Practice Essentials
Acute epididymitis is the most common condition that causes acute scrotal pain in adults, although acute epididymitis, testicular torsion, and testicular tumors can have a common presentation of pain. Acute epididymitis is inflammation of the epididymis characterized by scrotal pain and swelling of less than 6 weeks' duration. The condition is referred to as acute epididymo-orchitis if concurrent inflammation of the testis is present. Distinguishing between acute epididymitis and testicular torsion is important because their treatments differ significantly and because testicular torsion is a true urologic emergency. [1, 2, 3, 4, 5, 6, 7]
Testicular torsion is rare in patients older than 35 years. Acute epididymitis is commonly the cause of acute scrotal pain in patients younger than age 18, very common in patients age 19 to 25, and overwhelmingly the etiology in patients older than age 25. Acute scrotal pain in prepubertal boys occurs most commonly from torsion of the testicular appendages, a process that may clinically mimic testicular torsion or epididymo-orchitis. [8, 9, 10]
Preferred examination
Radiography has no role in the evaluation of epididymitis. The preferred imaging examination is ultrasonography, which is very useful in the detection of the epididymitis and/or epididymo-orchitis (see the following images). Ultrasonography is helpful in distinguishing acute epididymitis from the more ominous testicular torsion. Radiologic studies are recommended in children who have bacteruria and acute epididymitis in order to evaluate for structural abnormalities (found in >50% of these patients). In infants with bacteruria and epididymitis, in whom anatomica abnormalities are more common than in older children, a voiding cystourethrogram (VCUG) and abdominal ultrasonography are recommended. Retrograde urethrography is also indicated to evaluate for urethral stricture disease as symptoms dictate. [11, 9, 12, 13, 14, 10, 5, 15]
Color Doppler ultrasonography is important in the diagnostic workup of epididymitis, not only for diagnosing epididymitis but to rule out testicular torsion. The sensitivity for torsion in color Doppler ultrasonography is 82-100%, and the specificity is 88.9-100%. The sensitivity of color Doppler ultrasonography for epididymitis is 92-100%. This test is the most widely available; however, it is examiner-dependent. The effectiveness of the examination can be limited by pain and patient size (eg, infants). It should also be reserved for patients with indeterminate examination, history, or laboratory workup findings. [14, 15, 16]
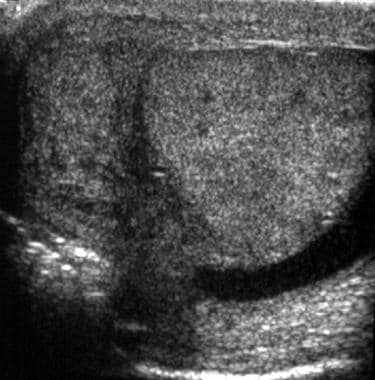 Transverse ultrasonogram of the testis shows an enlarged and predominantly hypoechoic epididymis with a reactive hydrocele in a patient with acute epididymitis.
Transverse ultrasonogram of the testis shows an enlarged and predominantly hypoechoic epididymis with a reactive hydrocele in a patient with acute epididymitis.
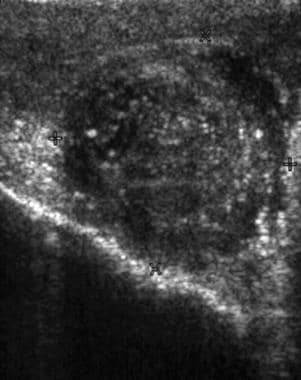
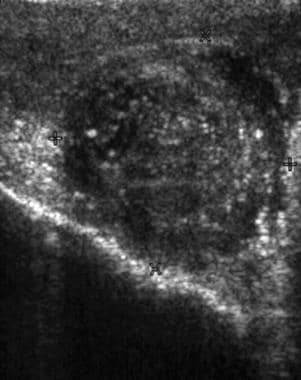
 Color-flow ultrasonogram shows increased vascularity in the epididymis. An enlarged epididymis with increased vascularity in the appropriate clinical setting is diagnostic of acute epididymitis.
Color-flow ultrasonogram shows increased vascularity in the epididymis. An enlarged epididymis with increased vascularity in the appropriate clinical setting is diagnostic of acute epididymitis.
 This ultrasonogram shows an enlarged epididymis with heterogeneous echotexture in a case of acute epididymitis.
This ultrasonogram shows an enlarged epididymis with heterogeneous echotexture in a case of acute epididymitis.
Guidelines
According to American College of Radiology (ACR) appropriateness criteria for acute onset of scrotal pain, patients in whom there is a strong clinical suspicion for testicular torsion can be promptly referred for scrotal exploration. Color Doppler ultrasonography (CDU) with grayscale imaging and special attention to the spermatic cord is the study of choice to evaluate patients with acute scrotal pain due to its widespread availability and its ability to diagnose testicular torsion with a high degree of sensitivity and specificity and to distinguish other causes of scrotal pain and swelling. Additional recommendations include the following [8]
-
Radionuclide scrotal imaging (RNSI) is infrequently used due to longer examination times, less availability, use of radiation, and diminished diagnostic capability in young boys.
