Practice Essentials
Esophageal varices are submucosal distal esophageal veins, connecting the portal circulation and systemic circulation, that are dilated because of portal hypertension, most commonly because of cirrhosis, resistance to portal blood flow, and increased portal venous blood inflow. Variceal rupture is the most common fatal complication of cirrhosis. [1]
They are native veins that serve as collaterals to the central venous circulation when flow through the portal venous system or superior vena cava (SVC) is obstructed. Esophageal varices are collateral veins within the wall of the esophagus that project directly into the lumen. They are of clinical concern because they are prone to hemorrhage.
Paraesophageal varices are collateral veins beyond the adventitial surface of the esophagus that parallel intramural esophageal veins. Paraesophageal varices are less prone to hemorrhage. Esophageal and paraesophageal varices are slightly different in venous origin, but they are usually found together. [2, 3]
There are 2 types of esophageal varices: downhill and uphill. Uphill varices are common and are found at the lower end of the esophagus; they extend upward and develop because of portal hypertension. Downhill varices are rare and are found at the upper esophagus; they extend downward and usually occur because of superior vena cava obstruction. [4]
(Esophageal and paraesophageal varices are displayed in the images below.)
 Uphill esophageal varices. Barium swallow demonstrates multiple serpiginous filling defects primarily involving the lower one third of the esophagus with striking prominence around the gastroesophageal junction. The patient had cirrhosis secondary to alcohol abuse.
Uphill esophageal varices. Barium swallow demonstrates multiple serpiginous filling defects primarily involving the lower one third of the esophagus with striking prominence around the gastroesophageal junction. The patient had cirrhosis secondary to alcohol abuse.
 Downhill esophageal varices on barium swallow examination. Notice the serpiginous filling defects proximally with normal-appearing esophagus distally.
Downhill esophageal varices on barium swallow examination. Notice the serpiginous filling defects proximally with normal-appearing esophagus distally.
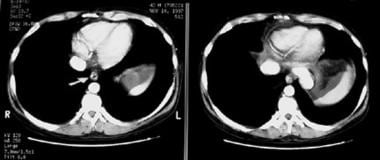
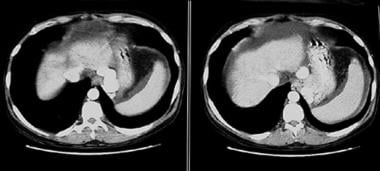 Computed tomography scan shows large, enhancing paraesophageal varices just to the left of the esophagus. Note the ascites and cirrhosis.
Computed tomography scan shows large, enhancing paraesophageal varices just to the left of the esophagus. Note the ascites and cirrhosis.
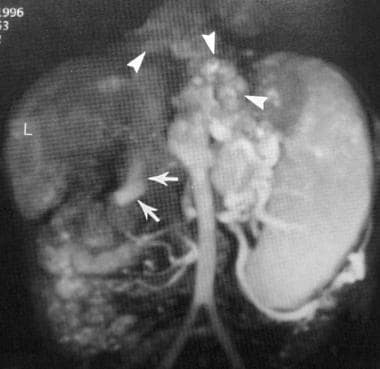 Maximum intensity projection magnetic resonance image of the portal venous system demonstrates extensive esophageal varices (arrows) in conjunction with splenic and gastric varices. L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
Maximum intensity projection magnetic resonance image of the portal venous system demonstrates extensive esophageal varices (arrows) in conjunction with splenic and gastric varices. L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
Imaging modalities
The gold-standard for evaluation of esophageal varices is esophagogastroduodenoscopy, but radiographic modalities, such as CT, MRI, and ultrasonography, have been studied as noninvasive means of diagnosing esophageal varices and evaluating the risk of bleeding. Esophageal and paraesophageal varices have been identified on contrast-enhanced cross-sectional imaging as torturous, enlarged, smooth tubular structures. [5, 6, 7, 8, 9, 10, 11, 12, 1]
(See the images below.)
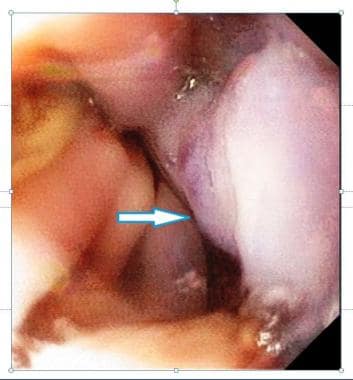 An endoscopic image of esophageal varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
An endoscopic image of esophageal varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
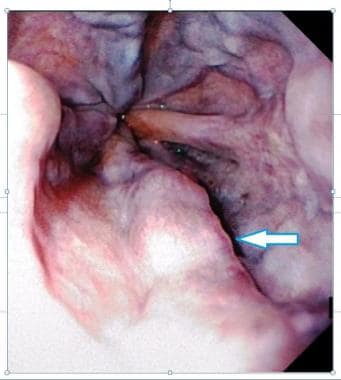 Endoscopic picture of esophageal varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
Endoscopic picture of esophageal varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
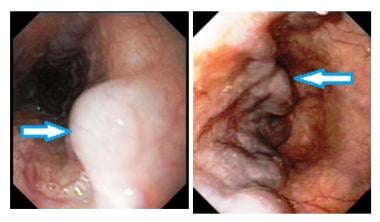 Endoscopic pictures of esophageal varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
Endoscopic pictures of esophageal varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
When esophageal varices are discovered, they are graded according to their size, as follows:
-
Grade 1 – Small, straight esophageal varices
-
Grade 2 – Enlarged, tortuous esophageal varices occupying less than one third of the lumen
-
Grade 3 – Large, coil-shaped esophageal varices occupying more than one third of the lumen
The esophageal varices are also inspected for red wheals, which are dilated intraepithelial veins under tension and which carry a significant risk for bleeding (see the image below). The grading of esophageal varices and identification of red wheals by endoscopy predict a patient's bleeding risk, on which treatment is based.
