Practice Essentials
Diffuse axonal injury (DAI) is a frequent result of traumatic acceleration/deceleration or rotational injuries and a frequent cause of persistent vegetative state in patients. In fact, DAI represents approximately one half of all intra-axial traumatic lesions. [1] This lesion is the most significant cause of morbidity in patients with traumatic brain injuries, which most commonly result from high-speed motor vehicle accidents. [2] Any patient with a closed head injury who experiences extensive loss of consciousness and neurologic deficits warrants neuroimaging. [3] Diffuse axonal injury typically consists of several focal white-matter lesions measuring 1-15 mm in a characteristic distribution. [4]
(See the images below.)
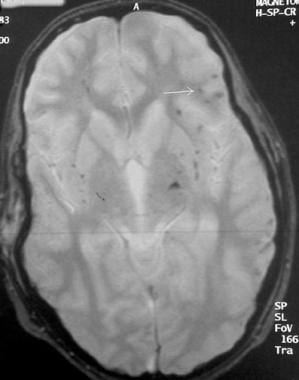
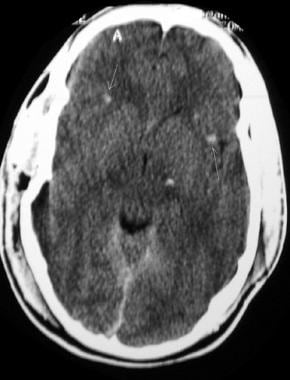 Noncontrast computed tomography scan of a trauma patient demonstrates multiple petechial hemorrhages (arrows) consistent with diffuse axonal injury. Note that the hemorrhages are characteristically located at the gray-white matter interface.
Noncontrast computed tomography scan of a trauma patient demonstrates multiple petechial hemorrhages (arrows) consistent with diffuse axonal injury. Note that the hemorrhages are characteristically located at the gray-white matter interface.
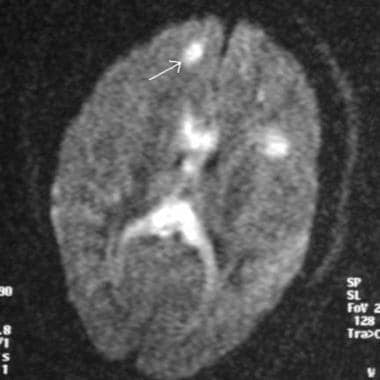 Magnetic resonance imaging diffusion sequence demonstrating multiple foci of abnormal increased signal at the gray-white matter junction (arrow) and within the corpus callosum in a patient with diffuse axonal injury
Magnetic resonance imaging diffusion sequence demonstrating multiple foci of abnormal increased signal at the gray-white matter junction (arrow) and within the corpus callosum in a patient with diffuse axonal injury
Classically, DAI has been considered a primary-type injury, with damage occurring at the time of the accident. Research has shown that another component of the injury comprises the secondary factors (or delayed component), since the axons are injured, secondary swelling occurs, and retraction bulbs form. Of patients with DAI, 80% demonstrate multiple areas of injury on CT scans.
The degree of microscopic injury usually is considered to be greater than that seen on diagnostic imaging, and the clinical findings reflect this point. DAI is suggested in any patient who demonstrates clinical symptoms disproportionate to his or her CT scan findings. DAI results in instantaneous loss of consciousness, and most patients (>90%) remain in a persistent vegetative state, since brainstem function typically remains unaffected. DAI rarely causes death.
Imaging modalities
Magnetic resonance imaging (MRI) is the preferred examination for DAI (particularly with gradient-echo sequences), although CT scanning may demonstrate findings suggestive of DAI and is more practical and available. [3, 5, 6, 7, 8, 9, 10, 4, 11] Studies have indicated that MRI can play a role in predicting the length of coma in DAI patients. However, MRI is contraindicated in patients with implanted pacemakers or certain types of metallic prostheses, as well as in patients who have metallic foreign bodies, such as bullet fragments, in their head or neck or near important vascular structures. In addition, MRI is difficult to perform on patients who have claustrophobia and on ventilator-dependent patients.
