Practice Essentials
Hyperaldosteronism is characterized by excessive secretion of aldosterone, which causes increases in sodium reabsorption and loss of potassium and hydrogen ions. It may be either primary (autonomous) or secondary. Hyperaldosteronism represents part of a larger entity of hypermineralocorticoidism that may be caused by aldosterone, its mineralocorticoid precursors, or defects that modulate aldosterone effects on its target tissues. [1]
Primary aldosteronism, also termed Conn syndrome, is clinically characterized by hypertension, hypokalemia, and metabolic alkalosis. [2, 3, 4]
Guidelines, such as those by the Endocrine Society, recommend increased screening for primary aldosteronism in patients at greater risk, such as hypertensive patients with type 2 diabetes mellitus and those with obstructive sleep apnea. [5, 6, 7]
Adrenal venous sampling (AVS) is the gold standard to differentiate between unilateral and bilateral forms of primary aldosteronism, and cross-sectional CT imaging is an essential component of the workup for primary aldosteronism. CT provides reliable anatomic information regarding the bilateral adrenal glands and can exclude an adrenal cortical carcinoma. CT is fairly sensitive in detecting patients with a hypersecreting adenoma but not in confirming an aldosterone-secreting adenoma. [4, 8, 9]
Imaging modalities
The workup in patients in whom primary aldosteronism is suspected usually starts with appropriate biochemical analysis, after which thin-collimation CT imaging is performed. If CT scan findings are equivocal, radionuclide studies and MRI should be performed. If doubt concerning the diagnosis remains and if CT scans do not show a mass in the adrenal glands, adrenal venous sampling (AVS) is recommended. [10, 11, 12, 13, 14, 15, 16, 8, 9] Nunes et al found CT-guided percutaneous radiofrequency ablation was a safe and effective treatment for functioning adrenal adenomas, with short hospital length of stay and low complication rate. [17]
(See the hyperaldosteronism-related images below.)
 Longitudinal sonogram through the left kidney in a 32-year-old woman who presented with hypertension shows a 3-cm hypoechoic but solid mass superior to the upper pole of the kidney. Initially, the mass was regarded as a nonfunctioning adenoma unrelated to the patient's hypertension. Subsequently, mild hypokalemia developed. Surgical resection confirmed a tumor due to Conn syndrome.
Longitudinal sonogram through the left kidney in a 32-year-old woman who presented with hypertension shows a 3-cm hypoechoic but solid mass superior to the upper pole of the kidney. Initially, the mass was regarded as a nonfunctioning adenoma unrelated to the patient's hypertension. Subsequently, mild hypokalemia developed. Surgical resection confirmed a tumor due to Conn syndrome.
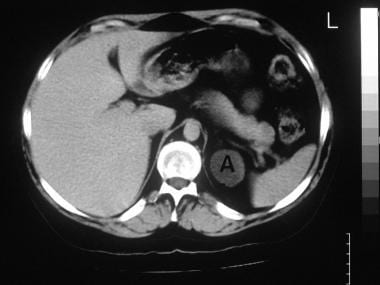 Axial enhanced CT scan in a 32-year-old woman who presented with hypertension shows a low-attenuating 2.8-cm suprarenal mass (A) (same patient as in previous image). Histologic results obtained after surgery confirmed a tumor due to Conn syndrome.
Axial enhanced CT scan in a 32-year-old woman who presented with hypertension shows a low-attenuating 2.8-cm suprarenal mass (A) (same patient as in previous image). Histologic results obtained after surgery confirmed a tumor due to Conn syndrome.