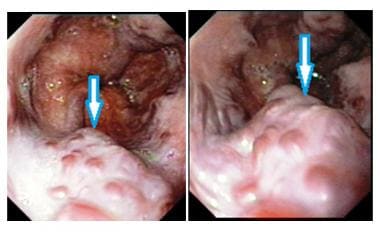 Esophageal varices with cherry red spots. These spots are suggestive of recent or impending bleeding from the varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
Esophageal varices with cherry red spots. These spots are suggestive of recent or impending bleeding from the varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
Varices can also be seen in the stomach and the duodenum (see the images below).
 Fundal varices found during endoscopic examination of the stomach. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
Fundal varices found during endoscopic examination of the stomach. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
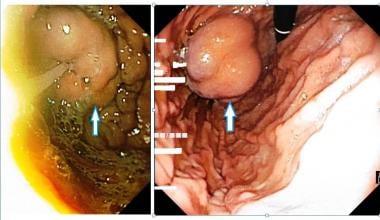 Fundal varices seen on endoscopic examination of the stomach. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
Fundal varices seen on endoscopic examination of the stomach. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
 Fundal varices. The photo on the right shows endoscopic findings in a 47-year-old man with a history of polycythemia rubra vera who had a recent episode of hematemesis. Endoscopy showed a normal esophagus, but multiple polypoid submucosal lesions were seen in the fundus and body of the stomach. The final diagnosis was left-sided portal hypertension secondary to splenic vein thrombosis.
Fundal varices. The photo on the right shows endoscopic findings in a 47-year-old man with a history of polycythemia rubra vera who had a recent episode of hematemesis. Endoscopy showed a normal esophagus, but multiple polypoid submucosal lesions were seen in the fundus and body of the stomach. The final diagnosis was left-sided portal hypertension secondary to splenic vein thrombosis.
 Duodenal varice noted on endoscopic exam. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
Duodenal varice noted on endoscopic exam. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
Endoscopy is also used for interventions. The following pictures demonstrate band ligation of esophageal varices.
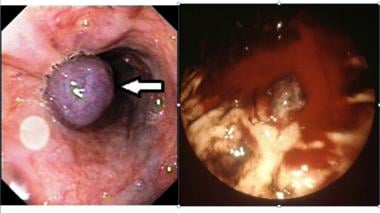 These two photos show band ligation of esophageal varices. The image on the right is of a 43-year-old patient with known alcoholic cirrhosis and portal hypertension presented with a massive hematemesis. The bleeding esophageal varices were banded during the endoscopic procedure.
These two photos show band ligation of esophageal varices. The image on the right is of a 43-year-old patient with known alcoholic cirrhosis and portal hypertension presented with a massive hematemesis. The bleeding esophageal varices were banded during the endoscopic procedure.
CT scanning and MRI are identical in their usefulness in diagnosing and evaluating the extent of esophageal varices. These modalities have an advantage over endoscopy because CT scanning and MRI can help in evaluating the surrounding anatomic structures, both above and below the diaphragm. CT scanning and MRI are also valuable in evaluating the liver and the entire portal circulation. [13]
These modalities are used in preparation for a transjugular intrahepatic portosystemic shunt (TIPS) procedure or liver transplantation and in evaluating for a specific etiology of esophageal varices. These modalities also have an advantage over both endoscopy and angiography because they are noninvasive. CT scanning and MRI do not have strict criteria for evaluating the bleeding risk, and they are not as sensitive or specific as endoscopy. CT scanning and MRI may be used as alternative methods in making the diagnosis if endoscopy is contraindicated (eg, in patients with a recent myocardial infarction or any contraindication to sedation).
In the past, angiography was considered the criterion standard for evaluation of the portal venous system. However, current CT scanning and MRI procedures have become equally sensitive and specific in the detection of esophageal varices and other abnormalities of the portal venous system. Although the surrounding anatomy cannot be evaluated the way they can be with CT scanning or MRI, angiography is advantageous because its use may be therapeutic as well as diagnostic. In addition, angiography may be performed if CT scanning or MRI findings are inconclusive. [14]
Ultrasonography, excluding endoscopic ultrasound (EUS), and nuclear medicine studies are of minor significance in the evaluation of esophageal varices. EUS is used primarily in the evaluation and staging of esophageal and pancreatic carcinomas, but it has also played a role in the evaluation and treatment of esophageal varices. [15, 16, 17, 18, 19]
Nuclear medicine does not play a clinically useful role in the evaluation or diagnosis of esophageal varices. In occasional case reports in the literature, variceal hemorrhage was identified as a source of upper gastrointestinal tract bleeding seen on a tagged-RBC scan.
A group from Japan used abdominal blood pool, single-photon emission CT (SPECT) scanning as a tool to evaluate success and predict recurrence of esophageal varices after sclerotherapy. [20] More literature has been generated regarding the use of EUS imaging, with good results. [15, 16, 21]
The American Association for the Study of Liver Diseases (AASLD) and the Baveno VI consensus statement have recommended the use of noninvasive tests to stratify patients and rule out high-risk esophageal varices. According to the Baveno VI consensus statement, patients with liver stiffness greater than 20 kPa and a platelet count greater than 150,000 uL have a very low risk of clinically significant varices. [22, 23, 24, 25, 26]
Limitations of techniques
Although endoscopy is the criterion standard in diagnosing and grading esophageal varices, the anatomy outside of the esophageal mucosa cannot be evaluated with this technique. Therefore, imaging modalities such as CT scanning, MRI, and EUS are also performed for a more complete evaluation.
Barium swallow examination is not a sensitive test, and it must be performed carefully with close attention to the amount of barium used and the degree of esophageal distention. Barium swallow images may help in detecting only 50% of esophageal varices.
On CT scans and MRIs, esophageal varices are difficult to see at times. However, in severe disease, esophageal varices may be prominent. CT scanning and MRI are useful in evaluating other associated abnormalities and adjacent anatomic structures in the abdomen or thorax. On MRIs, surgical clips may create artifacts that obscure portions of the portal venous system. Disadvantages of CT scanning include the possibility of adverse reactions to the contrast agent and an inability to quantitate portal venous flow, which is an advantage of MRI and ultrasonography.