Traumatic microbleeds are considered to be a radiologic marker for DAI. Gradient echo-sequence-based susceptibility-weighted imaging has been found to be sensitive and accurate for microbleed detection. [10, 4, 11]
Scoring tools used for traumatic brain injury include the Glasgow Coma Scale, the Rotterdam score on CT, and the DAI grade on MRI. In a study of pediatric patients with traumatic brain injury, Janus et al found that with each 1-point increase in DAI grade, the odds of unfavorable functional outcome increased by 2.4-fold. As noted in other studies, deeper DAI lesions were associated with an increased risk of unfavorable outcome. A higher DAI grade on early MRI was associated with worse 6-month functional outcome and with discharge to inpatient rehabilitation in children with acute moderate to severe traumatic brain injury. Both the Rotterdam CT score and the DAI grade were found to be significantly higher in patients with unfavorable functional outcome. [12, 13, 14, 15, 16]
No specific findings related to diffuse axonal injury can be made using conventional radiography; the degree of confidence is low, as conventional radiography cannot demonstrate subtle soft-tissue changes. However, other signs of head trauma can be appreciated, such as facial bone fractures or fluid levels within the paranasal sinuses. Radiographs can also clearly demonstrate skull fractures, but this is not helpful in DAI, as DAI is rarely associated with skull fracture. Thus, many false negatives are possible, because a negative skull radiograph in no way excludes a parenchymal brain injury.
Nuclear medicine currently has no role in the routine diagnostic workup of patients with possible diffuse axonal injury; however, studies have suggested that iodine-123 (123I) single-photon emission CT (SPECT) imaging demonstrates areas of hypoperfusion in areas of known injury and reveals additional areas of injury not visualized with MRI.
Computed Tomography
Among patients eventually proven to have diffuse axonal injury, 50-80% demonstrate a normal CT scan upon presentation. Delayed CT scanning may be helpful in demonstrating edema or atrophy, which are later findings. Small petechial hemorrhages located at the gray-white matter junction (as seen in the image below), as well as in the corpus callosum and brainstem, are characteristic of CT scan findings in the acute setting. [17]
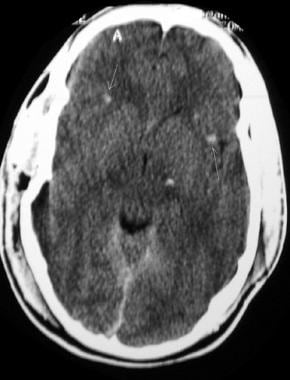 Noncontrast computed tomography scan of a trauma patient demonstrates multiple petechial hemorrhages (arrows) consistent with diffuse axonal injury. Note that the hemorrhages are characteristically located at the gray-white matter interface.
Noncontrast computed tomography scan of a trauma patient demonstrates multiple petechial hemorrhages (arrows) consistent with diffuse axonal injury. Note that the hemorrhages are characteristically located at the gray-white matter interface.
Wang and colleagues [18] suggested using CT scan criteria, including the presence of one or more small intraparenchymal hemorrhages less than 2 cm in diameter located in the cerebral hemispheres; intraventricular hemorrhage; hemorrhage in the corpus callosum; small focal areas of hemorrhage less than 2 cm in diameter adjacent to the third ventricle; and brainstem hemorrhage as characteristic of DAIs. There may also be small focal areas of low density on CT scans; these correspond to areas of edema occurring where shearing injury took place.
The degree of confidence in CT scanning is moderate, as the only finding may be petechial hemorrhage, and fewer than 20% of patients with DAI demonstrate this finding on CT scanning alone. When petechial hemorrhages are observed with the appropriate clinical findings, the sensitivity of CT scanning in the detection of DAI is high.
As with conventional radiographs, frequent false negatives are possible, because normal or almost-normal CT scan findings are common in patients with DAI on initial presentation, as demonstrated in the image below. For this reason, when CT scan findings are negative and DAI is suggested clinically, MRI may be performed, as MRI can demonstrate lesions not observed through CT scanning. However, although MRI is more sensitive in the detection of subtle soft-tissue abnormalities, CT scanning is more available and practical in the current medical environment and is therefore, according to Teasdale, the "mainstay of acute investigation of head injury." [19]
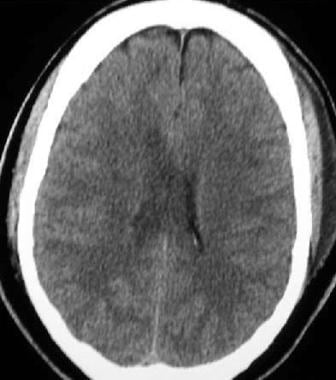 Noncontrast axial computed tomography (CT) scan demonstrates why magnetic resonance imaging (MRI) is the study of choice in diagnosing diffuse axonal injury. This CT scan appears normal, although on closer examination, punctate hypodensities can be observed in the right frontal and left parietal white matter.
