kidney. MSK is characterized by cystic dilatation of the collecting tubules in one or more renal pyramids in one or both kidneys. MSK is found in approximately 0.5% of patients examined with excretory urography. The disease is often sporadic, rarely familial, and is shown to present bilaterally with a prevalence between 5/10,000 and 5/100,000. It typically presents between ages 20 and 30 years. The imaging gold standard is radiographic intravenous urography (IVU). Most patients remain asymptomatic, and MSK is detected incidentally on urograms unless it is complicated by infection, stone formation, or hematuria. Most cases are sporadic, but a few hereditary cases have been reported in the literature. MSK has also been documented in siblings and in several generations of families. [1] MSK is associated with nephrocalcinosis and recurrent calcium nephrolithiasis. MSK was regarded as a sporadic disorder, but 3 pedigrees have been described in which an apparently autosomal dominant inheritance is suggested. [2, 3]
(See the images below.)
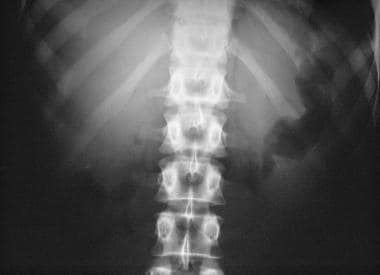 Control image from an intravenous urographic series in a 35-year-old woman who presented with painless hematuria. This plain radiograph shows bilateral tiny, rounded calcifications that correspond to the renal pyramids, which are suggestive of medullary sponge kidney.
Control image from an intravenous urographic series in a 35-year-old woman who presented with painless hematuria. This plain radiograph shows bilateral tiny, rounded calcifications that correspond to the renal pyramids, which are suggestive of medullary sponge kidney.
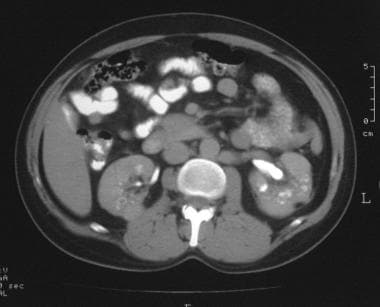
 Axial computed tomography scan of the kidneys in a 21-year-old woman with medullary sponge kidney. Delayed contrast-enhanced scan shows persistence of the contrast enhancement in the renal collecting tubules, a finding that is typical of medullary sponge kidney.
Axial computed tomography scan of the kidneys in a 21-year-old woman with medullary sponge kidney. Delayed contrast-enhanced scan shows persistence of the contrast enhancement in the renal collecting tubules, a finding that is typical of medullary sponge kidney.
Although it was first recognized by G Lenarduzzi in 1939, the thorough description of this condition resulted from the multidisciplinary cooperation among Lenarduzzi, a radiologist, and 2 of his colleagues at Padua University Hospital: Cacchi, a urologist, and Ricci, a pathologist; hence, MSK is also known as Lenarduzzi-Cacchi-Ricci disease. According to Gambaro et al, "These authors 'established' the paradigm for its diagnosis that is still used today." [4]
Although the pathogenesis of MSK has yet to be elucidated, its association with several developmental anomalies supports the idea that it is a developmental disorder. There are findings to suggest that MSK may be the consequence of a disruption of the ureteral-bud/metanephric-blastema interface. [4]
A study of Fabris et al provides strong evidence that familial clustering of MSK is common and has an autosomal dominant inheritance. The authors studied family members of 50 patients with MSK systematically by means of interviews, renal imaging, and biochemical studies in an effort to establish whether MSK is an inheritable disorder. The study found that patients with MSK had first- and second-degree relatives of both sexes with MSK in all generations. There were progressively lower mean levels of serum calcium, urinary sodium, pH, and volume, combined with higher serum phosphate and potassium, from patients with relatives with bilateral MSK, to those with unilateral MSK, and to those unaffected by MSK. The study suggests that most affected relatives have a milder form of MSK than nonaffected patients. Thus, it is important to keep the familial association in mind when investigating MSK. [5]
Preferred examination
Radiologically the diagnostic criteria are the presence of 3 or more linear or round collections of contrast within one or more renal papillae in the absence of obstruction. It can involve only one papilla or can be diffuse. [6] Mild cases give a striated appearance that is often referred to as a "brush." More marked dilations have been described as having the appearance of a "bouquet of flowers." [7]
Plain radiographs may demonstrate nephrocalcinosis. Although medullary sponge kidney cannot be diagnosed with the use of plain radiographic findings alone, the presence of linear and rounded medullary calcifications may suggest the diagnosis.
