Practice Essentials
Carpal tunnel syndrome (CTS) is the most common peripheral compressive neuropathy, accounting for 90% of all compressive neuropathies. [1] It is defined as the impairment of motor and/or sensory function of the median nerve as it traverses through the carpal tunnel. (See the images below.) It is caused either by intrinsic swelling of the median nerve or by extrinsic compression of the median nerve by one of the many surrounding structures of the wrist.
 Carpal tunnel syndrome. Carpal and Guyon tunnels. Drawing showing the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor retinaculum (medium gray region) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. The palmar carpal ligament (dark gray region) forms the volar boundary of the Guyon tunnel. * = flexor pollicis longus tendon, * = flexor carpi radialis tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
Carpal tunnel syndrome. Carpal and Guyon tunnels. Drawing showing the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor retinaculum (medium gray region) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. The palmar carpal ligament (dark gray region) forms the volar boundary of the Guyon tunnel. * = flexor pollicis longus tendon, * = flexor carpi radialis tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
 Carpal tunnel syndrome. Carpal and Guyon tunnels. Drawing showing the distal level of the carpal tunnel delimited by the hook of the hamate (H) and the tubercle of the trapezium (T). The flexor retinaculum (medium gray region) forms the roof of the carpal tunnel. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
Carpal tunnel syndrome. Carpal and Guyon tunnels. Drawing showing the distal level of the carpal tunnel delimited by the hook of the hamate (H) and the tubercle of the trapezium (T). The flexor retinaculum (medium gray region) forms the roof of the carpal tunnel. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
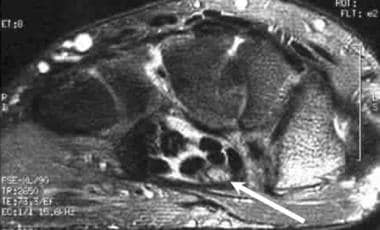
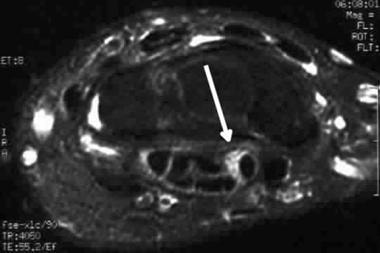 Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with fat saturation. Note the increased T2-weighted signal within the median nerve (arrow). A slightly increased cross sectional area of the nerve is noted but the nerve architecture is preserved, consistent with early or mild inflammation.
Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with fat saturation. Note the increased T2-weighted signal within the median nerve (arrow). A slightly increased cross sectional area of the nerve is noted but the nerve architecture is preserved, consistent with early or mild inflammation.
CTS symptoms can be ameliorated through conservative and surgical strategies. The exact CTS pathophysiology must be identified. Genetic predispositions to CTS are augmented by various variants within genes; however, CTS etiology could include risk factors such as wrist movements, injury, and specific conditions (eg, age, body mass index [BMI], sex, cardiovascular conditions). The high prevalence of CTS diminishes the quality of life of its sufferers and imposes costs on health systems—hence the significance of research and clinical trials to elucidate CTS pathogenesis and to develop novel therapeutic targets. [2]
Preferred examination
Although CTS is a well-recognized condition, new insights into its epidemiology, diagnosis, and treatment have emerged. The availability of disease-modifying treatments for rare systemic disorders associated with CTS (eg, amyloidosis) should alert clinicians to these diagnostic possibilities.