-
If CDU results are equivocal for testicular torsion, scrotal exploration is required
-
Future studies are needed to evaluate the role of MRI in patients with acute scrotal pain who have equivocal CDU findings.
The European Society of Urogenital Radiology (ESUR) recommends MRI as an adjunct diagnostic tool for the characterization of both intratesticular and paratesticular masses, especially when sonographic findings are equivocal. MRI is also recommended in the rare cases when discrimination between intratesticular and paratesticular masses is impossible, based on the sonographic characteristics alone. The recommended MRI protocol should include T1-, T2-weighted imaging, diffusion-weighted imaging and dynamic contrast-enhanced MRI.The ESUR notes that the added information provided by MRI may often allow a more conservative therapeutic plan to be used, obviating the need for surgical explorations or radical orchiectomy. [17]
Anatomy
Normal testes develop in the celom and begin to descend into the scrotum at 36 weeks' gestation, guided by the contractile, cordlike structure called the gubernaculum testis. The epididymis and ductus deferens develop from the wolffian ducts.
At sonography, a normal adult testis has medium-level echoes and measures 5 x 3 x 2 cm. Septa extend from the tunica albuginea into the testicle, dividing the testes into lobules. The posterior surface of the tunica albuginea is reflected into the interior of the gland to form the incomplete septum known as the mediastinum of the testis. Each lobule is composed of many seminiferous tubules that open, via tubules (tubuli recti), into dilated spaces called the rete testes in the mediastinum. These, in turn, communicate via efferent ductules in the epididymal head.
The epididymis is composed of a head, body, and tail, the ducts of which continue as the vas deferens in the spermatic cord. The epididymis lies superior and lateral, along the posterior aspect of the testis; the head of epididymis is the most cephalic part.
Four testicular appendages have been described; however, only 2 are clinically relevant: the appendix of the testis (müllerian duct remnant) and the appendix of the epididymis, a wolffian duct remnant. Sonographically, the head of the epididymis is better depicted in the longitudinal view than in others. It is an isoechoic or slightly hypoechoic structure with medium-level echoes. Usually, the body of the epididymis is not identified at sonography in healthy adults. Sometimes, the epididymal tail is seen.
Differential Diagnoses
The following should be considered in the differential diagnosis:
-
Acute idiopathic scrotal edema
Acute epididymitis generally presents as the gradual onset of posterior scrotal pain and swelling over one to two days. There may be concurrent symptoms of fever, hematuria, dysuria, and urinary frequency, and the pain may radiate into the lower abdomen. In contrast, torsion of the testis or appendix testis (vestigial tissue along the testis) presents as the sudden onset of severe unilateral pain, often associated with nausea and vomiting but without fever or other urologic symptoms. A history of intermittent scrotal pain is uncommon in epididymitis or torsion of the testicular appendages but may occur with intermittent testicular torsion. [4]
Testicular cancer and trauma may also cause scrotal pain. The typical patient presentation for paratesticular rhabdomyosarcoma (RMS) is a painless scrotal mass, or symptoms of metastasis, such as inguinal lymphadenopathy, fatigue, decreased appetite and weight loss. A paratesticular RMS can cause pain when it oppresses the nerve. However, pain is extremely uncommon and present in only 7% of the cases. When patients present with a painful, edematous scrotum, they are often misdiagnosed with epididymitis. [18, 19]
It is also important to consider an inguinal hernia because it may also present as a swollen, tender scrotum. With an inguinal hernia, bowel sounds may be auscultated within the scrotum. [4]
Ultrasonography
Ultrasonography is the first-line imaging modality for evaluating a patient with suspected acute epididymo-orchitis. The sensitivity of color Doppler ultrasonography in detecting scrotal inflammation is almost 100%. [20] Usually, no false-positive or false-negative findings occur. However, the epididymis may be involved in some patients with testicular torsion. Hence, in every case of epididymitis, intratesticular blood flow should be carefully evaluated to exclude the possibility of acute testicular torsion. [15, 21, 20, 22, 23, 16, 24, 25, 26]
Ultrasonographic findings considered diagnostic of acute epididymitis include an enlarged (>17 mm) epididymis with a hypoechoic, hyperechoic, or heterogeneous echotexture (gray-scale ultrasonography) and increased blood flow (color or power Doppler ultrasonography) (see the images below). [10] Associated reactive hydrocele and scrotal wall thickening may be present. Blood flow can be seen in a normal epididymis; therefore, the mere presence of blood flow should not be considered the sine qua non of epididymitis. It is the asymmetrical increase (more in the affected epididymis) that is important. [21] Abscess formation may complicate acute epididymitis and appears as an avascular hypoechoic area within the epididymis. [20]
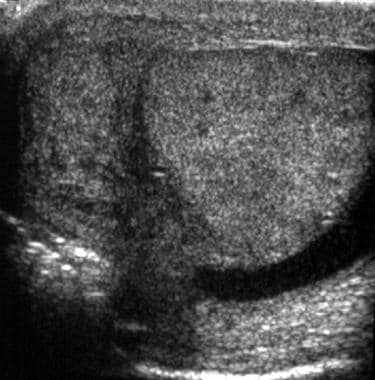 Transverse ultrasonogram of the testis shows an enlarged and predominantly hypoechoic epididymis with a reactive hydrocele in a patient with acute epididymitis.