Radiography
Plain radiography
Plain radiographic findings are insensitive and nonspecific in the evaluation of esophageal varices.
Plain radiographic findings may suggest paraesophageal varices. Anatomically, paraesophageal varices are outside the esophageal wall and may create abnormal opacities. Esophageal varices are within the wall; therefore, they are concealed in the normal shadow of the esophagus.
Ishikawa et al described chest radiographic findings in paraesophageal varices in 352 patients with portal hypertension, [27] and the most common was obliteration of a short or long segment of the descending aorta without a definitive mass shadow. Other plain radiographic findings included a posterior mediastinal mass and an apparent intraparenchymal mass. On other images, the intraparenchymal masses were confirmed to be varices in the region of the pulmonary ligament.
On plain radiographs, a downhill varix may be depicted as a dilated azygos vein that is out of proportion to the pulmonary vasculature. In addition, a widened superior mediastinum may be shown. A widened superior mediastinum may result from dilated collateral veins or the obstructing mass.
Barium study
Endoscopy is the criterion standard for diagnosing esophageal varices. Barium studies may be of benefit if the patient has a contraindication to endoscopy or if endoscopy is not available (see the images below). Pay attention to technique to optimize detection of esophageal varices. The procedure should be performed with the patient in the supine or slight Trendelenburg position.
 Uphill esophageal varices. Barium swallow demonstrates multiple serpiginous filling defects primarily involving the lower one third of the esophagus with striking prominence around the gastroesophageal junction. The patient had cirrhosis secondary to alcohol abuse.
Uphill esophageal varices. Barium swallow demonstrates multiple serpiginous filling defects primarily involving the lower one third of the esophagus with striking prominence around the gastroesophageal junction. The patient had cirrhosis secondary to alcohol abuse.
These positions enhance gravity-dependent flow and engorge the vessels. The patient should be situated in an oblique projection and, therefore, in a right anterior oblique position to the image intensifier and a left posterior oblique position to the table. This positioning prevents overlap with the spine and further enhances venous flow.
A thick barium suspension or paste should be used to increase adherence to the mucosal surface. Ideally, single swallows of a small amount of barium should be ingested to minimize peristalsis and to prevent overdistention of the esophagus. If the ingested bolus is too large, the esophagus may be overdistended with dense barium, and the mucosal surface may be smoothed out, rendering esophageal varices invisible.
In addition, a full column of dense barium may white out any findings of esophageal varices. Too many contiguous swallows create a powerful, repetitive, stripping wave of esophageal peristalsis that squeezes blood out of the varices as it progresses caudally.
Effervescent crystals may be used to provide air contrast, but crystals may also cause overdistention of the esophagus with gas and thereby hinder detection of esophageal varices. In addition, crystals may create confusing artifacts in the form of gas bubbles, which may mimic small varices.
The Valsalva maneuver may be useful to further enhance radiographic detection of esophageal varices. The patient is asked to "bear down as if you are having a bowel movement" or asked to "tighten your stomach muscles as if you were doing a sit-up." The Valsalva maneuver increases venous return and also prevents further peristaltic waves. The Valsalva maneuver also traps barium in the distal esophagus and allows retrograde flow for an even coating.
Barium study findings are as follows:
-
Esophageal varices appear as tortuous, serpiginous, longitudinal filling defects that project into the lumen of the esophagus; these defects are seen best on relief projections of the esophagus
-
Esophageal varices may appear as thickened folds with rounded expansions etched in white because of barium trapped in the grooves of adjacent varices; this appearance may differentiate esophageal varices from the thickened esophageal folds of esophagitis
-
In a filled esophagus, varices may be identified as a scalloped border, which is a more specific sign of esophageal varices, especially if found in conjunction with the aforementioned findings
-
In the differential diagnosis, varicoid carcinoma of the esophagus is important; varicoid carcinoma demonstrates a similar appearance to esophageal varices, but it has a more-rigid appearance that does not change or become distended with positioning, repetitive swallows, or use of the Valsalva maneuver.
Degree of confidence
Plain radiographic findings suggestive of paraesophageal varices are very nonspecific. Any plain radiographic findings suggesting paraesophageal varices should be followed up with CT scanning or a barium study to differentiate the findings from a hiatal hernia, posterior mediastinal mass, or other abnormality (eg, rounded atelectasis). Similarly, barium studies or CT scan findings suggestive of esophageal varices should be followed up with endoscopy. Endoscopic follow-up imaging can be used to evaluate the grade and appearance of esophageal varices to assess the bleeding risk. The results of this assessment direct treatment.
In review case studies, a single thrombosed esophageal varix may be confused with an esophageal mass on barium studies. With endoscopy, the 2 entities can be differentiated easily.
The only normal variant is a hiatal hernia. The rugal fold pattern of a hiatal hernia may be confused with esophageal varices; however, a hiatal hernia can be identified easily by the presence of the B line marking the gastroesophageal junction.
Computed Tomography
CT scanning is an excellent method for detecting moderate to large esophageal varices and for evaluating the entire portal venous system. CT scanning is a minimally invasive imaging modality that involves the use of only a peripheral intravenous line; therefore, it is a more attractive method than angiography or endoscopy in the evaluation of the portal venous system (see the images below). [10, 11, 28, 29]
 Computed tomographic appearance of esophageal varices. Arrow points to enhancing vascular structures within the wall of the esophagus projecting into the lumen.
Computed tomographic appearance of esophageal varices. Arrow points to enhancing vascular structures within the wall of the esophagus projecting into the lumen.
 Computed tomography scan shows large, enhancing paraesophageal varices just to the left of the esophagus. Note the ascites and cirrhosis.
Computed tomography scan shows large, enhancing paraesophageal varices just to the left of the esophagus. Note the ascites and cirrhosis.