Besides clinical evaluation and electrophysiology, the role of ultrasonography (US) as a diagnostic tool has been confirmed, and newer US techniques have been applied; their clinical utility and feasibility require further investigation. Surgical and nonsurgical interventions are beneficial for the treatment of CTS, and several treatment options are now available, giving clinicians the possibility of choosing the best approach for every patient. New diagnostic and therapeutic techniques require further validation. [3]
CTS is seen in 5% of the population and in 14-30% of diabetic individuals. Although electrophysiologic tests are used as the gold standard method for diagnosis, alternative methods are being explored. Sertbas et al in 2023 aimed to investigate whether measurement of median nerve cross-sectional area (CSA) by US is associated with the presence and severity of CTS. Investigators in this prospective cross-sectional observational study concluded that CSA measurement with US can be used as an effective method in diagnosing severe CTS disease. [4]
Electrodiagnostic tests such as electromyography (EMG) and nerve conduction studies are 85-90% accurate in patients with CTS, with a false-negative rate of 10-25%, especially for early CTS; results may be normal in as many as one third of patients with mild CTS. [5] Therefore, in cases of clinically symptomatic CTS with normal EMG and conduction findings, radiologic studies can play a strong complementary role in diagnosis. [6, 7]
Of the available imaging methods, magnetic resonance imaging (MRI) has consistently shown the greatest sensitivity and specificity in the diagnosis and evaluation of CTS. [8]
Advances in US have improved its image quality as well as its affordability, leading to increased adoption of US evaluation of CTS. [1] US can be useful in the evaluation of soft tissues of the carpal tunnel and the median nerve. An increasing number of studies have supported early suggestions that measurement of the CSA and morphology of the median nerve with high-resolution US compares favorably with physical examination alone. Additionally, US may prove to be a beneficial adjunct in the conservative treatment of CTS. [6, 9, 10, 11, 12]
Plain radiography has no role in the evaluation of CTS apart from its ability to show the anatomic relationship of the carpal bones and detect evidence of severe prior trauma or fractures. Helical computed tomography (CT) is more sensitive than plain radiography in revealing subtle bony trauma and misalignments and can be used to measure the CSA of the carpal tunnel.
Limitations of techniques
Plain radiographs usually do not reveal ligamentous or soft-tissue abnormalities but may be useful to exclude frank fractures or chronic degenerative or posttraumatic morphologic abnormalities.
CT does not reveal ligamentous or soft-tissue abnormalities to any degree. Axial scanners are even more limited, in that they do not allow adequate multiplanar or three-dimensional (3D) reconstructions.
US is operator- and equipment-dependent. Although musculoskeletal US using high-frequency transducers is widely employed in Europe, familiarity with and training in the performance and interpretation of carpal tunnel US remain variable in European countries, and even more so in the United States.
High-frequency gray-scale US can clearly show the median nerve and surrounding structures, which provides valuable information for clinical treatment. Generally, an increased nerve CSA is the main objective criterion for diagnosis of CTS on US. However, the cutoff value for CSA varies among published reports from 8.5 to 15 mm2, and the uncertainty of the diagnosis criterion affects its value. In addition, sensitivity is low for diagnosis using CSA alone. [13]
MRI is useful for the evaluation of all of the intrinsic structures of the wrist (including the carpal bones) but may not be widely available, is technique- and equipment-dependent, can require up to 45 minutes to complete an examination, and has a number of contraindications (eg, cardiac pacemakers, older aneurysm clips, new stents or aortic valves, ferromagnetic ocular fragments).
Differential diagnosis
A number of clinical processes can create symptoms similar to those of CTS, originating more proximally in the neural pathway of the median nerve. These include multiple sclerosis, cervical radiculopathy, Pancoast tumor, brachial plexitis or brachial plexopathy, pronator syndrome, ulnar or radial neuropathy, generalized neuropathy, and median nerve contusion.
Although the appearance of CTS is fairly distinctive on MRI, differential possibilities include contusion and lipofibromatous hamartoma of the median nerve. A clinical history of recent trauma or a longstanding mass often allows the exclusion or inclusion of these etiologies in the differential.
Radiography
Plain radiographs are useful for evaluating the wrist and carpal bones for trauma and fractures (especially the hook of the hamate and the tubercle of the trapezium), severe osteoarthritis, and other arthropathies. Plain films are of limited use in diagnosing or evaluating CTS. They do not effectively visualize the small soft-tissue structures of the carpal tunnel, many of which can be involved in the syndrome. A carpal tunnel view of the wrist on plain films provides only a very rough idea of the CSA of the carpal tunnel.
Computed Tomography
CT is useful for its ability to display and evaluate the cross-sectional volume of the carpal tunnel and for detecting subtle calcification in the tendons within the canal. CT also provides an excellent tool for evaluating the carpal bones through multiplanar and 3D reconstructions.
CT is limited in its ability to visualize the median nerve and tendons of the carpal tunnel well enough to allow a definitive differential diagnosis to be rendered. Therefore, other methods of visualizing the soft tissues of the carpal tunnel are preferable.
