Practice Essentials
Spondylodiscitis (spondylodiskitis, infectious spondylitis) is an infection that involves one or more of the extradural components of the spine. Although it affects a small proportion (2-7%) of all patients with osteomyelitis, it is important because of its potential morbidity and mortality. Infectious spondylitis most commonly appears as spinal osteomyelitis and/or diskitis. Its complications include paraspinal and epidural abscess formation. [1, 2, 3, 4, 5, 6, 7]
The disease is most often seen in older adults (older than 60 years), but it can occur at any age. Risk factors include diabetes mellitus, immunosuppression, IV drug use, malnutrition, rheumatic disease, and spinal surgery. [8, 9]
Pyogenic spinal infections most commonly are caused by Staphylococcus aureus (in > 50% of patients) and Enterobacter species (in 30% of patients). Osteomyelitis caused by Salmonella is most often seen in patients with sickle cell disease. [10] Pseudomonas aeruginosa, Serratia species, and Candida species most often affect patients with a history of intravenous drug abuse. Mycobacterium tuberculosis causes most nonpyogenic spinal infections; however, fungi (eg, Cryptococcus species, Aspergillus species, coccidioidomycosis) also may cause infections. [1, 2, 11, 12, 13]
The spondylodiscitis diagnosis is made by a combination of clinical, laboratory, and radiologic findings. Symptoms and clinical signs of spondylodiscitis include severe back pain, fever, and neurologic deficits (eg, leg weakness, paralysis, sensory deficit, radiculopathy, loss of sphincter control). Laboratory results may include elevated levels of C-reactive protein, increased erythrocyte sedimentation rate, and elevated white blood cell count. [8, 9, 14, 15, 16]
(The characteristics of spondylodiskitis as they appear on radiographs, CT scans, and MRI scans are demonstrated in the images below.)
 Fluoroscopy-guided radiograph shows how disk aspiration may be used to direct an image-guided procedure. This image also demonstrates the relatively subtle changes of spondylodiskitis on radiography. Although early loss of the disk space may be present, no definite endplate erosion is seen. MRI findings were supportive of infection; the biopsy was culture positive for Staphylococcus aureus.
Fluoroscopy-guided radiograph shows how disk aspiration may be used to direct an image-guided procedure. This image also demonstrates the relatively subtle changes of spondylodiskitis on radiography. Although early loss of the disk space may be present, no definite endplate erosion is seen. MRI findings were supportive of infection; the biopsy was culture positive for Staphylococcus aureus.
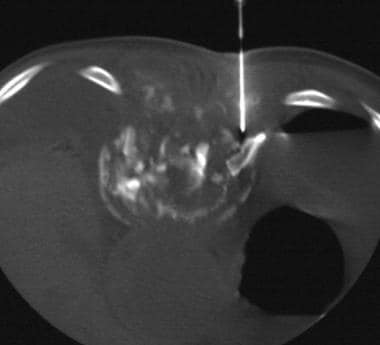 This image of a CT-guided biopsy of diskitis/osteomyelitis demonstrates extensive destruction and fragmentation of the vertebral body resulting from spondylodiskitis. CT-guided percutaneous needle aspiration and biopsy were performed to obtain material for cultures to direct appropriate antibiotic therapy.
This image of a CT-guided biopsy of diskitis/osteomyelitis demonstrates extensive destruction and fragmentation of the vertebral body resulting from spondylodiskitis. CT-guided percutaneous needle aspiration and biopsy were performed to obtain material for cultures to direct appropriate antibiotic therapy.
 Diskitis/osteomyelitis is seen on this T2-weighted MRI of the lumbar spine, which demonstrates destruction of the L3-4 disk space with the adjacent endplate and/or vertebral body. L3 and L4 vertebral bodies show increased T2 signal, indicating edema and/or infarction. Also shown is a retropulsion of debris, which compresses the thecal sac.
Diskitis/osteomyelitis is seen on this T2-weighted MRI of the lumbar spine, which demonstrates destruction of the L3-4 disk space with the adjacent endplate and/or vertebral body. L3 and L4 vertebral bodies show increased T2 signal, indicating edema and/or infarction. Also shown is a retropulsion of debris, which compresses the thecal sac.
