Practice Essentials
Agenesis of the corpus callosum (ACC) is the complete or partial absence of corpus callosum and is one of the most common congenital cerebral malformations. The corpus callosum is the largest white matter structure of the brain. Fetal ultrasonography can detect ACC as early as the 16th week of gestation. Agenesis of the corpus callosum (ACC) is an anomaly that may occur in isolation or in association with other central nervous system (CNS) or systemic malformations. Because the corpus callosum may be partially or completely absent, the term dysgenesis has also been used to describe the spectrum of callosal anomalies. The normal appearance of the corpus callosum, along with the appearance on magnetic resonance imaging (MRI) of partial and complete ACC, are shown below. [1, 2, 3, 4, 5, 6]
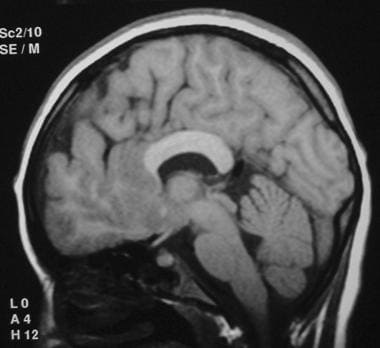
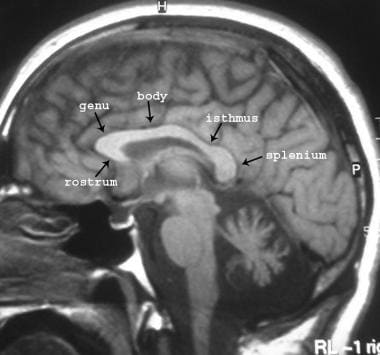 Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows the normal appearance of the corpus callosum.
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows the normal appearance of the corpus callosum.
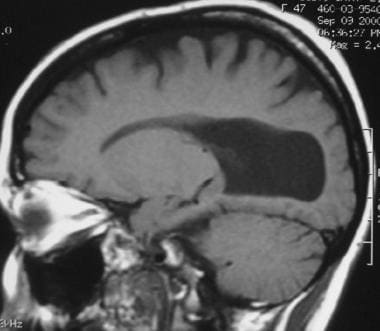
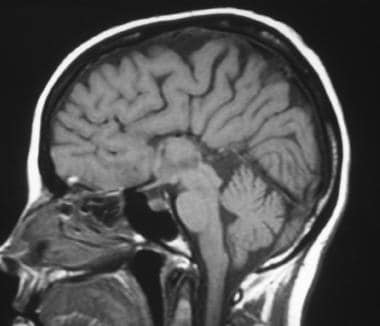 Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows complete absence of the corpus callosum. The cingulate sulcus is absent, and the medial hemispheric sulci reach the third ventricle in a radial fashion.
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows complete absence of the corpus callosum. The cingulate sulcus is absent, and the medial hemispheric sulci reach the third ventricle in a radial fashion.
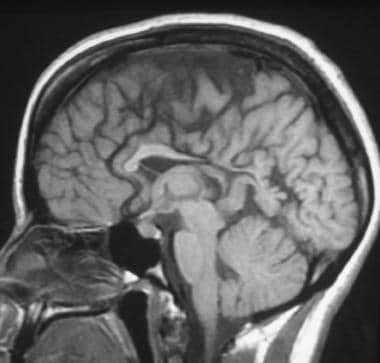 Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows partial agenesis of the corpus callosum. The genu and anterior body of the corpus callosum are visualized, whereas the posterior body, splenium, and rostrum are absent.
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows partial agenesis of the corpus callosum. The genu and anterior body of the corpus callosum are visualized, whereas the posterior body, splenium, and rostrum are absent.
Spectrum of abnormalities
ACC may be complete, partial, or atypical. With complete agenesis, the corpus callosum is totally absent. With partial agenesis (hypoplasia), the anterior portion (posterior genu and anterior body) is formed, but the posterior portion (posterior body and splenium) is not. The rostrum and the anterior/inferior genu are also not formed. An atypical appearance occurs when the anterior to posterior formation is not respected.
In holoprosencephaly, callosal anomalies are atypical; for example, the splenium may be present without a genu or body. In middle interhemispheric fusion, which is a variety of holoprosencephaly, the genu and splenium may be present without the callosal body. [7]
With pseudo–corpus callosum, which involves conditions of complete or partial agenesis, the hippocampal commissure may become enlarged and appear like the posterior part of the corpus callosum.