Magnetic Resonance Imaging
In patients with flexor tenosynovitis, axial MRI demonstrates bowing of the flexor retinaculum. Inflamed synovium and tendon sheaths demonstrate low signal intensity on T1-weighted images and increased signal intensity on T2-weighted, T2*-weighted, and short tau inversion recovery (STIR) sequences. [14] (See the images below.)
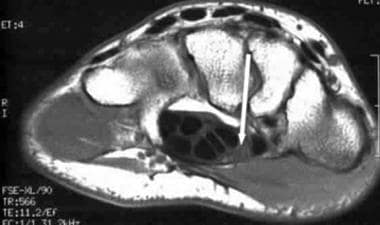 Carpal tunnel syndrome. Normal findings on an axial spin-echo T1 MRI of the carpal tunnel showing the intermediate signal intensity of the median nerve (arrow).
Carpal tunnel syndrome. Normal findings on an axial spin-echo T1 MRI of the carpal tunnel showing the intermediate signal intensity of the median nerve (arrow).
 Carpal tunnel syndrome. Normal findings of isointense to hypointense appearance of the median nerve on fast spin-echo T2-weighted MRI (arrow). Note the fairly well-defined nerve fascicles within the median nerve sheath.
Carpal tunnel syndrome. Normal findings of isointense to hypointense appearance of the median nerve on fast spin-echo T2-weighted MRI (arrow). Note the fairly well-defined nerve fascicles within the median nerve sheath.
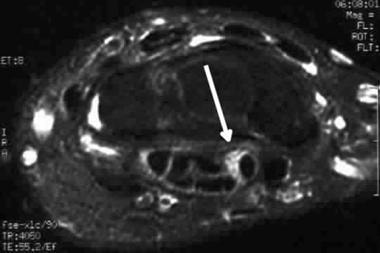 Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with fat saturation. Note the increased T2-weighted signal within the median nerve (arrow). A slightly increased cross sectional area of the nerve is noted but the nerve architecture is preserved, consistent with early or mild inflammation.
Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with fat saturation. Note the increased T2-weighted signal within the median nerve (arrow). A slightly increased cross sectional area of the nerve is noted but the nerve architecture is preserved, consistent with early or mild inflammation.
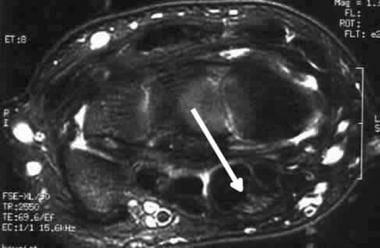
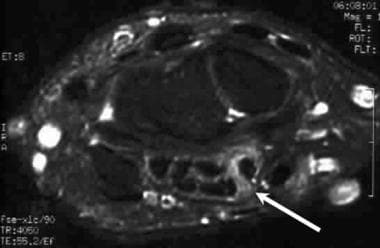
 Carpal tunnel syndrome. Fast spin-echo T2-weighted MRI illustrates more pronounced increased signal within the median nerve (arrow). Note the small amount of fluid within the carpal tunnel, a secondary sign of inflammation. Slightly less optimal fat saturation is noted than on other images, which is a common occurrence.
Carpal tunnel syndrome. Fast spin-echo T2-weighted MRI illustrates more pronounced increased signal within the median nerve (arrow). Note the small amount of fluid within the carpal tunnel, a secondary sign of inflammation. Slightly less optimal fat saturation is noted than on other images, which is a common occurrence.
 Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with greater increase in signal and loss of definition within the nerve (arrow). Inflammatory change is noted within the carpal tunnel, adjacent to the flexor digitorum superficialis tendons. The appearance is consistent with pronounced inflammatory change within the carpal tunnel.
Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with greater increase in signal and loss of definition within the nerve (arrow). Inflammatory change is noted within the carpal tunnel, adjacent to the flexor digitorum superficialis tendons. The appearance is consistent with pronounced inflammatory change within the carpal tunnel.
Regardless of the etiology of CTS, changes in the median nerve are similar. Diffuse swelling or segmental enlargement of the median nerve may be demonstrated (usually seen best at the level of the pisiform).
The median nerve may flatten (usually demonstrated best at the level of the hamate), and palmar bowing of the flexor retinaculum may be noted (usually demonstrated best at the level of the hamate).