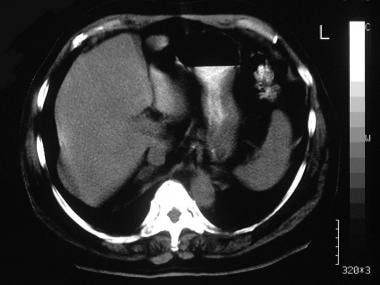
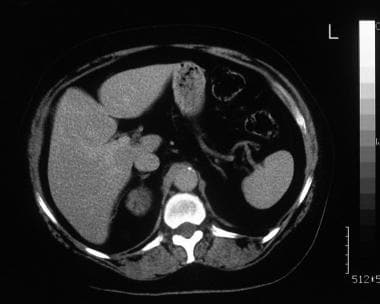
 Axial nonenhanced CT scan through the adrenal glands in 56-year-old man shows multiple nodules in both glands, although biochemical results indicated primary aldosteronism. The patient received medical treatment.
Axial nonenhanced CT scan through the adrenal glands in 56-year-old man shows multiple nodules in both glands, although biochemical results indicated primary aldosteronism. The patient received medical treatment.
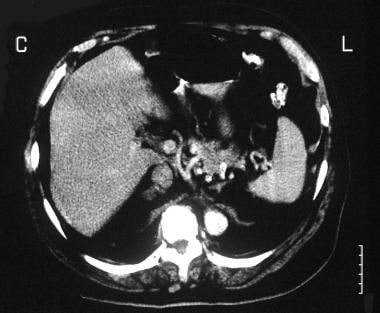
 Axial enhanced CT scan in a 56-year-old man shows no enhancement of the adrenal masses (same patient as in the previous image).
Axial enhanced CT scan in a 56-year-old man shows no enhancement of the adrenal masses (same patient as in the previous image).
Plain radiographs have no significant role. Ultrasonography has little to contribute unless the adrenal tumor is large, which is seldom the case. However, ultrasonography is an excellent modality for the investigation of hypertension.
Hypersecreting adrenal glands may appear to be normal in size on images, because the size of the adrenal gland may be compared to a normal measurement and because the healthy adrenal gland varies considerably in size. The adrenal glands also vary in size and weight as a result of illness or stress. This size discrepancy is a particular problem with aldosterone-producing adenomas (APAs), because they are often small and difficult to detect. In one series, the average diameter of an APA was 18 mm, and 20% of tumors were smaller than 1 cm.
SPECT/CT can identify small adenomas (0.8-1.5 cm) even in patients with chronic renal disease where the biochemical diagnosis of primary hyperaldosteronism is difficult.
Limitations of techniques
In earlier generations of CT scanners, the sensitivity for detecting APAs was 50-70%. With current CT scanners, the sensitivity has been improved to 82-88%. Diagnosis by using CT scans is hampered by the detection of ipsilateral or contralateral, nonfunctioning adenomas, which leads to a false-positive diagnosis of adrenal hyperplasia. CT scanning is not reliable in distinguishing between hyperplasia and adenoma in patients with multiple, bilateral nodules. [10, 18, 19, 20]
Anatomy
Since computed tomography (CT) scanning has become the standard technique in diagnostic adrenal imaging, differentiating normal from abnormal adrenal glands is essential. Normal adrenal glands are identified in almost all patients with the help of CT scans, whereas a normal left-sided gland is identified in 45% of patients and a normal right-sided gland is identified in 80% of patients with the help of ultrasonograms. [10, 18]
Cross-sectional images obtained by using CT scanning and MRI show the adrenal glands as thin, folded structures with an anteromedial ridge and 2 posterior or posterolateral limbs. These limbs, which appear winglike, are joined together at the superior aspect of the gland, placed at the upper pole of the kidney. Inferiorly, the limbs open, straddling the upper poles of the kidney. MRI scans can show the adrenal glands elegantly and in many planes. With standard CT scanning, only cross-sectional images may need to be interpreted. On the most cephalic CT scan section, the gland usually has a linear appearance with an anteroposterior orientation or a slanted, anterior-to-posterolateral orientation. [18, 21, 22, 23]
The midsections of the gland present a Y -shaped configuration. Occasionally, the anteromedial ridge is small or not well developed, resulting in an inverted, V -shaped gland. The normal adrenal limbs measure 3-6 mm in thickness, 4-6 cm in length, and 2-3 cm in width. The variation in size explains why some hyperfunctioning glands are seen to be normal in size on images and at surgery.