The principal method for diagnosing MSK is intravenous urography (IVU), in which discrete linear papillary densities, characteristic of MSK, are seen. [8, 9] Ultrasonographic (US) and computed tomography (CT) scan findings are more sensitive than plain radiographic findings in showing medullary calcifications, but they are less specific than IVU findings. CT scanning can be help confirm the presence of nephrocalcinosis when it is suggested on US images, and CT scans can demonstrate tubular ectasia. [10, 11, 12, 13, 14, 15]
The use of multidetector CT (MDCT) allows for rapid, high-resolution imaging with the capability of obtaining images with a slice thickness of 0.625 mm or less. Detailed reconstruction of the renal collecting system with MDCT urography equivalent to that of IVU has been demonstrated. MDCT urography can also detect related complications such as hydronephrosis, calculi, and pyelonephritis. [16]
The role of radioisotope uptake imaging is to assess renal function and to show the site of renal parenchymal scarring. MRI has a complementary role and is a useful alternative in patients who are allergic to iodinated contrast media. [17]
Radiography
Plain radiographic findings may be normal or may demonstrate nephrocalcinosis. This finding is characteristic of medullary sponge kidney (MSK), with several discrete pyramidal medullary calcifications occurring in clusters [18, 19] . When passed into the collecting systems, [8] calculi may be seen in the renal pelvis, ureter, or bladder. The renal size is usually normal, but the kidneys can be enlarged if the condition is associated with polycystic kidney disease.
IVU appearances depend on the type of tubular changes present. Changes form a spectrum that ranges from mild dilatation of the renal collecting tubules (often called renal tubular ectasia), which shows discrete linear opacities in one or more papillae through increasing severity of tubular dilatation and cystic changes, to gross deformities with multiple cyst and cystlike cavities of various sizes with beaded or striated cavities that extend through the pyramid from tip to base. The cystic collections of ectatic collecting ducts have been likened to "bunches of grapes" or "bouquets of flowers."
(Radiographic characteristics of medullary sponge kidney are demonstrated in the images below.)
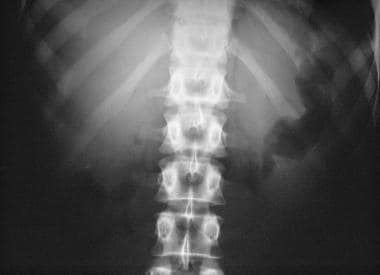 Control image from an intravenous urographic series in a 35-year-old woman who presented with painless hematuria. This plain radiograph shows bilateral tiny, rounded calcifications that correspond to the renal pyramids, which are suggestive of medullary sponge kidney.
Control image from an intravenous urographic series in a 35-year-old woman who presented with painless hematuria. This plain radiograph shows bilateral tiny, rounded calcifications that correspond to the renal pyramids, which are suggestive of medullary sponge kidney.
 Image from an intravenous urographic series in a 35-year-old woman who presented with painless hematuria (same patient as in the previous image). This radiograph was obtained at 15 minutes after the intravenous injection of contrast material and shows collection of the contrast agent in the ectatic renal collecting tubules.
Image from an intravenous urographic series in a 35-year-old woman who presented with painless hematuria (same patient as in the previous image). This radiograph was obtained at 15 minutes after the intravenous injection of contrast material and shows collection of the contrast agent in the ectatic renal collecting tubules.
 Plain abdominal radiograph in a 50-year-old woman with abdominal pain. The image shows bilateral nephrocalcinosis.
Plain abdominal radiograph in a 50-year-old woman with abdominal pain. The image shows bilateral nephrocalcinosis.
 Image from an intravenous urographic series in a 50-year-old woman with abdominal pain (same patient as in the previous image). This radiographic compression view of the kidneys was obtained at 15 minutes after the intravenous injection of contrast material and shows linear striations of contrast material that opacify the collecting tubules, giving a paintbrush-like appearance that is typical of medullary sponge kidney.