Increased T2-weighted signal intensity within the median nerve occurs, which is demonstrated best on axial fast spin-echo (FSE) T2-weighted images. If FSE signal sequences are not available, axial gradient-recalled echo (GRE) or inversion recovery (IR) sequences also are sensitive to the increased edema in the median nerve that accompanies carpal tunnel syndrome.
MRI also is useful in detecting and characterizing space-occupying lesions, such as neuromas, ganglion cysts, lipomas, and hemangiomas. Enlargement or swelling of the median nerve proximal to the carpal tunnel, termed a pseudoneuroma, has been documented by means of MRI.
Flow-sensitive sequences or dynamic contrast-enhanced MRI can detect a circulatory disturbance causing CTS, which is a cause separate from deformation or compression of the median nerve.
One of two abnormal patterns of median nerve enhancement is usually demonstrated: (1) marked enhancement of the nerve (attributed to hypervascular edema) or (2) noticeable lack of enhancement (attributed to nerve ischemia).
As with the symptoms of CTS, MRI findings in the syndrome may vary with wrist position: flexion or extension of the wrist during the scan can alter the visualization of the median nerve from marked enhancement to complete lack of enhancement, presumably because of mechanical obstruction of blood flow to the nerve. These actions are associated with exacerbation of clinical symptoms.
Attempted surgical therapy for CTS may result in incomplete release of the flexor retinaculum. This can be detected by a residual increase in T2 signal of the median nerve within the carpal tunnel and by direct visualization of the still-connected fibers of the retinaculum.
Transverse carpal ligament release from the hook of the hamate can cause the contents of the carpal canal and/or the flexor tendons to demonstrate a volar convexity caused by the loss of the normal roof support of the flexor retinaculum.
In addition to incomplete release of the flexor retinaculum, postoperative MRI changes in failed carpal tunnel surgery include excessive fat within the carpal tunnel, neuromas, scarring, and persistent neuritis. A normal postoperative finding is widening of the fat stripe posterior to the flexor digitorum profundus tendons.
MRI studies following carpal tunnel release may demonstrate an increase in carpal tunnel volume of up to 24%, often accompanied by a change in shape from oval to circular, resulting in increased anteroposterior and mediolateral diameters.
Magnetic resonance diffusion tensor imaging (DTI) can detect microstructural changes in peripheral nerves. Studies have reported that the median nerve apparent diffusion coefficient (ADC), a quantification of water molecule diffusion direction, is sensitive in diagnosing CTS. Median nerve ADC is decreased in individuals with CTS as compared with healthy individuals at the levels of the hamate and the pisiform. ADC cutoffs to diagnose CTS should be established according to these anatomic levels; this approach can be improved through additional studies that include use of a wrist coil. [15]
Degree of confidence
Early detection of the subtle changes of CTS requires soft-tissue discrimination that is not achievable with standard radiography or CT. The ability to evaluate the cross-sectional morphologic and signal characteristics of the medial nerve and adjacent structures makes MRI invaluable in characterizing normal anatomy and abnormal pathology in the carpal tunnel.
Significant differences often are present in patients with CTS, despite the subjective flattening of the median nerve at the lateral and distal carpal row. Flattening ratios have been used to document statistically significant flattening of the median nerve at the level of the hamate. The median nerve may display enlargement or dilation at the level of the pisiform and concomitant compression and flattening at the level of the hook of the hamate.
Because carpal tunnel involvement is bilateral in as many as 50% of patients, comparison with the contralateral wrist can be misleading. Alterations in the median nerve signal intensity may represent edema or demyelination within neural fibers and thus are somewhat nonspecific. T1 and T2 signal intensities may be decreased when fibrosis of the median nerve is present. Evaluation of swelling is accomplished by comparing the CSA of the median nerve at the level of the pisiform and hamate to the CSA of the median nerve at the level of the distal radius.