Preferred examination
Although plain images, radiographs, CT scans, and nuclear medicine studies can help establish the diagnosis of spondylodiskitis, MRI is considered the modality of choice for evaluating the presence and severity of spinal infection. MRI is especially effective for evaluating the neural structures of the spine (ie, spinal cord, nerve roots) and extradural soft tissue. It is less effective for treatment response evaluation. [17] Along with appropriate history taking, physical examination, and positive blood cultures, findings on MRI or radionuclide studies may confirm the diagnosis. [18, 9]
Contrast-enhanced MRI is the method of choice because of high contrast resolution, high sensitivity for soft tissue, absence of ionizing radiation, and ability to show evidence of bone marrow abnormalities. MRI cannot be performed in patients with cardiac implantable electronic devices, cardioverter defibrillators, or cardiac resynchronization devices. The primary MRI findings for spondylodiscitis are impairment of the intervertebral discs associated with disc space narrowing or possible epidural involvement and increased contrast enhancement in the spine. High cost and long run times for whole-spine examination are drawbacks, along with the fact that MRI diagnostic performance decreases in follow-up evaluation and in postoperative infection of the spine. [19, 20, 21, 22, 23]
The use of 18F-fluorodeoxyglucose-positron emission tomography (18-FDG-PET) for evaluating spondylodiscitis has shown great promise. The drawback of reduced image quality regarding anatomical information has been overcome in studies by a combined simultaneous acquisition of CT or MRI. [24, 25, 26, 27, 28, 29, 30] In a study by Altini et al, 18F-FDG PET/CT compared favorably with MRI. The sensitivity, specificity, and accuracy for 18F-FDG PET/CT were 92%, 100%, and 94%; and for MRI, sensitivity, specificity, and accuracy were 100%, 60%, and 97%, respectively. [14]
CT scanning is most useful for characterizing vertebral osteomyelitis in patients with subacute or chronic illness. CT scanning provides radiologic guidance for interventional procedures (ie, biopsy, drainage). [31]
Generally, plain radiography is the first imaging modality used for suspected spinal infection, despite low sensitivity and specificity. Signs of spondylodiscitis are usually not present on radiographs until 2-8 weeks after the onset of symptoms. [14, 16, 32, 33, 34] Conventional radiographs are insensitive to the acute changes seen in cases of spondylodiskitis, but they may be used on a limited basis in the follow-up of chronically ill patients.
Invasive methods may be required to establish a diagnosis of spondylodiskitis. Spinal biopsy may be performed as an open surgical procedure or as an image-guided percutaneous procedure. The morbidity rate associated with percutaneous image-guided biopsy (eg, with CT scanning or fluoroscopy) is lower than the morbidity rate associated with open biopsy. Percutaneous biopsy may be highly sensitive and specific. Multiple samples should be obtained and submitted in appropriate containers for Gram staining, acid-fast bacillus smears, fungal staining, and culturing. [4, 35]
Limitations of techniques
MRI is relatively expensive. In addition, it is contraindicated in patients with certain implanted medical devices (eg, pacemakers), and it is not tolerated by all patients because of claustrophobia or morbid obesity. Good MRIs require the cooperation of the patient; the quality of MRI is degraded by motions of the patient. Use of a gadolinium-based intravenous contrast agent is strongly recommended.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). NSF/NFD has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
CT scanning is quick and inexpensive, although it exposes the patient to ionizing radiation. In addition, it is associated with a low risk of an allergic reaction to the intravenous contrast agent, though detection of bone destruction or a paraspinal mass does not require the use of contrast material.
Radionuclide studies may be time consuming, and spatial resolution may be low.
With plain radiographs, results are often normal or nonspecific in patients with acute spinal infection.
Radiography
Conventional radiography is insensitive to the early changes of spondylodiskitis. In the acute setting, radiographs are normal. In the subacute period (1-3 wk), reduced disk-space height and/or endplate erosion may be evident. In the chronic period (>10 wk), vertebral body sclerosis or collapse may be observed on either side of a narrowed disk space. Paraspinal soft-tissue opacity may develop. Gradual disk obliteration may occur with fusion (ie, osseous, fibrous). Partial restoration of disk height may be observed with successful treatment.