Image from an intravenous urographic series in a 50-year-old woman with abdominal pain (same patient as in the previous image). This radiographic compression view of the kidneys was obtained at 15 minutes after the intravenous injection of contrast material and shows linear striations of contrast material that opacify the collecting tubules, giving a paintbrush-like appearance that is typical of medullary sponge kidney.
 Plain abdominal radiograph in a 30-year-old woman who presented with renal failure. This scout radiograph shows clusters of multiple, tiny, rounded calcifications (arrow) that are more extensive in the lower pole calyx of the left kidney than elsewhere; this finding is consistent with medullary sponge kidney.
Plain abdominal radiograph in a 30-year-old woman who presented with renal failure. This scout radiograph shows clusters of multiple, tiny, rounded calcifications (arrow) that are more extensive in the lower pole calyx of the left kidney than elsewhere; this finding is consistent with medullary sponge kidney.
 Excretory urogram in a 30-year-old woman who presented with renal failure (same patient as in the previous image). This image was obtained after a delay of 6 hours and shows the persistent nephrogram of the poorly functioning left kidney.
Excretory urogram in a 30-year-old woman who presented with renal failure (same patient as in the previous image). This image was obtained after a delay of 6 hours and shows the persistent nephrogram of the poorly functioning left kidney.
 Plain abdominal radiograph in a 40-year-old man. This image shows extensive calculus formation in the medullary sponge kidney.
Plain abdominal radiograph in a 40-year-old man. This image shows extensive calculus formation in the medullary sponge kidney.
 Image from an intravenous urographic series in a 40-year-old man obtained after a 15-minute delay (same patient as in the previous image). This radiograph shows contrast agent accumulation in the collecting tubules.
Image from an intravenous urographic series in a 40-year-old man obtained after a 15-minute delay (same patient as in the previous image). This radiograph shows contrast agent accumulation in the collecting tubules.
 Plain abdominal radiograph in an adult man with medullary sponge kidney. No calcification is evident in the region of the kidneys.
Plain abdominal radiograph in an adult man with medullary sponge kidney. No calcification is evident in the region of the kidneys.
 Image from an intravenous urography series obtained after a 15-minute delay in an adult man with medullary sponge kidney (same patient as in previous image). Both kidneys are contracted predominantly on the right side. Note the accumulation of contrast agent in a cavity, reflecting a severe form (cystic) of medullary sponge kidney.
Image from an intravenous urography series obtained after a 15-minute delay in an adult man with medullary sponge kidney (same patient as in previous image). Both kidneys are contracted predominantly on the right side. Note the accumulation of contrast agent in a cavity, reflecting a severe form (cystic) of medullary sponge kidney.
 Conventional tomogram in an adult man (same patient as in the previous 2 images). This image clearly demonstrates pyramidal cysts and renal parenchymal scarring.
Conventional tomogram in an adult man (same patient as in the previous 2 images). This image clearly demonstrates pyramidal cysts and renal parenchymal scarring.
In patients with full-blown MSK, the calyces tend to be broad, shallow, distorted, and widely cupped. If calculi are present, they tend to be arranged in groups around a calyx, similar to a cluster of grapes or a bunch of flowers. Renal function decreases with subsequent poor depiction of the kidney. In view of the high incidence of nephrolithiasis in MSK, many patients have ureteral calculi. In these patients, the excretory urogram may show obstruction, calyceal distortion or destruction, and evidence of a urinary tract infection.
Degree of confidence
Plain radiographic findings of nephrocalcinosis are nonspecific. Nephrocalcinosis can occur in a variety of conditions, such as hyperparathyroidism, renal tubular acidosis, renal papillary necrosis, and primary hyperoxaluria, and in causes of hypercalcemia or hypercalciuria, such as milk-alkali syndrome, idiopathic hypercalciuria, sarcoidosis, and hypervitaminosis D. The absence of medullary nephrocalcinosis does not exclude MSK. Although a specific diagnosis of MSK cannot be made by using plain radiographic findings alone, the presence of a typical pattern of calcification suggests the diagnosis.