Secondary destruction of the corpus callosum occurs when the genu and anterior body are destroyed, leaving the posterior portion of the corpus callosum intact. This may occur secondary to porencephaly or schizencephaly, as a surgical complication in cases involving the transcallosal approach to the lateral and third ventricle, or with hemisection of the callosum for the treatment of seizures.
ACC is often complicated by other intracranial and extracranial findings that significantly affect the postnatal prognosis. Studies have shown that associated anomalies as more frequent, with a finding of isolated ACC ranging from 10 to 27%. [8, 9, 10] Other cerebral malformations found to coexist with callosal dysgenesis include interhemispheric cysts; intracranial lipomas; and disorders of neuronal migration, such as neuronal heterotopias, lissencephaly, pachygyria, and, as mentioned, schizencephaly.
Imaging modalities
The diagnosis of callosal agenesis depends on neuroimaging. In the newborn, before closure of the anterior fontanelle occurs, screening ultrasonography (US) may clearly show the absence of the corpus callosum; it may also show parallel lateral ventricles, interhemispheric cysts, hydrocephalus, and other related anomalies. US was the first imaging modality to allow direct sagittal imaging of callosal dysgenesis. [11, 12, 13, 14, 15, 16]
Antenatal diagnosis of ACC is possible from about 20 weeks' gestation. Characteristic intrauterine US findings include colpocephaly and parallel ventricular walls. Computed tomography (CT) scan findings are also diagnostic of ACC. Parallel lateral ventricles, colpocephaly, and extension of the third ventricle into the interhemispheric fissure are particularly pertinent findings. In patients with ACC who have an interhemispheric cyst, the preoperative injection of nonionic water-soluble contrast material into the cystic loculations for CT evaluation enables assessment of the ventricular system or of the communication of the cystic components with one another.
Magnetic resonance imaging (MRI) is currently the imaging procedure of choice in infants and children with ACC, even in patients who have previously undergone CT and US examinations. [17, 18, 19, 20] The multiplanar capability and high soft-tissue contrast that are possible with MRI permit confident diagnosis of ACC and its associated anomalies, especially neuronal migration anomalies or atypical forms of holoprosencephaly. These entities may be extremely subtle or indiscernible on CT or US images. [21]
Computed Tomography
Axial CT scanning shows parallel ventricles and continuation of the interhemispheric fissure with the third ventricle in patients with agenesis of the corpus callosum (ACC). Colpocephaly (shown in the image below) may easily be visualized.
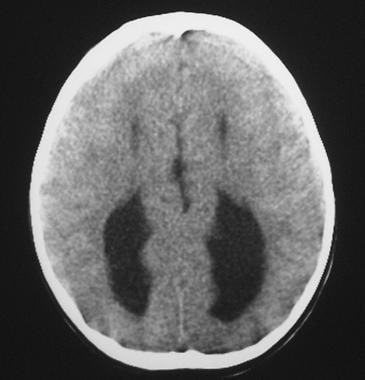 Corpus callosum, agenesis. Axial nonenhanced CT of the brain shows colpocephaly, caused by dilation of the atria, and occipital horns of the lateral ventricle. Note the parallel configuration of the lateral ventricles. Interdigitation of gyri from fenestration of the falx may be noted incidentally.
Corpus callosum, agenesis. Axial nonenhanced CT of the brain shows colpocephaly, caused by dilation of the atria, and occipital horns of the lateral ventricle. Note the parallel configuration of the lateral ventricles. Interdigitation of gyri from fenestration of the falx may be noted incidentally.
Nonenhanced axial CT may show an interhemispheric cyst. In complex types of multilocular interhemispheric cysts associated with callosal agenesis, a CT cystogram or ventriculogram may be obtained after iohexol is introduced into the cyst to establish which of the CSF collections communicate with each other or with the ventricular system.
Although CT findings may suggest the diagnosis of agenesis of the corpus callosum, MRI and US show the anatomic features of ACC better than CT does. MRI is the preferred imaging modality, especially for the diagnosis of partial agenesis and for the depiction of associated anomalies.