Plain radiographic findings suggestive of subacute or chronic spondylodiskitis, such as disk-space loss, endplate erosion, and vertebral sclerosis, should be correlated with the patient's clinical history. In cases of spondylodiskitis, radiographic findings lag behind clinical response to treatment by approximately 1 month.
(See the image below.)
 Fluoroscopy-guided radiograph shows how disk aspiration may be used to direct an image-guided procedure. This image also demonstrates the relatively subtle changes of spondylodiskitis on radiography. Although early loss of the disk space may be present, no definite endplate erosion is seen. MRI findings were supportive of infection; the biopsy was culture positive for Staphylococcus aureus.
Fluoroscopy-guided radiograph shows how disk aspiration may be used to direct an image-guided procedure. This image also demonstrates the relatively subtle changes of spondylodiskitis on radiography. Although early loss of the disk space may be present, no definite endplate erosion is seen. MRI findings were supportive of infection; the biopsy was culture positive for Staphylococcus aureus.
Computed Tomography
In spondylodiskitis, CT scans may appear normal early in the course of disease. Disk-space narrowing or decreased attenuation in the disk is often the earliest manifestation of disease. After the administration of iodinated contrast material, the abnormal disk space, vertebral marrow, or paravertebral soft tissues may enhance. [31, 36]
As the disease progresses, destruction of the vertebral body and fragmentation of vertebral endplates are observed. Destruction may be either diffuse or permeative. The presence of paraspinal soft tissue lesions and/or collections aids in the diagnosis of spondylodiskitis. In children, extrusion of the vertebral body may be observed. [37]
Overall, CT scanning is more sensitive (68%), more specific (97%), and more accurate (80%) than plain radiography in identifying areas of vertebral osteomyelitis in animal models.
Because of its ease and speed of use, lower cost, and availability, CT scanning is an excellent method for evaluating the bony changes of spondylodiskitis and for directing radiologic intervention (ie, aspiration or biopsy; see the image below) in spinal infections. In the diagnosis of active bacterial disk-space infections, the sensitivity and specificity of CT-guided percutaneous aspiration may be as high as 91% and 100%, respectively; however, percutaneous aspiration is less reliable in the diagnosis of nonbacterial infections.
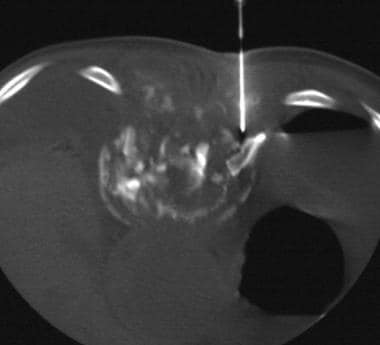 This image of a CT-guided biopsy of diskitis/osteomyelitis demonstrates extensive destruction and fragmentation of the vertebral body resulting from spondylodiskitis. CT-guided percutaneous needle aspiration and biopsy were performed to obtain material for cultures to direct appropriate antibiotic therapy.
This image of a CT-guided biopsy of diskitis/osteomyelitis demonstrates extensive destruction and fragmentation of the vertebral body resulting from spondylodiskitis. CT-guided percutaneous needle aspiration and biopsy were performed to obtain material for cultures to direct appropriate antibiotic therapy.
Gas in the disk space (ie, vacuum phenomenon) may occasionally be observed on CT scans. Although this finding is most often associated with degenerative disk disease, it may also occur with infection.
CT scanning is less sensitive than MRI in depicting soft tissue structures, but its sensitivity may be improved with the use of intravenous contrast material.