Computed Tomography
After a diagnosis of hyperaldosteronism has been established clinically and biochemically, dedicated CT scanning of the adrenal glands is performed using thin (3-mm) collimation. Nonenhanced and enhanced CT scans are obtained. [10, 14, 15, 18, 19, 20, 21, 24]
The mean attenuation level in adrenal adenomas is -2.2 HU. Among hyperfunctioning adenomas, aldosteronomas have the lowest attenuation levels. In patients with primary hyperaldosteronism, CT scan findings may be normal, or scans may show nodular or multinodular glands.
CT appears more reliable at revealing tumors larger than 1 cm. Conversely, 20% of tumors may be missed. In one series, the average diameter of an APA was 18 mm, and 20% of tumors were smaller than 1 cm. With earlier-generation CT scanners, the sensitivity for detecting aldosterone-producing adenomas was 50-70%. The sensitivity of current scanners has been improved to 82-88%. The specificity of CT scanning in the detection of APAs is 77%. [10, 18, 19, 20]
CT scan findings of ipsilateral or contralateral, nonfunctioning adenomas lead to a false-positive diagnosis of adrenal hyperplasia. CT scanning is not reliable in distinguishing hyperplasia from adenoma in patients with multiple, bilateral nodules.
(See the CT images below.)
 Axial nonenhanced CT scan through the adrenal glands in 56-year-old man shows multiple nodules in both glands, although biochemical results indicated primary aldosteronism. The patient received medical treatment.
Axial nonenhanced CT scan through the adrenal glands in 56-year-old man shows multiple nodules in both glands, although biochemical results indicated primary aldosteronism. The patient received medical treatment.
 Axial enhanced CT scan in a 56-year-old man shows no enhancement of the adrenal masses (same patient as in the previous image).
Axial enhanced CT scan in a 56-year-old man shows no enhancement of the adrenal masses (same patient as in the previous image).
 Axial nonenhanced CT scan through the adrenal glands in a 60-year-old patient who presented with hypertension and hypokalemia shows a bilobulated tumor in the right adrenal gland.
Axial nonenhanced CT scan through the adrenal glands in a 60-year-old patient who presented with hypertension and hypokalemia shows a bilobulated tumor in the right adrenal gland.
 Axial enhanced CT scan through the adrenal glands in a 60-year-old patient who presented with hypertension and hypokalemia shows minor tumor enhancement (same patient as in previous image). Note the normal left adrenal gland.
Axial enhanced CT scan through the adrenal glands in a 60-year-old patient who presented with hypertension and hypokalemia shows minor tumor enhancement (same patient as in previous image). Note the normal left adrenal gland.
 A 59-year-old man was referred for renal ultrasonography as a part of the workup for newly diagnosed hypertension. The sonogram depicted a 3-cm right adrenal mass, which was regarded as an incidentaloma (not shown). Axial enhanced CT scan through the adrenal gland shows minor patchy enhancement in a right adrenal tumor.
A 59-year-old man was referred for renal ultrasonography as a part of the workup for newly diagnosed hypertension. The sonogram depicted a 3-cm right adrenal mass, which was regarded as an incidentaloma (not shown). Axial enhanced CT scan through the adrenal gland shows minor patchy enhancement in a right adrenal tumor.
Magnetic Resonance Imaging
Early experience with MRI in the diagnosis of aldosterone-producing adenoma (APA) has been encouraging. APAs are isointense or hypointense relative to the liver on T1-weighted images; they are slightly hyperintense on T2-weighted images.