Magnetic Resonance Imaging
The MRI findings in agenesis of the corpus callosum (ACC) are clearly demonstrated on the sagittal projection. Sagittal T1-weighted images (examples of which appear below) clearly show the exact extent of callosal dysgenesis. [19, 20] Fetal MRI is increasingly being used for prenatal diagnosis of ACC. Shwe et al found that in 43 of 59 (73%) cases with postnatal neuroimaging for ACC, the prenatal ACC subcategory (isolated-complete, isolated-partial, complex-complete, complex-partial) on fetal MRI was confirmed. [22]
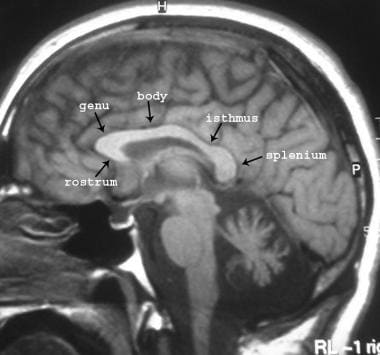 Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows the normal appearance of the corpus callosum.
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows the normal appearance of the corpus callosum.
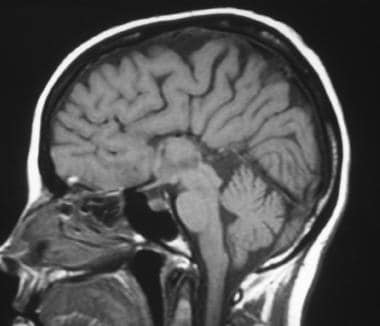 Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows complete absence of the corpus callosum. The cingulate sulcus is absent, and the medial hemispheric sulci reach the third ventricle in a radial fashion.
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows complete absence of the corpus callosum. The cingulate sulcus is absent, and the medial hemispheric sulci reach the third ventricle in a radial fashion.
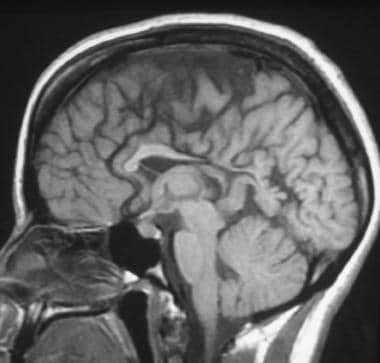 Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows partial agenesis of the corpus callosum. The genu and anterior body of the corpus callosum are visualized, whereas the posterior body, splenium, and rostrum are absent.
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows partial agenesis of the corpus callosum. The genu and anterior body of the corpus callosum are visualized, whereas the posterior body, splenium, and rostrum are absent.
In complete agenesis, the corpus callosum is not visualized, whereas in a hypogenetic corpus callosum, the later-forming structures are usually absent. Therefore, the corpus callosum may show a posterior genu; a posterior genu and anterior body; a genu and an entire body; or an entire genu, body, and splenium with the exception of the rostrum. The third ventricle may be high riding and interposed between the bodies of the lateral ventricles. [23, 24, 25] (See the images below.)
 Corpus callosum, agenesis. Axial T1-weighted MRI shows that the lateral ventricles are parallel to each other and do not come into contact with each other as they normally should.
Corpus callosum, agenesis. Axial T1-weighted MRI shows that the lateral ventricles are parallel to each other and do not come into contact with each other as they normally should.
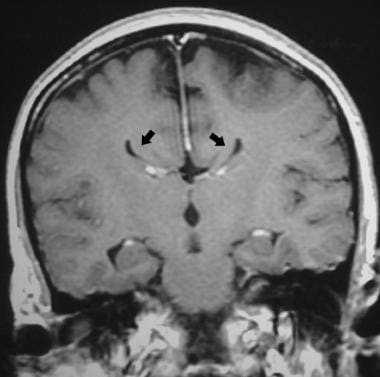 Corpus callosum, agenesis. Coronal T1-weighted MRI of the brain shows absence of the normal corpus callosum. The lateral ventricles form a bull's-horn appearance and are indented medially by the Probst bundle (arrows).
Corpus callosum, agenesis. Coronal T1-weighted MRI of the brain shows absence of the normal corpus callosum. The lateral ventricles form a bull's-horn appearance and are indented medially by the Probst bundle (arrows).
 Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain. Parasagittal section through the lateral ventricle shows dilatation of the atrium and occipital horn (colpocephaly).
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain. Parasagittal section through the lateral ventricle shows dilatation of the atrium and occipital horn (colpocephaly).
 Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows apparent atypical callosal dysgenesis in lobar holoprosencephaly. The body and splenium of the corpus callosum are well formed, whereas the genu and rostrum are hypoplastic.
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows apparent atypical callosal dysgenesis in lobar holoprosencephaly. The body and splenium of the corpus callosum are well formed, whereas the genu and rostrum are hypoplastic.