Transverse ultrasonogram of the testis shows an enlarged and predominantly hypoechoic epididymis with a reactive hydrocele in a patient with acute epididymitis.
 Color-flow ultrasonogram shows increased vascularity in the epididymis. An enlarged epididymis with increased vascularity in the appropriate clinical setting is diagnostic of acute epididymitis.
Color-flow ultrasonogram shows increased vascularity in the epididymis. An enlarged epididymis with increased vascularity in the appropriate clinical setting is diagnostic of acute epididymitis.
 This ultrasonogram shows an enlarged epididymis with heterogeneous echotexture in a case of acute epididymitis.
This ultrasonogram shows an enlarged epididymis with heterogeneous echotexture in a case of acute epididymitis.
The epididymis is primarily involved in epididymo-orchitis, with orchitis developing in about 20-40% of cases by means of direct spread. [20] Diffuse testicular involvement is confirmed with testicular enlargement and an inhomogeneous echotexture. These findings are nonspecific, but acute epididymo-orchitis is the most common disease with this pattern. This pattern of heterogeneous echotexture can also occur in patients with tumors, metastasis, and infarction. Therefore, patients with these conditions should be followed up with ultrasonography to demonstrate complete resolution.
The readily detectable intratesticular venous flow is highly suggestive of orchitis. Analysis of the spectral waveform also can provide useful information. In the testes of a healthy volunteer, the resistive index (RI) is rarely less than 0.5, but more than half of the patients with epididymo-orchitis have an RI of less than 0.5.
In a retrospective study by Boettcher et al to differentiate torsion of the appendix testis from epididymitis, the best predictors for epididymitis were found to be dysuria, a painful epididymis on palpation, and altered epididymal echogenicity and increased peritesticular perfusion on ultrasound. The best predictor for torsion of the appendix testis was a positive blue dot sign (a tender nodule with blue discoloration on the upper pole of the testis). [27]
Magnetic resonance imaging (MRI)
MRI techniques are not typically used for the acute scrotum due to the limited availability of equipment and the long examination time involved. However, the use of MRI in scrotal diseases is increasing. High spatial resolution and a large field of view make MRI an ideal second-level technique when sonographic findings are equivocal, [22, 23, 17]
A retrospective study reported that MRI has a 93% sensitivity and 100% specificity for diagnosing testicular torsion. The most sensitive finding in torsion is decreased or lack of perfusion on dynamic contrast-enhanced MRI. Other characteristics include low or very low signal intensities with spotty or streaky patterns on fat-suppressed T2-weighted, heavily T2-weighted, or T2*-weighted images. The use of a combination of dynamic contrastenhanced T1-weighted MR imaging with T2- and T2*-weighted sequences may help distinguish patients with torsion alone from those with torsion and hemorrhagic necrosis. [8]
Nuclear Imaging
Radionuclide scrotal imaging (RNSI) is an alternative method for evaluating epididymitis. However, because of the improved capability of color and power Doppler ultrasonography in the evaluation of testicular perfusion, this modality is no longer favored. [8] The most common scenario in which epididymitis appears on scintigrams is in patients who undergo imaging for suspected torsion. Nuclear medicine studies can help differentiate epididymo-orchitis from acute torsion. Increased radionuclide uptake may be present in the setting of trauma. A potential pitfall is that photon-deficient areas secondary to hydrocele, spermatocele, and rarely an inguinal hernia can be mistaken for an avascular testis. [8]
The radionuclide angiogram obtained with technetium-99m (99m Tc) pertechnetate reveals increased spermatic cord blood flow. Static images reveal increased radiotracer uptake, which may be focal (as in epididymitis) or diffuse (as in epididymo-orchitis), in the involved hemiscrotum. These findings should easily differentiate epididymitis from acute torsion. However, if an abscess or hydrocele formation is present, a photopenic area with a hypervascular rim (halo sign) can be apparent. This finding could potentially mimic late, missed torsion.
Problems in examination performance may arise in infants and very small children whose genitalia are small and therefore difficult to image. The unavailability of RNSI equipment in many radiology practices as well as its use of ionizing radiation, its poor anatomical detailing, and the time required for RNSI examinations are also limiting factors. [8]
-
Transverse ultrasonogram of the testis shows an enlarged and predominantly hypoechoic epididymis with a reactive hydrocele in a patient with acute epididymitis.
-
Color-flow ultrasonogram shows increased vascularity in the epididymis. An enlarged epididymis with increased vascularity in the appropriate clinical setting is diagnostic of acute epididymitis.
-
This ultrasonogram shows an enlarged epididymis with heterogeneous echotexture in a case of acute epididymitis.