Noncontrast axial computed tomography (CT) scan demonstrates why magnetic resonance imaging (MRI) is the study of choice in diagnosing diffuse axonal injury. This CT scan appears normal, although on closer examination, punctate hypodensities can be observed in the right frontal and left parietal white matter.
Magnetic Resonance Imaging
Recommended MRI sequences include T1-weighted, T2-weighted, T2–gradient-echo, proton density–weighted, and diffusion-weighted images. [5, 10, 20] The degree of confidence is high, as abnormal signal in the characteristic locations, discovered in the clinical setting of recent trauma, leaves little doubt about the diagnosis of diffuse axonal injury. In a prospective cohort study, Skandsen et al examined MRI scans from patients in the early phase of moderate to severe head injury and determined the prognosis was better in patients with DAI whose lesions were confined to the lobar white matter or who had callosal lesions than it was in patients with DAI who had lesions in the dorsolateral brainstem. [6]
T1-weighted images are helpful for anatomic localization [21] ; however, nonhemorrhagic lesions may be isointense to surrounding tissue. Hemorrhagic lesions appear hyperintense on T1-weighted images. However, on T2-weighted sequences, nonhemorrhagic lesions appear hyperintense. Diffusion-weighted sequences can reveal hyperintensities in areas of axonal injury.
As demonstrated in the image below, gradient-echo sequences are particularly useful in revealing the paramagnetic effects of petechial hemorrhages. Gradient-echo imaging can often show signal abnormality in areas that appear normal in T1- and T2-weighted spin-echo sequences. For this reason, gradient-echo imaging has become a mainstay of MRI exams for patients with suggested shearing-type injuries. The abnormal signal on gradient-echo images can persist for many years after the injury.
 Gradient-echo axial magnetic resonance image demonstrating numerous small foci of diminished signal consistent with the paramagnetic effect of the hemoglobin content of many acute hemorrhages
Gradient-echo axial magnetic resonance image demonstrating numerous small foci of diminished signal consistent with the paramagnetic effect of the hemoglobin content of many acute hemorrhages
The most common MRI finding of DAI, as seen in the image below, is the presence of multifocal areas of abnormal signal (bright on T2-weighted images) at the white matter in the temporal or parietal corticomedullary junction or in the splenium of the corpus callosum. Other areas that frequently are abnormal include the dorsolateral rostral midbrain and the corona radiata. Eventually, nonspecific atrophic changes are observed.
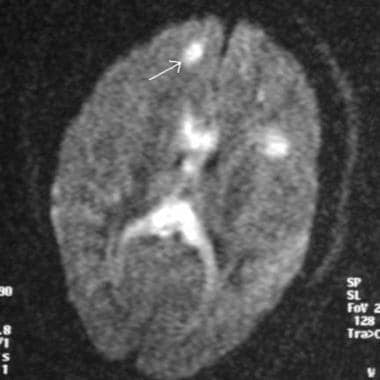 Magnetic resonance imaging diffusion sequence demonstrating multiple foci of abnormal increased signal at the gray-white matter junction (arrow) and within the corpus callosum in a patient with diffuse axonal injury
Magnetic resonance imaging diffusion sequence demonstrating multiple foci of abnormal increased signal at the gray-white matter junction (arrow) and within the corpus callosum in a patient with diffuse axonal injury
Diffusion-weighted imaging (DWI) and the corresponding apparent diffusion coefficient (ADC) differentiate between lesions with increased and decreased diffusion based on the net movement of water molecules. Traditionally, DWI has been used for the diagnosis of acute stroke, given its high sensitivity for acute ischemia; however, DWI has been shown to be sensitive for other cerebral disease processes, including DAI. [22] Characteristic imaging findings on DWI/ADC can be broken down into 3 types: (1) Lesions that are hyperintense on DWI and ADC, (2) lesions that are hyperintense on DWI and hypointense on ADC, and (3) hemorrhagic lesions that are hypointense on DWI and ADC but are surrounded by a hyperintense signal on DWI and ADC. [23] (See the image below.)
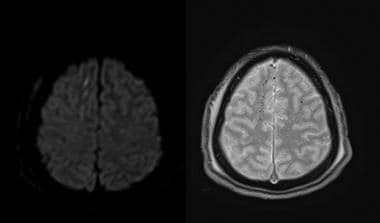 Diffusion-weighted axial image on the left demonstrates multiple foci of increased signal intensity in the right frontal lobe, corresponding to areas that surround hemorrhage. The axial gradient-echo sequence on the right confirms microhemorrhages in the right frontal lobe from diffuse axonal injury (DAI).