Magnetic Resonance Imaging
MRI is the modality of choice for evaluating spinal infections. Contrast-enhanced MRI is the method of choice because of high contrast resolution, high sensitivity for soft tissue, absence of ionizing radiation, and ability to show evidence of bone marrow abnormalities. [19, 20, 21, 22, 23] In particular, MRI is useful in detecting abnormalities during the acute stage of spinal infection. MRI is 96% sensitive, 92% specific, and 94% accurate in the evaluation of spondylodiskitis. During the acute stage, MRI may demonstrate increased signal intensity on T2-weighted images in the vertebral body or disk space caused by infarction, abscess, or edema (see the image below). MRI cannot be performed in patients with cardiac implantable electronic devices, cardioverter defibrillators, or cardiac resynchronization devices. The primary MRI findings for spondylodiscitis are impairment of the intervertebral discs associated with disc space narrowing or possible epidural involvement and increased contrast enhancement in the spine.
On T1-weighted images, decreased signal intensity may be observed in the disk and adjacent endplates as a result of edema, and the margin between the disk and the endplate may be diminished. The multiplanar capability of MRI allows excellent anatomic localization of the extent of infection, as well as full evaluation of the spinal cord and nerve roots. MRI is also useful for the evaluation of postoperative spinal infections and for the follow-up evaluation of treatment of spondylodiskitis. Fat-suppression sequences with contrast-enhanced T1-weighted imaging should be routinely performed. [5, 38, 39, 40, 41, 42]
 Diskitis/osteomyelitis is seen on this T2-weighted MRI of the lumbar spine, which demonstrates destruction of the L3-4 disk space with the adjacent endplate and/or vertebral body. L3 and L4 vertebral bodies show increased T2 signal, indicating edema and/or infarction. Also shown is a retropulsion of debris, which compresses the thecal sac.
Diskitis/osteomyelitis is seen on this T2-weighted MRI of the lumbar spine, which demonstrates destruction of the L3-4 disk space with the adjacent endplate and/or vertebral body. L3 and L4 vertebral bodies show increased T2 signal, indicating edema and/or infarction. Also shown is a retropulsion of debris, which compresses the thecal sac.
Paraspinal and epidural abscesses generally appear isointense to muscle on T1-weighted images and hyperintense on fat-saturated T2-weighted or short-tau inversion recovery (STIR) images.
Abscesses of the vertebral body may appear more conspicuous on diffusion-weighted images (DWIs) than on conventional T1- or T2-weighted images.
On contrast-enhanced MRIs, an epidural abscess may appear as an area of peripheral enhancement (as seen in the image below) surrounding an area of fluid signal intensity; it may also appear as an area of abnormal enhancement of disk, vertebral marrow, or paraspinal soft tissue.
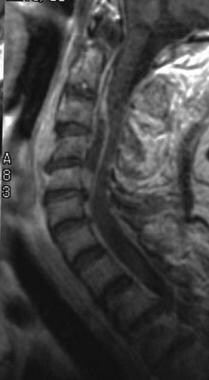 The epidural abscess on this contrast-enhanced T1-weighted MRI demonstrates the loss of disk-space height, which is most prominent at C4-5 and C5-6. A large, peripherally enhancing epidural abscess extends from C5-6 to the C2 level. The thecal sac and cord are compressed.
The epidural abscess on this contrast-enhanced T1-weighted MRI demonstrates the loss of disk-space height, which is most prominent at C4-5 and C5-6. A large, peripherally enhancing epidural abscess extends from C5-6 to the C2 level. The thecal sac and cord are compressed.
Signal and enhancement changes may persist after clinical resolution of the infection; such findings gradually decrease over weeks to months. This illustrates the fact that contrast enhancement is not always indicative of active infection. These changes do not occur as rapidly as with gallium scanning.
False-negative findings may occur in patients with spondylodiskitis caused by organisms of low virulence (eg, diphtheroids, coagulase-negative staphylococci).