Chemical-shift imaging is a useful method for the characterization of adrenal masses. It is based on the principle that fat protons precess faster than do water protons. Chemical-shift MRI is highly sensitive and specific for the differentiation of benign from malignant adrenal tumors, because benign adrenal tumors contain fat, while malignant adrenal tumors rarely do. With chemical-shift imaging, the signal intensity has been found to decrease on out-of-phase images in 86% of patients with APAs and in 89% of patients with bilateral adrenal hyperplasia. [21, 22, 23]
A sensitivity of 70-100% and a specificity of 64-100% have been reported in the detection of APAs with MRI. [21, 22, 23] False-positive diagnoses have occurred in cases of idiopathic hyperaldosteronism, bilateral nodular hyperplasia, primary hypertension, and primary hypertension associated with nonfunctioning adrenal adenoma. [15]
Ultrasonography
Ultrasonograms may reveal a significantly sized aldosterone-producing adenoma (APA), but because APAs tend to be small, the overall sensitivity of ultrasonography is poor. Compared with the adrenal tumors in Cushing disease, larger APAs are easier to identify, because neither retroperitoneal nor subcutaneous fat is obtrusive, as it is with Cushing disease. Ultrasonographic findings contribute little to the diagnosis unless the adrenal tumor is large, which is seldom the case. However, ultrasonography is an excellent modality for the investigation of hypertension. The exact sensitivity of ultrasonography in the diagnosis of APA is not known, but it appears to be low. Similar to other types of cross-sectional imaging, ultrasonography may incidentally demonstrate nonfunctioning masses in the adrenal glands.
Nuclear Imaging
Iodine-131-6β-iodomethylnorcholesterol (NP-59) is a cholesterol analog that binds to low-density lipoprotein receptors of the adrenal cortex. [19] Imaging is usually performed after dexamethasone suppression to reduce high background tracer uptake by the zona fasciculata. The normal glands (which show uptake of the radionuclide) are identified on day 5 or thereafter. Early, bilateral depiction of the glands (that is, before day 5) implies adrenal hyperplasia, whereas early, unilateral early depiction implies an APA. Detection rate of aldosterone-producing adenomas (APAs) can be improved by using single-photon emission CT (SPECT) scanning. [20]
Primary aldosteronism must be clinically and biochemically diagnosed before the radionuclide study is performed, because secondary hyperaldosteronism produces bilateral tracer uptake that is indistinguishable from that of primary, autonomous, bilateral hyperplasia. In addition, all drugs that disturb the renin-angiotensin-aldosterone axis must be withdrawn before imaging. [20]
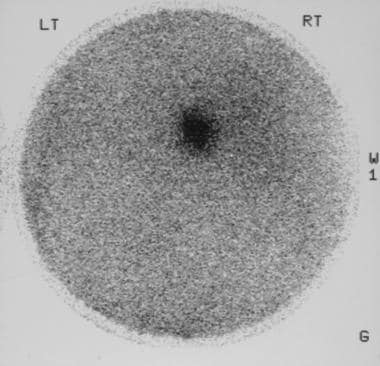
Scintigraphy (see the image below) must be performed in the appropriate clinical setting, because NP-59 uptake has been described in benign, nonsecretory adenoma, as well as in metastatic lung cancer, metastatic colon cancer, lymphoma, myelolipoma, ganglioneuroma, adrenal cysts, and adrenocortical carcinoma. Tracer uptake at extra-adrenal sites also has been reported. [20]
Angiography
Because aldosterone-producing adenomas (APAs) are small and are not usually vascular, selective adrenal angiography is seldom helpful. However, adrenal phlebography has a useful role in the investigation of APA, because the splaying of veins around APAs can help identify even small tumors. If contrast medium is refluxed into the veins of the APA, a wheel-spoke pattern is seen in the intratumoral veins. Because APAs are small, a vigorous retrograde venous injection is usually required to detect the tumors; this vigorous injection is not without risk, because extravasation may occur.
Extravasation is a particular problem if the catheter is wedged into the vein. Extravasation can be painful and has been associated with adrenal infarction. Adrenal vein thrombosis is also a known complication of adrenal phlebography, which has been linked to adrenal infarction. Adrenal insufficiency has been described as a result of bilateral adrenal infarction. Adrenal vein thrombosis is more likely to occur if the catheter is wedged in the adrenal vein and left there for several minutes during the procedure.