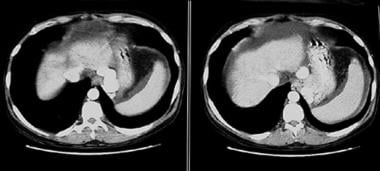
 Computed tomography sections demonstrate esophageal varices protruding into the lumen, as well as paraesophageal varices.
Computed tomography sections demonstrate esophageal varices protruding into the lumen, as well as paraesophageal varices.
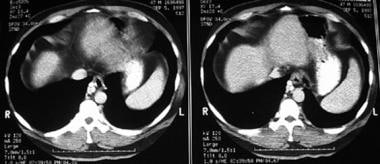
 Computed tomography scan showing esophageal varices. Note the extensive collateralization within the abdomen adjacent to the spleen as a result of severe portal hypertension.
Computed tomography scan showing esophageal varices. Note the extensive collateralization within the abdomen adjacent to the spleen as a result of severe portal hypertension.
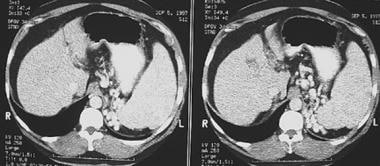
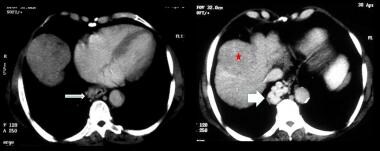 Axial contrast-enhanced CT scans in the portal venous phase show irregular liver surface due to cirrhosis and esophageal and para-esophageal varices (white arrows). Note the hypodense mass in the liver, proven hepatocellular carcinoma (red star).
Axial contrast-enhanced CT scans in the portal venous phase show irregular liver surface due to cirrhosis and esophageal and para-esophageal varices (white arrows). Note the hypodense mass in the liver, proven hepatocellular carcinoma (red star).
Helical CT scanning and portal venography
Helical CT scanning and CT portal venography are becoming more important preprocedural tools before performing TIPS and transplantation. A variety of techniques have been described for the CT evaluation of the portal venous system. Most involve a helical technique with a pitch of 1.5-1.7–mm and 5-mm collimation. For imaging, 100-150 mL of 60% iodinated contrast is administered into an 18-gauge (preferred) peripheral intravenous line with a 60- to 80-second delay. The images are reconstructed in 5-mm increments. The amount of contrast material and the delay time are slightly greater than those in conventional helical CT scanning of the abdomen. The difference in technique ensures adequate opacification of both the portal venous and mesenteric arterial systems.
Contrast-enhanced studies
On nonenhanced studies, esophageal varices may not be depicted well. Only a thickened esophageal wall may be found. Paraesophageal varices may appear as enlarged lymph nodes, posterior mediastinal masses, or a collapsed hiatal hernia. On contrast-enhanced images, esophageal varices appear as homogeneously enhancing tubular or serpentine structures projecting into the lumen of the esophagus. Paraesophageal varices are easier to detect than esophageal varices because of the contrast of the surrounding lung and mediastinal fat.
On contrast-enhanced CT scans, downhill esophageal varices may have an appearance similar to that of uphill varices, varying only in location. Because the etiology of downhill esophageal varices is usually secondary to superior vena cava (SVC) obstruction, the physician must be aware of other potential collateral pathways that may suggest the diagnosis.
Stanford et al published data based on venography, [30] describing 4 patterns of flow in the setting of SVC obstruction as follows [30] :
-
Type 1 – Partial occlusion of the SVC with patency of the azygos vein
-
Type 2 – Near-complete or complete obstruction of the SVC, with patency and antegrade flow through the azygos vein and into the right atrium
-
Type 3 – Near-complete or complete obstruction of the SVC with reversal of azygos blood flow
-
Type 4 – Complete obstruction of the SVC and 1 or more major caval tributaries, including the azygos system
In a retrospective investigation, Cihangiroglu et al analyzed CT scans from 21 studies of patients with SVC obstruction [31] and described as many as 15 different collateral pathways. Only 8 patients could be characterized by using the Stanford classification.
In the setting of SVC obstruction, the most common collateral pathways were the (in decreasing order of frequency): (1) azygos vein, (2) thoracoepigastric vein, (3) mediastinal vein, and (4) internal mammary vein. [31] The azygos vein collateral is most likely to develop downhill esophageal varices; however, any collateral vessel identified in the chest wall or mediastinum in the setting of SVC obstruction should prompt the radiologist to look for esophageal varices.
In a study by Zhao et al of 64-row multidetector CT portal venography for characterizing paraesophageal varices in 52 patients with portal hypertensive cirrhosis and esophageal varices, [32] 50 of the 52 cases showed an origin from the posterior branch of left gastric vein, whereas the others were from the anterior branch. Fifty cases demonstrated their locations close to the esophagogastric junction; the other 2 cases were extended to the inferior bifurcation of the trachea. [32]
Forty-three patients in the Zhao et al study showed the communications between paraesophageal varices and periesophageal varices, whereas the hemiazygos vein (43 cases) and IVC (5 cases) were also involved. [32] Zhao et al concluded that "64-row multidetector computed tomography portal venography could display the location, morphology, origin, and collateral types of paraesophageal varices, which provides important and referable information for clinical management and disease prognosis." [32]
Degree of confidence
CT scanning is a minimally invasive method used to detect moderate to large esophageal varices and to evaluate the entire portal venous system. CT scans also help in evaluating the liver, other venous collaterals, details of other surrounding anatomic structures, and the patency of the portal vein. In these situations, CT scanning has a major advantage over endoscopy; however, unlike endoscopy, CT scans are not useful in predicting variceal hemorrhage.
Compared with angiography, CT scanning is superior in detecting paraumbilical and retroperitoneal varices and at providing a more thorough examination of the portal venous system without the risk of intervention. In the detection of esophageal varices, CT scanning is slightly better than angiography. As many as 25% of esophageal varices detected at endoscopy may be missed on angiograms. CT scanning and angiography are approximately equal in the detection of varices smaller than 3 mm. If CT scans do not demonstrate small varices, they are unlikely to be seen on angiograms.