Nuclear Imaging
Radionuclide studies are useful for early detection (3-15 days) of spinal infection. However, establishing this diagnosis may be more difficult in the spine than in other areas of the skeleton because of the presence of active bone marrow. On 3-phase technetium-99m (99mTc) scintigraphy, osteomyelitis is characterized by nonspecific arterial hyperemia and the progressive focal skeletal uptake of tracer. Bone scan specificity may be increased by combining 99mTc with an indium-111–labeled WBC or gallium-67 (67Ga) scans. Ga-67 functions as an acute-phase reactant, accumulating in areas of inflammation. In-111-labeled WBCs also accumulate in areas of infection and inflammation. Areas of infection should appear hotter on the 67Ga scan than on the accompanying 99mTc scan. Infective lesions may appear hot or cold on 111In WBC scans. Ga-67 scans may normalize after satisfactory treatment, and they may be used to monitor treatment response. The use of single-photon emission CT (SPECT) enhances the 3-dimensional localization of infection. [43, 44, 24, 25, 26, 27, 45]
The use of 18F-fluorodeoxyglucose-positron emission tomography (18-FDG-PET) for evaluating spondylodiscitis has shown great promise. The drawback of reduced image quality regarding anatomical information has been overcome in studies by a combined simultaneous acquisition of CT or MRI. [24, 25, 26, 27, 28, 29] In a study by Altini et al, 18F-FDG PET/CT compared favorably with MRI. The sensitivity, specificity, and accuracy for 18F-FDG PET/CT were 92%, 100%, and 94%; and for MRI, sensitivity, specificity, and accuracy were 100%, 60%, and 97%, respectively. [14]
Nuclear scintigraphy is sensitive for vertebral osteomyelitis; however, increased bone turnover from surgery, fracture, or degenerative changes decreases specificity.
False-negative results may occur when atherosclerosis or primary bone destruction compromises blood flow to a lesion.
Use of 111In WBCs may increase the specificity of bone scanning; however, the images may be falsely negative in patients with chronic osteomyelitis or falsely positive in patients with inflammatory or reactive conditions such as rheumatoid arthritis and fractures.
In a study by Tamm et al of 34 patients assessed for spondylodiscitis, bone (99mTc-methylene diphosphonate) or gallium-67 SPECT-CT and MRI had similar sensitivities (0.94 vs 0.94), specificities (1.00 vs 1.00), positive predictive values (1.00 vs 1.00), negative predictive values (0.94 vs 0.80), and accuracies (0.97 vs 0.95). [46]
In a retrospective analysis by Smids et al of 68 patients with a clinical suspicion of spondylodiscitis, who had an infection or fever of unknown origin, MRI had an overall sensitivity of 67% and specificity of 84%, and 18F-FDG-PET/CT had a sensitivity of 96% and a specificity of 95%. Diagnostic accuracy was 58% when MRI was performed within 2 weeks after the start of symptoms, and it improved to 82% when performed more than 2 weeks after onset of symptoms; 18F-FDG-PET/CT displayed no relation to the interval between the scan and the start of symptoms. [26]
-
Fluoroscopy-guided radiograph shows how disk aspiration may be used to direct an image-guided procedure. This image also demonstrates the relatively subtle changes of spondylodiskitis on radiography. Although early loss of the disk space may be present, no definite endplate erosion is seen. MRI findings were supportive of infection; the biopsy was culture positive for Staphylococcus aureus.
-
Spread from an adjacent source, such as a psoas abscess, is an uncommon infection route in spondylodiskitis. These T2-weighted MRI scans show a large, right psoas abscess with epidural extension. Despite the large fluid collection, results of percutaneous biopsy were culture negative. The patient was treated with intravenous antibiotics before the procedure.
-
Diskitis/osteomyelitis is seen on this T2-weighted MRI of the lumbar spine, which demonstrates destruction of the L3-4 disk space with the adjacent endplate and/or vertebral body. L3 and L4 vertebral bodies show increased T2 signal, indicating edema and/or infarction. Also shown is a retropulsion of debris, which compresses the thecal sac.
-
The epidural abscess on this contrast-enhanced T1-weighted MRI demonstrates the loss of disk-space height, which is most prominent at C4-5 and C5-6. A large, peripherally enhancing epidural abscess extends from C5-6 to the C2 level. The thecal sac and cord are compressed.
-
This image of a CT-guided biopsy of diskitis/osteomyelitis demonstrates extensive destruction and fragmentation of the vertebral body resulting from spondylodiskitis. CT-guided percutaneous needle aspiration and biopsy were performed to obtain material for cultures to direct appropriate antibiotic therapy.