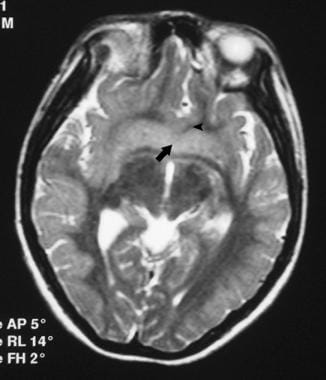 Corpus callosum, agenesis. Axial T2-weighted MRI of the brain shows apparent atypical callosal dysgenesis in lobar holoprosencephaly (same patient as in the previous image). There is fusion across the midline of the inferior basal ganglia (arrow) and the medial cortex of the frontal lobes across the interhemispheric fissure (arrowhead).
Corpus callosum, agenesis. Axial T2-weighted MRI of the brain shows apparent atypical callosal dysgenesis in lobar holoprosencephaly (same patient as in the previous image). There is fusion across the midline of the inferior basal ganglia (arrow) and the medial cortex of the frontal lobes across the interhemispheric fissure (arrowhead).
Loss of the supporting function of the corpus callosum results in upward bulging of the roof of the third ventricle into the interhemispheric fissure. This upward herniation of the distended third ventricle is generally referred to as the interhemispheric cyst, but it should not be confused with a true dorsal or arachnoid cyst of the interhemispheric fissure found in some cases of callosal agenesis.
The herniated third ventricle or true cyst may be located in the midline, separating the cerebral hemispheres, or it may be located predominantly to one side of the falx or the other. The herniated third ventricle is of variable size, sometimes extending superiorly all the way to the inner table of the calvaria.
An arachnoid or dorsal cyst generally does not communicate with the third or lateral ventricles, and it may be multiseptated. Hemorrhage may occur within the cysts, markedly changing their signal intensity on MRIs.
Coronal and axial MRI sections are best for demonstrating the longitudinal callosal bundles of Probst. They represent nondecussated callosal fibers. Instead of crossing in the midline, these fibers deviate at the interhemispheric fissure to run along the medial borders of the lateral ventricles from the frontal paraolfactory cortex to the occipital region. Their volume is less than that of the fibers in the normal corpus callosum; they are of different sizes.
The anterior commissure is usually present; occasionally, it is larger or smaller than normal. It is best seen on sagittal or axial T1-weighted images. The hippocampal commissure is usually absent or hypoplastic but sometimes may be enlarged.
The lateral ventricles may have a colpocephalic appearance with a localized dilatation of the atria and occipital horns. The lateral ventricles are pressed upon superomedially by the adjacent bundles, which are more marked in the frontal regions, where the bundles are thickest. They also appear widely separated and are medially concave, with the upper corners turned up and pointed. This finding is called bull's horns or the bat-wing conformation.
The foramen of Monro may be enlarged. The cingulate gyri are not rotated, and the cingulate sulcus is absent; this results in a radial pattern of sulci in the medial surface of the cerebral hemisphere. This finding is helpful in evaluating newborns, in whom the corpus callosum is normally thin.
Often, keyhole dilatation of the temporal horns occurs secondary to incomplete inversion of the hippocampal formation. This finding indicates the intimate relationship between the development of the corpus callosum and the limbic system.
A large percentage of patients with dysgenesis of the corpus callosum have a large interhemispheric cyst, which may or may not communicate with the ventricular system. The cyst is frequently associated with hydrocephalus. The exact origin of the cyst is not known. Some suggest that it is a dilated third ventricle or a true arachnoid cyst. At autopsy, the lining of the cyst may contain ependymal or arachnoid cells. On MRIs, the cyst may have a high protein content; in these cases, the signal intensity on T1-weighted images is greater than that of CSF.
A pericallosal lipoma of the corpus callosum appears as a high–signal-intensity mass on T1-weighted images, usually dorsal to the corpus callosum; it may be associated with callosal dysgenesis.
Degree of confidence
With the exception of US in the sagittal projection, MRI is best for directly visualizing the anatomy of the corpus callosum. The neuropathologic abnormalities intrinsic to callosal dysgenesis, as well as the associated brain anomalies, are portrayed in exquisite detail on sagittal, axial, and coronal MRIs. Only MRI is reliable for detecting subtle partial callosal dysgenesis.