Contrast-enhanced CT scanning is essential for evaluating esophageal varices. Contrast enhancement greatly increases the sensitivity and specificity of the examination and reduces the rate of false-positive or false-negative results. On nonenhanced CT scans, esophageal varices may mimic soft-tissue masses, enlarged lymph nodes, or other gastrointestinal tract abnormalities (eg, hiatal hernia).
Magnetic Resonance Imaging
MRI is an excellent noninvasive method for imaging the portal venous system and esophageal varices (see the images below). Esophageal varices appear as flow voids on conventional T1- and T2-weighted images. This appearance makes them easily distinguishable from soft tissue masses. Flow voids appear as well-defined circular structures outside of or within the wall of the esophagus on axial images or serpiginous on sagittal or coronal images. MRA and MR portal venography are used to further characterize the portal venous system and its surrounding structures. [33]
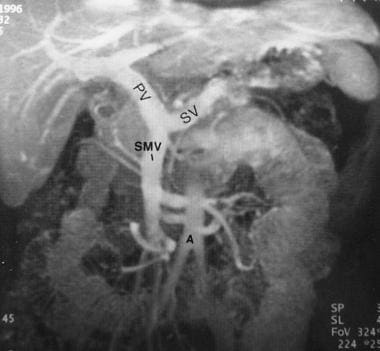 Maximum intensity projection magnetic resonance image of the normal portal venous system. PV = portal vein; SMV = superior mesenteric vein; SV = splenic vein. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
Maximum intensity projection magnetic resonance image of the normal portal venous system. PV = portal vein; SMV = superior mesenteric vein; SV = splenic vein. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
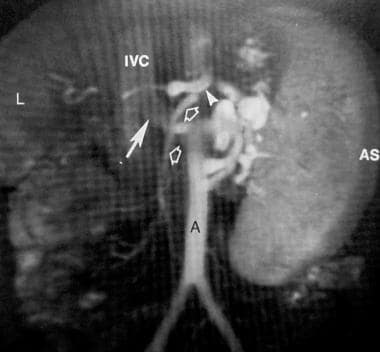 Maximum intensity projection magnetic resonance image of the portal venous system. A = abdominal aorta; AS = spleen; IVC = inferior vena cava; L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
Maximum intensity projection magnetic resonance image of the portal venous system. A = abdominal aorta; AS = spleen; IVC = inferior vena cava; L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
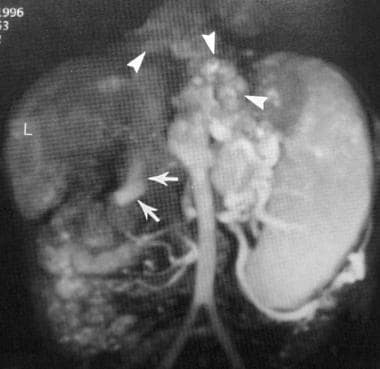 Maximum intensity projection magnetic resonance image of the portal venous system demonstrates extensive esophageal varices (arrows) in conjunction with splenic and gastric varices. L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
Maximum intensity projection magnetic resonance image of the portal venous system demonstrates extensive esophageal varices (arrows) in conjunction with splenic and gastric varices. L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
Most imaging protocols are based on time-of-flight or phase-contrast methods. Improved images can be obtained by using a contrast-enhanced, breath-hold, fat-saturated, segmented, 3-dimensional (3-D), gradient-echo technique. This approach involves imaging during 3 sequential breath holds, 6 seconds apart, after the injection of paramagnetic contrast material. Data from the 3 acquisitions are processed by using a maximum intensity projection (MIP) algorithm. The MIP technique provides imaging of the entire vascular anatomy at different phases, and it provides excellent resolution in a short time (see the images below).
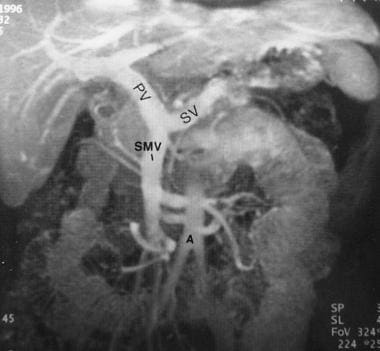 Maximum intensity projection magnetic resonance image of the normal portal venous system. PV = portal vein; SMV = superior mesenteric vein; SV = splenic vein. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
Maximum intensity projection magnetic resonance image of the normal portal venous system. PV = portal vein; SMV = superior mesenteric vein; SV = splenic vein. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
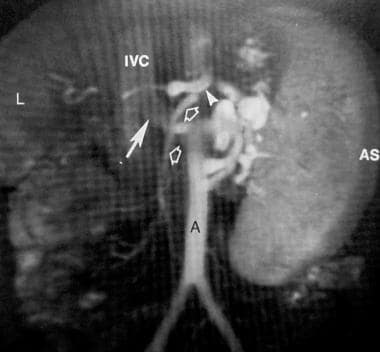 Maximum intensity projection magnetic resonance image of the portal venous system. A = abdominal aorta; AS = spleen; IVC = inferior vena cava; L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
Maximum intensity projection magnetic resonance image of the portal venous system. A = abdominal aorta; AS = spleen; IVC = inferior vena cava; L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
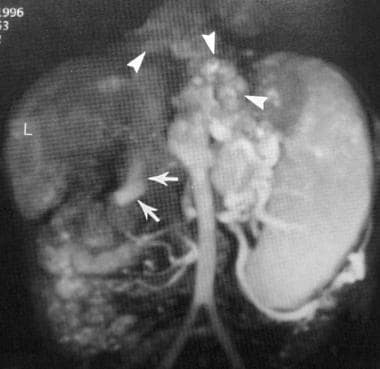 Maximum intensity projection magnetic resonance image of the portal venous system demonstrates extensive esophageal varices (arrows) in conjunction with splenic and gastric varices. L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
Maximum intensity projection magnetic resonance image of the portal venous system demonstrates extensive esophageal varices (arrows) in conjunction with splenic and gastric varices. L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
Esophageal varices and other portosystemic collateral vessels are demonstrated as serpiginous contrast-enhanced vessels in the portal venous phase. Downhill esophageal varices appear similar to uphill varices. The advantage of MRI over CT scanning in evaluating downhill esophageal varices is its superior ability in evaluating soft tissues. Therefore, if SVC obstruction caused by a tumor is identified, the adjacent soft-tissue structures of the mediastinum, thoracic inlet, and brachial plexus can be evaluated.