MSK is usually bilateral; however, if MSK is unilateral or segmental with localized tubular ectasia, the adjacent calyx must be evaluated for tumor or obstructing calculi. On the other hand, segmental MSK can mimic a renal mass. [20]
Benign tubular ectasia is a relatively common finding that can appear similar to MSK and can produce linear paintbrush-like striations arising from the medullary pyramids. However, unlike MSK, in benign tubular ectasia, there is no evidence of cystic dilatation in the tubules or of calcification formation, and there is no evidence to suggest that benign tubular ectasia progresses to MSK. The presence of medullary nephrocalcinosis is not necessary for a diagnosis of MSK if cystic dilatation of tubules is identified with IVU.
Computed Tomography
In medullary sponge kidney (MSK), unenhanced CT scan findings may be normal or demonstrate medullary nephrocalcinosis. Enhanced scans may demonstrate contrast accumulation within the papillae. [11, 14]
CT scans readily depict obstructive changes and help to identify complications, such as interstitial infection and abscess formation. [12]
Ill-defined areas of low attenuation that represent interstitial infection can readily be distinguished from normally enhancing renal parenchyma.
CT scans can also help in differentiating interstitial infection from abscess formation because abscesses appear as sharply defined, low-attenuation areas with thick walls. In addition, CT scans can help assess the perinephric extension of abscesses, and they can guide percutaneous drainage.
On MDCT, MSK presents with brushlike striations within the renal papillae, as well as cystic dilations of the distal tubules. [16] A study by Guany et al showed MDCT was diagnostic for MSK in 9 of 10 patients who were previously diagnosed by IVU. [16]
(CT scan characteristics of medullary sponge kidney are demonstrated in the images below.)
 Axial computed tomography scan of the kidneys in a 21-year-old woman with medullary sponge kidney. Delayed contrast-enhanced scan shows persistence of the contrast enhancement in the renal collecting tubules, a finding that is typical of medullary sponge kidney.
Axial computed tomography scan of the kidneys in a 21-year-old woman with medullary sponge kidney. Delayed contrast-enhanced scan shows persistence of the contrast enhancement in the renal collecting tubules, a finding that is typical of medullary sponge kidney.
 Nonenhanced computed tomography scan of the kidney demonstrates areas of low attenuation in the renal medulla that correspond to the area of cystic dilatation of the collecting tubules that was seen at intravenous urography. Note the bilateral, irregular renal outline.
Nonenhanced computed tomography scan of the kidney demonstrates areas of low attenuation in the renal medulla that correspond to the area of cystic dilatation of the collecting tubules that was seen at intravenous urography. Note the bilateral, irregular renal outline.
 Computed tomography image of the kidney obtained immediately after the intravenous administration of contrast agent (same patient as in the previous image). The nonenhanced medullary cysts are seen clearly against the background of enhancing renal cortex.
Computed tomography image of the kidney obtained immediately after the intravenous administration of contrast agent (same patient as in the previous image). The nonenhanced medullary cysts are seen clearly against the background of enhancing renal cortex.
 Delayed contrast-enhanced computed tomography image of the kidney in an adult man (same patient as in the previous 2 images). Note the gradual pooling of contrast agent in the cystlike collecting tubules.
Delayed contrast-enhanced computed tomography image of the kidney in an adult man (same patient as in the previous 2 images). Note the gradual pooling of contrast agent in the cystlike collecting tubules.
Degree of confidence
CT scan findings in patients with MSK are nonspecific. Although CT scanning has a limited role in evaluating patients with MSK, this imaging modality plays a significant role in evaluating complications such as infection or abscess formation, and CT scanning can be used to guide percutaneous drainage of these collections.
CT scanning may have some role in the evaluation of patients with MSK associated with microscopic calcification that cannot be seen on plain radiographs. However, CT scan findings can be negative despite microscopic calcification, as detected on histologic analysis. The accumulation of contrast material within the papillae can be seen in papillary blush. Segmental MSK can mimic a renal mass. Localized cystic dilatation associated with MSK can be seen in renal tuberculosis, renal papillary necrosis, and calyceal diverticula.
Ultrasonography
US findings demonstrate echogenic medullary pyramids in patients with medullary sponge kidney, irrespective of the presence of medullary nephrocalcinosis (see the image below). The echogenic medulla may cast acoustic shadowing. The increased echogenicity is seen in particular at the periphery of each pyramid between the interlobar cortices. US findings can demonstrate complications related to calculus disease.