Ultrasonography
The development of high-resolution (7-15 MHz) ultrasound transducers has allowed evaluation of normal and abnormal appearances of the median nerve and adjacent tendons on US. High-resolution US allows noninvasive imaging of the carpal tunnel and its contents. It has several advantages over MRI, including being relatively fast and inexpensive and allowing additional dynamic and blood flow imaging with relatively little additional time. [10] US may also be useful for evaluating rare structural causes of CTS, such as cysts, lumbrical incursion, and other space‐occupying masses. [1]
On transverse US scans, the normal median nerve is elliptical and flattens progressively as it courses distally. Median nerve compression is signaled on US by the classic triad of nerve flattening in the distal tunnel, nerve swelling at the level of the distal radius (less frequently in the proximal tunnel), and palmar bowing of the flexor retinaculum. (See the images below.)
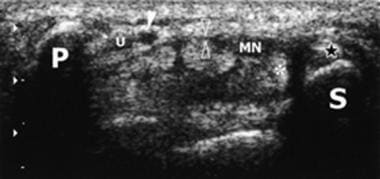 Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasonogram shows the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. At the level of the pisiform, the ulnar nerve (U) courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. * = flexor pollicis longus tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasonogram shows the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. At the level of the pisiform, the ulnar nerve (U) courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. * = flexor pollicis longus tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
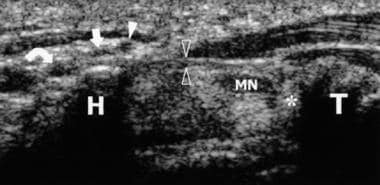 Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasonogram shows the distal level of the carpal tunnel, delimited by the hook of the hamate (H) and the tubercle of the trapezium (T). The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel. The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. At the level of the pisiform, the ulnar nerve courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. At the level of the hamate, the ulnar nerve divides into two terminal branches, a deep motor branch (curved arrow) and a superficial sensory branch (straight arrow). From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. * = flexor pollicis longus tendon. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasonogram shows the distal level of the carpal tunnel, delimited by the hook of the hamate (H) and the tubercle of the trapezium (T). The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel. The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. At the level of the pisiform, the ulnar nerve courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. At the level of the hamate, the ulnar nerve divides into two terminal branches, a deep motor branch (curved arrow) and a superficial sensory branch (straight arrow). From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. * = flexor pollicis longus tendon. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
Because the shape of the nerve varies as it passes through the tunnel, indexes have been introduced to better quantify abnormal findings; a nerve CSA greater than 9 mm2 at the level of the proximal tunnel is reported to be the best criterion for the diagnosis.
CTS, the most common peripheral entrapment neuropathy, is caused by compression of the median nerve at the level of the transverse carpal ligament of the volar wrist. Radiomics is an advanced semiautomated image analysis method that can be used to identify characteristics of the median nerve that can reveal CTS with considerable reproducibility. [16]
Radiomics can identify image information that the human eye cannot recognize. A 2023 retrospective study was undertaken to explore the value of ultrasound image–based radiomics in the diagnosis of mild CTS. Researchers concluded that the radiomics label based on ultrasound images had excellent diagnostic efficacy for mild CTS. This option is expected to help radiologists identify early CTS patients as soon as possible; it may be especially helpful for inexperienced doctors. [17]
In 2023, Chen and Fowler compared electrodiagnostic testing (EDX) with US for diagnosis of CTS. [18] Scientific consensus long has preferred nerve conduction studies; however, studies in 2023 proposed a diagnostic niche for US examination. This study assessed the relative diagnostic accuracy, sensitivity, and specificity of these two diagnostic tools.
The investigators found that EDX was more sensitive for CTS than US was [18] ; however, US aligned more closely with scores on Carpal Tunnel Syndrome 6 (CTS-6, a validated clinical CTS scoring system) and resulted in greater specificity and positive predictive value. [18] Their findings suggested that US holds a nontrivial niche in CTS diagnosis and that EDX is not clearly preferable for all CTS diagnoses and cases.
US-guided needle release and miniopen surgery are both effective measures in treating patients with CTS. US-guided needle release plus corticosteroid injection yields a smaller incision, reduces cost, requires less time for treatment, and leads to faster recovery as compared with miniopen surgery. Studies have found that US-guided needle release plus corticosteroid injection is better for clinical application. [19]
A 2023 retrospective study examined the feasibility of artificial intelligence (AI)-assisted quantitative muscle US in CTS. [20] Researchers found a significant increase in diagnostic accuracy when AI was used for quantitative analysis of muscle US. They concluded that if an analysis protocol using machine learning can be established and mounted on an ultrasound machine, then a noninvasive and non–time-consuming muscle ultrasound examination can be conducted as an ancillary tool for diagnosis.