Degree of confidence
Similar to CT, MRI is becoming a more common examination in pre-TIPS (transjugular intrahepatic portosystemic shunt) and pretransplantation evaluations. The only major disadvantages of MRI compared with CT are its limited availability and cost; otherwise, CT and MRI are equal in imaging the portal venous system and in detecting esophageal varices. An advantage of MRI over CT includes the ability to quantitate the peak velocity and to determine the direction of venous blood flow. As a result, MRI rivals ultrasonography when a bolus-tracking technique is used. Other advantages include better characterization of liver tumors and avoidance of iodinated contrast material.
In patients with severe portal hypertension, stagnant or to-and-fro flow may produce low or no signal intensity in a patent vessel, which may be mistaken for nonobstructive thrombus or occluded vessel. Surgical clips may create artifacts that obscure portions of the portal venous system. In imaging patients with portal hypertension, ascites may create significant motion artifact that degrades image quality and may result in a nondiagnostic study. Paracentesis is recommended prior to examination in patients with a large amount of ascites.
Ultrasonography
Duplex Doppler ultrasonography is excellent for evaluating the velocity and direction of flow in the portal venous system, and this imaging modality is also good for evaluating portal vein patency.
Ultraonography also provides an adequate evaluation of the size and echotexture of the liver. In the evaluation and detection of esophageal varices, conventional ultrasonography is limited and not clinically useful. [34]
Endoscopic ultrasonography (EUS) is a procedure performed by gastroenterologists, sometimes in conjunction with radiologists, to evaluate the esophagus. The procedure is used primarily in the evaluation and staging of esophageal and pancreatic carcinomas, but it has also played a role in the evaluation and treatment of esophageal varices. [15, 16, 17, 18, 19]
(See the images below.)
 An oblique color Doppler ultrasound scan through gallbladder fossa shows varices around the gallbladder in a patient with portal hypertension/portal vein thrombosis.
An oblique color Doppler ultrasound scan through gallbladder fossa shows varices around the gallbladder in a patient with portal hypertension/portal vein thrombosis.
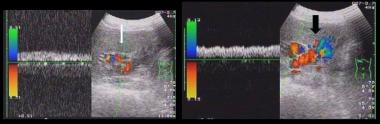 Spectral Doppler and Color Doppler ultrasound show perihilar (white arrow) and peripancreatic varices (black arrow). The patient had portal hypertension and portal vein thrombosis.
Spectral Doppler and Color Doppler ultrasound show perihilar (white arrow) and peripancreatic varices (black arrow). The patient had portal hypertension and portal vein thrombosis.
While the patient is under light sedation, a 13-mm side-view endoscope with a small ultrasound probe (7.5 or 12 MHz) at its tip is introduced into the esophagus. Once the desired placement is confirmed endoscopically, a water-filled balloon is inflated around the probe in close contact with the mucosal surface of the esophagus. Occasionally, sodium chloride solution is also introduced into the lumen to eliminate any air artifact. Axial images in a 180° or 360° field of view are generated. The images demonstrate all 5 layers of the esophagus, in alternating echogenic and hypoechoic layers, starting with the echogenic mucosa.
Varices are identified as multiple, well-circumscribed, hypoechoic or anechoic structures that have a tubular or serpiginous appearance; they are located in the submucosal layer. Some EUS probes have color Doppler capability and permit the demonstration of flow. EUS has been used to guide sclerotherapy for precise injection of the sclerosing agent. EUS has also played a role in postsclerotherapy follow-up to predict the recurrence of esophageal varices. The prediction is made by identifying and measuring the size of the surrounding paraesophageal and perforating veins.
Degree of confidence
In a study by Burtin et al of 58 patients with cirrhosis and 16 control subjects, [21] esophageal varices were detected more often with endoscopy (88%) than with EUS (55%). In addition, Burtin et al reported that higher-grade esophageal varices, as determined endoscopically, were more readily detected with EUS. Esophpageal varices are graded 0-3 on the basis of their protrusion into the esophageal lumen. A significant increase in the rate of EUS detection was found between grade 1 esophageal varices (25%) and grade 2 varices (73%). [21] This increase is believed to be because grade 0 and 1 esophageal varices are easily compressed out by the inflated balloon and are not as readily detectable.
Even with a water-filled esophagus, the overall detection rate for esophageal varices with EUS is only 60%. Endoscopic detection of esophageal varices alone remains the criterion standard, with EUS adding little more information to the evaluation.
With color Doppler ultrasonography, esophageal varices can be identified easily. However, in patients with a thrombosed varix due to either idiopathic causes or sclerotherapy, the appearance may resemble those of other submucosal masses, such as cystic duplications, leiomyomas, or leiomyosarcomas. These masses are more likely to be solitary or rounded, and they are not tubular or serpiginous, as are varices. Case reports describe a solitary thrombosed idiopathic varix, but these are extremely rare. A clinical history of cirrhosis or other causes of portal hypertension is helpful in evaluating such masses. [12, 35]
Angiography
Before the advent of flexible endoscopy, angiography was the criterion standard in diagnosing esophageal varices. [36, 37] Angiographic findings of esophageal varices appear similar to those of serpiginous varicose veins in contiguity with the left gastric or azygos veins, depending on whether the course is uphill or downhill. [38]
Multiple small collateral vessels may be depicted in the upper chest, head, and extremities in the setting of downhill esophageal varices. Parasplenic, gastric, and umbilical varices may be seen in association with uphill esophageal varices.