The most useful technique in the investigation of primary aldosteronism is adrenal venous sampling. [18, 21, 25] Blood samples are obtained from both adrenal veins for aldosterone level analysis; hormone level ratios are compared with each other and with levels in the inferior vena cava below the adrenal veins. In experienced hands, this technique can achieve a high sensitivity; however, it is a time-consuming procedure that necessitates prolonged cannulation of adrenal veins and increases the risk of adrenal vein thrombosis. In addition, the adrenal veins are small, and collecting 7 mL of blood for sampling is not easy. This is particularly a problem when blood is collected from the right adrenal vein, in which a short vein enters the inferior vena cava directly.
Some venous samples thus acquired may be diluted by blood from the inferior vena cava on the right and from the phrenic or renal vein on the left. To overcome the problem of dilution, cortisol levels can be measured from the same samples. A low cortisol level suggests dilution by nonadrenal blood, whereas a high cortisol level indicates a relatively pure sample. When aldosterone and cortisol are measured in blood samples from the same site, an aldosterone-cortisol ratio that corrects the concentration of aldosterone for dilution can be calculated.
An accuracy of 95% and a sensitivity of 75% have been reported with adrenal venous sampling. Adrenal venous sampling is required for the definitive diagnosis of primary aldosteronism and for the detection of laterality of the adrenal lesion. [25]
Zarnegar and colleagues conducted a study of 59 patients with hyperaldosteronism who underwent unilateral adrenalectomy [26] on the basis of CT scan alone (N=30) or CT scan and adrenal venous sampling (N=29), and the authors found that adrenalectomy had similar clinical effects in the 2 groups. CT scanning can be used to reliably diagnose adenomas larger than 1.0 cm. The authors recommended that adrenal venous sampling be reserved for cases in which CT scan findings are equivocal or in which both of the patient's adrenal glands are abnormal.
The dilution of blood from the inferior vena cava on the right and from the renal or phrenic vein on the left can lead to erroneous results in adrenal venous sampling.
Unilateral adrenal hyperplasia is not rare, sharing the same features of aldosterone-producing adenoma. When disease lateralization is confirmed by adrenal venous sampling, unilateral adrenalectomy achieves excellent long-term results. [27]
-
Longitudinal sonogram through the left kidney in a 32-year-old woman who presented with hypertension shows a 3-cm hypoechoic but solid mass superior to the upper pole of the kidney. Initially, the mass was regarded as a nonfunctioning adenoma unrelated to the patient's hypertension. Subsequently, mild hypokalemia developed. Surgical resection confirmed a tumor due to Conn syndrome.
-
Axial enhanced CT scan in a 32-year-old woman who presented with hypertension shows a low-attenuating 2.8-cm suprarenal mass (A) (same patient as in previous image). Histologic results obtained after surgery confirmed a tumor due to Conn syndrome.
-
Axial nonenhanced CT scan through the adrenal glands in 56-year-old man shows multiple nodules in both glands, although biochemical results indicated primary aldosteronism. The patient received medical treatment.
-
Axial enhanced CT scan in a 56-year-old man shows no enhancement of the adrenal masses (same patient as in the previous image).
-
Axial nonenhanced CT scan through the adrenal glands in a 60-year-old patient who presented with hypertension and hypokalemia shows a bilobulated tumor in the right adrenal gland.
-
Axial enhanced CT scan through the adrenal glands in a 60-year-old patient who presented with hypertension and hypokalemia shows minor tumor enhancement (same patient as in previous image). Note the normal left adrenal gland.
-
A 59-year-old man was referred for renal ultrasonography as a part of the workup for newly diagnosed hypertension. The sonogram depicted a 3-cm right adrenal mass, which was regarded as an incidentaloma (not shown). Axial enhanced CT scan through the adrenal gland shows minor patchy enhancement in a right adrenal tumor.
-
Scintigram obtained by using iodine-131-6-beta-iodomethylnorcholesterol (NP-59) in a 59-year-old man with hypertension shows fairly intense radionuclide uptake in the right adrenal tumor. At surgery, a Conn tumor was confirmed.