A meta-analysis of 798 fetuses reported that in infants with complete ACC, 10.9% additional anomalies were identified by fetal MRI; in patients with partial ACC, 13.4% additional anomalies were detected. Cortical and posterior fossa anomalies were the most common anomalies found by MRI for both complete and partial ACC. [26]
In a retrospective study, by the European Neurosonography (ENSO) Working Group, of 269 fetuses with a prenatal diagnosis of isolated corpus callosum anomalies detected on ultrasonography, additional structural anomalies of the CNS were detected on prenatal MRI in 11.2% (30/269) of cases. [27]
In a study by Santirocco et al of 46 cases of corpus callosum anomalies diagnosed by prenatal ultrasound, third-trimester MRI confirmed all 46 diagnoses, and in 7 cases (15.2%), MRI identified additional intracranial findings, with 3 cases being reclassified as a result of the MRI findings. [28]
As an adjunctive modality, diffusion tensor imaging (DTI) can provide more detailed information that cannot be obtained by conventional MRI regarding the visualization and connectivity of white-matter structures and anomalies, which can be helpful in the syndromic- and etiologic-based diagnosis. [29]
False positives/negatives
The differential diagnosis of agenesis is very limited because of the characteristic imaging appearance. In certain cases of hydrocephalus in infants, it may sometimes be difficult to visualize a corpus callosum that is very thin. However, with careful observation of sagittal MRI images, the radial convergence of sulci that is seen with ACC is not seen, and a thin corpus may usually be identified. The midline interhemispheric cysts may be confused with midline arachnoid cysts (suprasellar, collicular) or with prominent cavum septum pellucidum and cavum vergae.
Ultrasonography
Antenatal diagnosis of agenesis of the corpus callosum (ACC) is possible from about 20 weeks' gestation. Endovaginal US may contribute to the antenatal diagnosis of ACC. Findings that suggest ACC in utero are a disproportionate enlargement of the occipital horns and an abnormally parallel course of the ventricular walls. The abnormal radiating pattern may not be evident until late in the third trimester. [20, 30, 31, 32]
In coronal sonograms, ACC findings include the following:
-
Enlarged atria and occipital horns
-
Parallel and widely separated bodies of lateral ventricles
-
An enlarged and upwardly displaced third ventricle
-
Absent corpus callosum and septum pellucidum
-
Frontal horns that are sharply angulated laterally and are indented medially by the Probst bundles
-
Medial cerebral gyri and sulci, with a radial pattern extending to the roof of the elevated third ventricle
-
Elongation of the interventricular foramen of Monro
An associated midline interhemispheric cystic lesion, a separate arachnoid cyst, or a communicating porencephalic cyst may be seen with US. Lipoma of the corpus callosum is demonstrated as a highly echogenic mass in the region of the corpus callosum.
US, especially transvaginal US, helps in the prenatal diagnosis of nonchromosomal syndromes by enabling the detection of specific morphologic findings. In rare syndromes, the index case may not be diagnosed prenatally, but with subsequent pregnancies, early diagnosis is beneficial. However, MRI has been found to be more helpful than US in the prenatal diagnosis of corpus callosal dysgenesis. [33, 34]
-
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows the normal appearance of the corpus callosum.
-
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows complete absence of the corpus callosum. The cingulate sulcus is absent, and the medial hemispheric sulci reach the third ventricle in a radial fashion.
-
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows partial agenesis of the corpus callosum. The genu and anterior body of the corpus callosum are visualized, whereas the posterior body, splenium, and rostrum are absent.
-
Corpus callosum, agenesis. Axial nonenhanced CT of the brain shows colpocephaly, caused by dilation of the atria, and occipital horns of the lateral ventricle. Note the parallel configuration of the lateral ventricles. Interdigitation of gyri from fenestration of the falx may be noted incidentally.
-
Corpus callosum, agenesis. Axial T1-weighted MRI shows that the lateral ventricles are parallel to each other and do not come into contact with each other as they normally should.
-
Corpus callosum, agenesis. Coronal T1-weighted MRI of the brain shows absence of the normal corpus callosum. The lateral ventricles form a bull's-horn appearance and are indented medially by the Probst bundle (arrows).
-
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain. Parasagittal section through the lateral ventricle shows dilatation of the atrium and occipital horn (colpocephaly).
-
Corpus callosum, agenesis. Sagittal T1-weighted MRI of the brain shows apparent atypical callosal dysgenesis in lobar holoprosencephaly. The body and splenium of the corpus callosum are well formed, whereas the genu and rostrum are hypoplastic.
-
Corpus callosum, agenesis. Axial T2-weighted MRI of the brain shows apparent atypical callosal dysgenesis in lobar holoprosencephaly (same patient as in the previous image). There is fusion across the midline of the inferior basal ganglia (arrow) and the medial cortex of the frontal lobes across the interhemispheric fissure (arrowhead).