Three major angiographic approaches to the imaging and evaluation of the portal venous system and esophageal varices are used: indirect arterial portography, percutaneous transhepatic portography (TIP), and hepatic phlebography. [38]
Indirect arterial portography
Indirect arterial portography involves obtaining arterial access through the arm or groin and selectively cannulating the celiac or superior mesenteric arteries. A bolus of contrast agent is injected to obtain mesenteric angiograms and delayed images of the portal venous and splanchnic venous systems.
Intra-arterial injections of vasodilators, such as prostaglandin E or papaverine, may increase the amount of contrast agent that reaches the venous system to improve vessel opacification. The technique is useful for defining the anatomy before the performance of shunt procedures and for evaluating the collateral circulation, including esophageal varices. Major complications include bleeding at the arterial puncture site and dissection or pseudoaneurysm of any artery along the path of the procedure.
Percutaneous transhepatic portography (TIP)
TIP involves direct puncture of a main portal venous branch under ultrasonographic guidance, fluoroscopic guidance, or both. The patient receives local anesthesia at the midaxillary line and the 10th intercostal space. A 22-gauge Chiba needle is inserted parallel to the table and slightly inferiorly. The needle is withdrawn while contrast material is injected until a portal branch is opacified.
Once the vessel is identified, a 5-French (5F) catheter is inserted by using the Seldinger technique. Venography may be performed through the catheter. This procedure may also help in evaluating the venous anatomy and in identifying collaterals. TIP has the added benefit of better opacification of the main and intrahepatic portal venous system in the setting of hepatofugal flow.
Intervention, such as variceal embolization, may be performed by using this approach. Although the risk is low with the procedure, morbidity rates are increased compared with those of indirect portography. Potential additional complications include subcapsular hematoma, hemobilia, biloma formation, and perforation of a hollow viscus.
Hepatic phlebography
Hepatic phlebography involves venipuncture of the common femoral or common jugular vein and advancement of a catheter to the level of the hepatic veins through the inferior or superior vena cava, respectively. The primary purpose of the procedure is not to thoroughly evaluate the portal circulation but to evaluate hepatic venous anatomy and to search for postsinusoidal etiologies of portal hypertension.
Iodinated contrast material or carbon dioxide may be injected through a catheter wedged in a hepatic vein to obtain digital subtraction (DSA) images of the hepatic venous system and, possibly, the portal venous system (in hepatofugal flow).
The liver parenchyma may be roughly evaluated for indirect signs of cirrhosis (pruned-tree venographic appearance), malignancy, and intrahepatic venous-to-venous anastomoses. Indirect measurement of the portal venous pressure may be obtained by measuring the difference between the free hepatic venous pressure and hepatic venous wedge pressures.
Interventions, such as transvenous liver biopsy and the TIP shunt (TIPS) procedure, may be performed by using this approach. Complications of the procedure are minimal, with a small possibility of infection and bleeding at the venipuncture site.
Degree of confidence
Angiographic images may cause as many as 25% of esophageal varices to be missed, and the technique is inferior to endoscopy. Detection is slightly better with a percutaneous technique, but it potentially creates more morbidity than the indirect method. Hepatic phlebography is not a technique designed for the detection of esophageal varices.
The major disadvantage of angiography is incomplete opacification of the portal venous system, either because of extreme hepatofugal flow, to-and-fro flow, or the dilution of the contrast medium. Incomplete opacification may create problems in evaluation for portal vein thrombosis or in detecting collateral pathways, including esophageal varices. Incomplete opacification is more of a problem with the indirect portography technique.
(See the images below.)
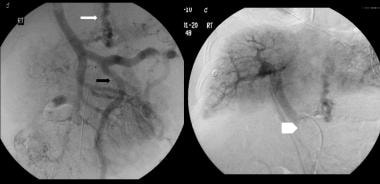 Digital subtraction venous phase of a superior mesenteric artery angiogram shows retrograde flow into the coronary vein (white arrow) and the inferior mesenteric vein (black arrow). Note the flow defect of the distal portal vein caused by retrograde flow (open arrowhead). The final diagnosis was hepatitis C cirrhosis, hepatocellular carcinoma of the left hepatic lobe (which had ruptured into the peritoneum), and portoarterial fistula (which had developed inside the ruptured tumor, giving rise to severe portal hypertension).
Digital subtraction venous phase of a superior mesenteric artery angiogram shows retrograde flow into the coronary vein (white arrow) and the inferior mesenteric vein (black arrow). Note the flow defect of the distal portal vein caused by retrograde flow (open arrowhead). The final diagnosis was hepatitis C cirrhosis, hepatocellular carcinoma of the left hepatic lobe (which had ruptured into the peritoneum), and portoarterial fistula (which had developed inside the ruptured tumor, giving rise to severe portal hypertension).
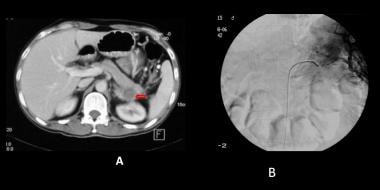 Sinistral portal hypertension is caused by occlusion of the splenic vein. The resultant elevated splenic venous pressure causes gastric varices that commonly present with hematemesis. Figure A shows a thrombus in the splenic vein, occluding the splenic vein (red arrow). Figure B is a subtraction digital splenic arteriogram in the venous phase showing splenic hilum venous collaterals but no filling of the splenic vein.
Sinistral portal hypertension is caused by occlusion of the splenic vein. The resultant elevated splenic venous pressure causes gastric varices that commonly present with hematemesis. Figure A shows a thrombus in the splenic vein, occluding the splenic vein (red arrow). Figure B is a subtraction digital splenic arteriogram in the venous phase showing splenic hilum venous collaterals but no filling of the splenic vein.
-
Normal venous flow through the portal and systemic circulation. IMC = inferior mesenteric vein; IVC = inferior vena cava; SVC = superior vena cava.