Diffusion-weighted axial image on the left demonstrates multiple foci of increased signal intensity in the right frontal lobe, corresponding to areas that surround hemorrhage. The axial gradient-echo sequence on the right confirms microhemorrhages in the right frontal lobe from diffuse axonal injury (DAI).
In a study of magnetic resonance diffusion tensor imaging (MR-DTI) to detect DAI after traumatic brain injury (TBI), a significant reduction in fractional anisotropy (FA) in the corpus callosum was seen in the acute phase. No significant changes were identified in the parallel or perpendicular eigenvalues or trace. At 6 months, a significant reduction in FA and a significant increase in trace and perpendicular eigenvalues were seen. [7]
Studies have reported that the magnetic transfer ratio has shown promise in identifying areas of injury not visible on the above MRI pulse sequences. This may allow the radiologist to appreciate a truer representation of the degree of microscopic injury. Studies have also indicated that MRI can play a role in predicting the length of coma in DAI patients. The volume of white-matter lesions has been correlated to the degree of injury, as measured by MRI. [8] MRI has also been used to quantify cerebral blood flow in damaged areas of the brain, thus predicting injury severity.
In a study of 11 patients with DAI, Sugiyama et al employed voxel-based analysis to investigate the clinical usefulness of DTI and found significantly more brain regions with decreased fractional anisotropy (FA) were found on the DTI scans of patients with DAI than on those of control subjects. [24] In addition, DTI revealed more brain lesions than did conventional MRI. The authors also found that patients' cognitive scores on functional independence and functional assessment measures correlated with the number and size of DAI lesions. Moreover, fiber tractography–based analysis revealed that DAI patients with memory disorders exhibited an interruption of fibers within the fornix. According to Sugiyama and colleagues, their data indicated that DTI is an effective modality for detecting lesions and examining cognitive disorders in patients with DAI. [24]
Multiple sclerosis (MS) is a progressive neurologic disorder that can involve multiple foci of white-matter signal abnormality on MRI; however, MS lesions typically are oval or oblong and are oriented in a direction perpendicular to the border of the lateral ventricles (Dawson fingers). In addition, MS lesions may involve the spinal cord, a finding not associated with DAI, and the clinical course of MS is dramatically different from that of DAI.
False negatives may occur with MRI if only routine sequences are performed. A sequence (such as gradient echo) that accentuates the susceptibility artifact arising from blood products must be performed in order to recognize small petechial hemorrhages.
Benjamin et al have described multidimensional MRI as an emerging approach for diffuse axonal imaging that combines T1-, T2-, and diffusion-weighted images and replaces voxel-averaged values with distributions. [25, 26]
Adams classification
The Adams classification of diffuse axonal injury has been used to grade lesions on MRI, using MRI susceptibility-weighted imaging, as follows [27, 28] :
-
Grade 1: Mild diffuse axonal injury with microscopic white matter changes in the cerebral cortex, corpus callosum, and brainstem.
-
Grade 2: Moderate diffuse axonal injury with gross focal lesions in the corpus callosum.
-
Grade 3: Severe diffuse axonal injury with finding as grade 2 and additional focal lesions in the brainstem.
-
Noncontrast computed tomography scan of a trauma patient demonstrates multiple petechial hemorrhages (arrows) consistent with diffuse axonal injury. Note that the hemorrhages are characteristically located at the gray-white matter interface.
-
Magnetic resonance imaging diffusion sequence demonstrating multiple foci of abnormal increased signal at the gray-white matter junction (arrow) and within the corpus callosum in a patient with diffuse axonal injury
-
Gradient-echo axial magnetic resonance image demonstrating numerous small foci of diminished signal consistent with the paramagnetic effect of the hemoglobin content of many acute hemorrhages
-
Fluid-attenuated inversion recovery sequence demonstrating edema within the corpus callosum (arrow) secondary to traumatic shearing injury. Note that other areas of edema are observed in this patient with diffuse axonal injury.
-
Noncontrast axial computed tomography (CT) scan demonstrates why magnetic resonance imaging (MRI) is the study of choice in diagnosing diffuse axonal injury. This CT scan appears normal, although on closer examination, punctate hypodensities can be observed in the right frontal and left parietal white matter.
-
Diffusion-weighted axial image on the left demonstrates multiple foci of increased signal intensity in the right frontal lobe, corresponding to areas that surround hemorrhage. The axial gradient-echo sequence on the right confirms microhemorrhages in the right frontal lobe from diffuse axonal injury (DAI).