Degree of confidence
A good correlation has been demonstrated between the measured area of the median nerve on US and the degree of findings of EMG or functional outcome after surgery. [1] Reduced transverse sliding of the nerve beneath the retinaculum during flexion and extension of the index finger also may be seen, but this sign is harder to quantify and may be too subjective.
Only a few studies have compared US with MRI in evaluating CTS, but these have demonstrated that US is capable of yielding results similar to those of MRI. MRI has been shown to be superior to US in the identification of subtle cases, and MRI demonstrates better sensitivity than color and power Doppler US in showing changes caused by nerve edema and blood perfusion abnormalities.
High-resolution US provides an objective assessment of surgical outcomes in cases of severe CTS, demonstrating normalization of the wrist-to-forearm ratio in a series of successful cases. Future studies of poor outcomes may reveal whether improvements in wrist-to-forearm ratio and in CSA can provide reassurance and support for observation rather than reoperation. US also allows anatomic evaluation and may be helpful in cases with medicolegal or psychosocial issues; it is potentially less costly and may be better tolerated by patients than EDX or MRI. [21]
-
Carpal tunnel syndrome. Carpal and Guyon tunnels. Drawing showing the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor retinaculum (medium gray region) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. The palmar carpal ligament (dark gray region) forms the volar boundary of the Guyon tunnel. * = flexor pollicis longus tendon, * = flexor carpi radialis tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
-
Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasonogram shows the proximal level of the carpal tunnel delimited by the pisiform (P) and the scaphoid (S). The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel and the floor of the Guyon tunnel. At the level of the pisiform, the ulnar nerve (U) courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. * = flexor pollicis longus tendon. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
-
Carpal tunnel syndrome. Carpal and Guyon tunnels. Drawing showing the distal level of the carpal tunnel delimited by the hook of the hamate (H) and the tubercle of the trapezium (T). The flexor retinaculum (medium gray region) forms the roof of the carpal tunnel. From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
-
Carpal tunnel syndrome. Carpal and Guyon tunnels. Transverse 5-12-MHz ultrasonogram shows the distal level of the carpal tunnel, delimited by the hook of the hamate (H) and the tubercle of the trapezium (T). The flexor retinaculum (open arrowheads) forms the roof of the carpal tunnel. The flexor tendons and median nerve (MN) extend through the carpal tunnel, with the nerve lying palmar and radial. At the level of the pisiform, the ulnar nerve courses medial to the ulnar artery (solid arrowhead) within the Guyon tunnel. At the level of the hamate, the ulnar nerve divides into two terminal branches, a deep motor branch (curved arrow) and a superficial sensory branch (straight arrow). From Martinoli C, Bianchi S, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. * = flexor pollicis longus tendon. Radiographics 2000; 20:S199-S217. Used by permission of the authors and RSNA.
-
Carpal tunnel syndrome. Normal findings on an axial spin-echo T1 MRI of the carpal tunnel showing the intermediate signal intensity of the median nerve (arrow).
-
Carpal tunnel syndrome. Normal findings of isointense to hypointense appearance of the median nerve on fast spin-echo T2-weighted MRI (arrow). Note the fairly well-defined nerve fascicles within the median nerve sheath.
-
Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with fat saturation. Note the increased T2-weighted signal within the median nerve (arrow). A slightly increased cross sectional area of the nerve is noted but the nerve architecture is preserved, consistent with early or mild inflammation.
-
Carpal tunnel syndrome. Fast spin-echo T2-weighted MRI illustrates more pronounced increased signal within the median nerve (arrow). Note the small amount of fluid within the carpal tunnel, a secondary sign of inflammation. Slightly less optimal fat saturation is noted than on other images, which is a common occurrence.
-
Carpal tunnel syndrome. Axial fast spin-echo T2-weighted MRI with greater increase in signal and loss of definition within the nerve (arrow). Inflammatory change is noted within the carpal tunnel, adjacent to the flexor digitorum superficialis tendons. The appearance is consistent with pronounced inflammatory change within the carpal tunnel.