-
Redirection of flow through the left gastric vein secondary to portal hypertension or portal venous occlusion. Uphill varices develop in the distal one third of the esophagus. IMC = inferior mesenteric vein; IVC = inferior vena cava; SVC = superior vena cava.
-
Direction of venous flow with superior vena cava (SVC) obstruction proximal to the azygous vein. Flow is redirected through the azygous vein into the systemic circulation. Downhill varices develop in the upper one third of the esophagus. IMC = inferior mesenteric vein; IVC = inferior vena cava.
-
Direction of flow with superior vena cava (SVC) obstruction involving or distal to the azygous vein. Flow is redirected through the azygous vein, the esophageal veins, and into the portal circulation. Flow enters the systemic circulation through the inferior vena cava (IVC). Downhill varices develop the entire length of the esophagus. IMC = inferior mesenteric vein.
-
Uphill esophageal varices. Barium swallow demonstrates multiple serpiginous filling defects primarily involving the lower one third of the esophagus with striking prominence around the gastroesophageal junction. The patient had cirrhosis secondary to alcohol abuse.
-
Uphill esophageal varices on mucosal relief barium swallow.
-
Uphill esophageal varices on barium swallow.
-
Downhill esophageal varices. Mucosal relief view shows the serpiginous varicoid filling defects in the proximal esophagus, with normal distal mucosa in this patient with superior vena cava obstruction.
-
Downhill esophageal varices on barium swallow examination. Notice the serpiginous filling defects proximally with normal-appearing esophagus distally.
-
Barium swallow demonstrating esophageal varices involving the entire length of the esophagus. This appearance may be seen in advanced uphill varices or downhill varices secondary to superior vena cava obstruction at or below the level of the azygous vein.
-
Varices involving the entire esophagus on barium swallow examination. Note the thickened folds with rounded expansions at the level of the gastroesophageal junction that are characteristic of esophageal varices findings on barium studies.
-
Full-column image of the esophagus with varices throughout its entire length. Note scalloping of the borders of the filled esophagus. This sign, in conjunction with thickened folds with rounded expansions and some degree of distensibility, is pathognomonic for esophageal varices.
-
Computed tomographic appearance of esophageal varices. Arrow points to enhancing vascular structures within the wall of the esophagus projecting into the lumen.
-
Computed tomography scan shows large, enhancing paraesophageal varices just to the left of the esophagus. Note the ascites and cirrhosis.
-
Computed tomography sections demonstrate esophageal varices protruding into the lumen, as well as paraesophageal varices.
-
Computed tomography scan showing esophageal varices. Note the extensive collateralization within the abdomen adjacent to the spleen as a result of severe portal hypertension.
-
Maximum intensity projection magnetic resonance image of the normal portal venous system. PV = portal vein; SMV = superior mesenteric vein; SV = splenic vein. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
-
Maximum intensity projection magnetic resonance image of the portal venous system. A = abdominal aorta; AS = spleen; IVC = inferior vena cava; L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
-
Maximum intensity projection magnetic resonance image of the portal venous system demonstrates extensive esophageal varices (arrows) in conjunction with splenic and gastric varices. L = liver. Courtesy of Ali Shirkhoda, MD, William Beaumont Hospital, Royal Oak, Mich.
-
An endoscopic image of esophageal varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
-
Endoscopic picture of esophageal varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
-
Endoscopic pictures of esophageal varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
-
Esophageal varices with cherry red spots. These spots are suggestive of recent or impending bleeding from the varices. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
-
These two photos show band ligation of esophageal varices. The image on the right is of a 43-year-old patient with known alcoholic cirrhosis and portal hypertension presented with a massive hematemesis. The bleeding esophageal varices were banded during the endoscopic procedure.
-
Fundal varices found during endoscopic examination of the stomach. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
-
Fundal varices seen on endoscopic examination of the stomach. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
-
Fundal varices. The photo on the right shows endoscopic findings in a 47-year-old man with a history of polycythemia rubra vera who had a recent episode of hematemesis. Endoscopy showed a normal esophagus, but multiple polypoid submucosal lesions were seen in the fundus and body of the stomach. The final diagnosis was left-sided portal hypertension secondary to splenic vein thrombosis.
-
Duodenal varice noted on endoscopic exam. Courtesy of Dr M Inayatullah, Professor of Medicine, Nishtar Hospital, Multan, Pakistan.
-
An oblique color Doppler ultrasound scan through gallbladder fossa shows varices around the gallbladder in a patient with portal hypertension/portal vein thrombosis.
-
Spectral Doppler and Color Doppler ultrasound show perihilar (white arrow) and peripancreatic varices (black arrow). The patient had portal hypertension and portal vein thrombosis.
-
Axial contrast-enhanced CT scans in the portal venous phase show irregular liver surface due to cirrhosis and esophageal and para-esophageal varices (white arrows). Note the hypodense mass in the liver, proven hepatocellular carcinoma (red star).
-
Digital subtraction venous phase of a superior mesenteric artery angiogram shows retrograde flow into the coronary vein (white arrow) and the inferior mesenteric vein (black arrow). Note the flow defect of the distal portal vein caused by retrograde flow (open arrowhead). The final diagnosis was hepatitis C cirrhosis, hepatocellular carcinoma of the left hepatic lobe (which had ruptured into the peritoneum), and portoarterial fistula (which had developed inside the ruptured tumor, giving rise to severe portal hypertension).
-
Sinistral portal hypertension is caused by occlusion of the splenic vein. The resultant elevated splenic venous pressure causes gastric varices that commonly present with hematemesis. Figure A shows a thrombus in the splenic vein, occluding the splenic vein (red arrow). Figure B is a subtraction digital splenic arteriogram in the venous phase showing splenic hilum venous collaterals but no filling of the splenic vein.
-
Sinistral portal hypertension. Digital subtraction celiac axis angiography shows the splenic and the superior mesenteric veins, but not the occluded splenic vein.