 Sonogram of a kidney in a patient with medullary sponge kidney. This image shows a hyperechoic medulla associated with echogenic foci, some of which are casting shadows. A hyperechoic medulla can also be seen in conditions causing hyperuricemia and hypokalemia.
Sonogram of a kidney in a patient with medullary sponge kidney. This image shows a hyperechoic medulla associated with echogenic foci, some of which are casting shadows. A hyperechoic medulla can also be seen in conditions causing hyperuricemia and hypokalemia.
The sonographic appearances of MSK are nonspecific. Hyperechoic medulla with or without shadowing has been documented in gout, Sjogren syndrome, systemic lupus erythematosus, Lesch-Nyhan syndrome, hyperparathyroidism, infantile polycystic kidney disease, glycogen storage diseases, Wilson disease, primary aldosteronism, and pseudo-Bartter syndrome. In some patients, ultrasonography is more sensitive than plain radiography in detecting medullary calcification. [8]
-
Control image from an intravenous urographic series in a 35-year-old woman who presented with painless hematuria. This plain radiograph shows bilateral tiny, rounded calcifications that correspond to the renal pyramids, which are suggestive of medullary sponge kidney.
-
Image from an intravenous urographic series in a 35-year-old woman who presented with painless hematuria (same patient as in the previous image). This radiograph was obtained at 15 minutes after the intravenous injection of contrast material and shows collection of the contrast agent in the ectatic renal collecting tubules.
-
Plain abdominal radiograph in a 50-year-old woman with abdominal pain. The image shows bilateral nephrocalcinosis.
-
Image from an intravenous urographic series in a 50-year-old woman with abdominal pain (same patient as in the previous image). This radiographic compression view of the kidneys was obtained at 15 minutes after the intravenous injection of contrast material and shows linear striations of contrast material that opacify the collecting tubules, giving a paintbrush-like appearance that is typical of medullary sponge kidney.
-
Plain abdominal radiograph in a 30-year-old woman who presented with renal failure. This scout radiograph shows clusters of multiple, tiny, rounded calcifications (arrow) that are more extensive in the lower pole calyx of the left kidney than elsewhere; this finding is consistent with medullary sponge kidney.
-
Excretory urogram in a 30-year-old woman who presented with renal failure (same patient as in the previous image). This image was obtained after a delay of 6 hours and shows the persistent nephrogram of the poorly functioning left kidney.
-
Plain abdominal radiograph in a 40-year-old man. This image shows extensive calculus formation in the medullary sponge kidney.
-
Image from an intravenous urographic series in a 40-year-old man obtained after a 15-minute delay (same patient as in the previous image). This radiograph shows contrast agent accumulation in the collecting tubules.
-
Sonogram of a kidney in a patient with medullary sponge kidney. This image shows a hyperechoic medulla associated with echogenic foci, some of which are casting shadows. A hyperechoic medulla can also be seen in conditions causing hyperuricemia and hypokalemia.
-
Axial computed tomography scan of the kidneys in a 21-year-old woman with medullary sponge kidney. Delayed contrast-enhanced scan shows persistence of the contrast enhancement in the renal collecting tubules, a finding that is typical of medullary sponge kidney.
-
Plain abdominal radiograph in an adult man with medullary sponge kidney. No calcification is evident in the region of the kidneys.
-
Image from an intravenous urography series obtained after a 15-minute delay in an adult man with medullary sponge kidney (same patient as in previous image). Both kidneys are contracted predominantly on the right side. Note the accumulation of contrast agent in a cavity, reflecting a severe form (cystic) of medullary sponge kidney.
-
Conventional tomogram in an adult man (same patient as in the previous 2 images). This image clearly demonstrates pyramidal cysts and renal parenchymal scarring.
-
Nonenhanced computed tomography scan of the kidney demonstrates areas of low attenuation in the renal medulla that correspond to the area of cystic dilatation of the collecting tubules that was seen at intravenous urography. Note the bilateral, irregular renal outline.
-
Computed tomography image of the kidney obtained immediately after the intravenous administration of contrast agent (same patient as in the previous image). The nonenhanced medullary cysts are seen clearly against the background of enhancing renal cortex.
-
Delayed contrast-enhanced computed tomography image of the kidney in an adult man (same patient as in the previous 2 images). Note the gradual pooling of contrast agent in the cystlike collecting tubules.







