Practice Essentials
De Quervain's tenosynovitis (or de Quervain tenosynovitis) is caused by stenosing tenosynovitis of the first dorsal compartment of the wrist. The first dorsal compartment at the wrist includes the tendons of the abductor pollicis longus (APL) and the extensor pollicis brevis (EPB). Patients with this condition usually report pain at the dorsolateral aspect of the wrist, with referral of pain toward the thumb and/or the lateral forearm. This condition responds well to nonsurgical treatment. [1, 2, 3, 4, 5, 6] See the images below.
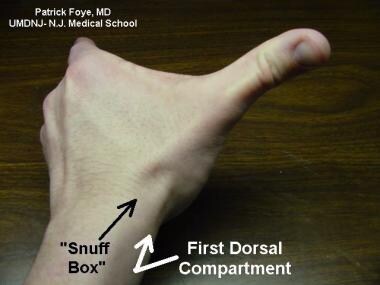 The first dorsal compartment of the wrist includes the tendon sheath that encloses the abductor pollicis longus and the extensor pollicis brevis tendons at the lateral border of the anatomic snuffbox.
The first dorsal compartment of the wrist includes the tendon sheath that encloses the abductor pollicis longus and the extensor pollicis brevis tendons at the lateral border of the anatomic snuffbox.
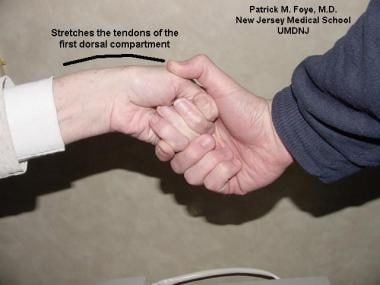 The Finkelstein test is performed by having the patient make a fist with the thumb inside the fingers. The clinician then applies ulnar deviation of the wrist to reproduce the presenting symptoms of dorsolateral wrist pain. Some authors refer to this same maneuver as Eichhoff’s test.
The Finkelstein test is performed by having the patient make a fist with the thumb inside the fingers. The clinician then applies ulnar deviation of the wrist to reproduce the presenting symptoms of dorsolateral wrist pain. Some authors refer to this same maneuver as Eichhoff’s test.
Workup in de Quervain tenosynovitis
No laboratory studies support the diagnosis of de Quervain tenosynovitis. The clinician may consider serologic testing for rheumatoid arthritis (ie, checking serum rheumatoid factor) if the patient has no history of either acute or repetitive trauma or other risk factors.
Usually, no imaging studies are required for diagnosing de Quervain tenosynovitis. If a sufficient history of acute trauma exists, radiographs of the wrist are indicated to assess for fracture.
If the radiographs are negative but there is nonetheless a suggestion of fracture or osteonecrosis, further imaging studies can be pursued (eg, 3-phase bone scan).
Management of de Quervain tenosynovitis
In the acute stage, the therapist may use cryotherapy (eg, cold packs, ice massage) to reduce inflammation and edema. Local inflammation also can be treated with topical corticosteroids (eg, hydrocortisone), which are driven into the subcutaneous tissues using ultrasound (ie, phonophoresis) or electrically charged ions (ie, iontophoresis). [7]
Low-level laser therapy (3 J/cm2 in continuous mode, frequency 7-10 sessions on alternative days) and therapeutic ultrasound (0.8-1.5 W/cm2, 1 MHz in pulsed mode) have each proven successful in the treatment of de Quervain tenosynovitis. However, both treatments have been found to be less effective than steroid injections in reducing pain and improving grip strength. [8]
An occupational therapist can perform an assessment of a patient's activities of daily living (ADL) to help determine possible precipitating factors in the development of de Quervain syndrome; he/she can then suggest activity modifications. Although off-the-shelf orthotic devices usually are adequate in the treatment of de Quervain tenosynovitis, sometimes a custom-made thumb spica can be fabricated by a trained occupational therapist. [9]
For severe, unresponsive cases of de Quervain tenosynovitis in which injections, splinting, and ergonomic modification of activities have failed, a referral for surgical treatment to decompress the first dorsal compartment is needed. [6, 10, 11]
Pathophysiology
In the first dorsal compartment of the wrist, a tendon sheath encloses the abductor pollicis longus and the extensor pollicis brevis tendons at the lateral border of the anatomical snuffbox. Inflammation at this site commonly is seen in patients who use their hands and thumbs in a repetitive fashion. Thus, de Quervain tenosynovitis can result from cumulative (repetitive) microtrauma. Inflammation also may occur after an isolated episode of acute trauma to the site. [6]
The first dorsal compartment of the wrist often contains a septum, which can complicate treatment by making target structures more difficult to inject. Up to 50% of patients may have first dorsal compartments with septa. These septa have an average length of 5 mm. [12]
Etiology
A randomized study of 300 undergraduate students showed that those who texted more mobile phone messages per day were more likely to have a positive Finkelstein test (indicative de Quervain tenosynovitis). The investigators concluded that students who use their mobile phones to send more than 50 texts per day have a higher probability of developing de Quervain tenosynovitis. [13]
A cross-sectional study by Baabdullah et al indicated that heavy smartphone use correlates with thumb/wrist pain. Using a self-administered patient-rated wrist and hand evaluation (PRWHE) questionnaire, the investigators found that smartphone “addicts” (as identified using the short version of the smartphone addiction scale) had a median total pain and disability score of 8.00, compared with 4.25 for non-addict smartphone users. However, the study did not find smartphone addiction to be significantly associated with a positive Finkelstein test. [14]
A cross-sectional study of 500 students, by Ma et al, showed that those who played mobile games frequently and for long periods of time were at higher risk of developing de Quervain tenosynovitis. The investigators recommended limiting mobile game play to less than 2.25 hours/day to limit the risk of developing the condition. [15]
A cross-sectional study by Warrender et al indicated that de Quervain tenosynovitis is less prevalent in regions with higher humidity and more prevalent in areas with higher average barometric pressure. [16]
Epidemiology
Frequency
United States
De Quervain tenosynovitis is relatively prevalent, especially among individuals who perform repetitive activities using their hands (eg, certain assembly line workers, secretaries). [17]
Mortality/Morbidity
Mortality is not associated with de Quervain tenosynovitis. Some morbidity may result as the patient experiences progressive pain, with limitations occurring in activities requiring use of the affected hand.
Race
Traditionally, no race predilection has been reported for de Quervain tenosynovitis. However, recently the University of Colorado School of Medicine has described the black race as a risk factor for de Quervain tenosynovitis. [17]
Sex
Although this condition is commonly seen in females and males, the incidence of de Quervain tenosynovitis appears to be significantly greater in women. [6] Some sources even quote a female-to-male ratio as high as 8:1. Interestingly, many women suffer from de Quervain tenosynovitis during pregnancy or the postpartum period. [18]
Age
De Quervain tenosynovitis is much more common in adults than in children.
Genetics
Genomic research has revealed that rs35360670 on chromosome 8 has a significant association with de Quervain tenosynovitis. [19]
-
The first dorsal compartment of the wrist includes the tendon sheath that encloses the abductor pollicis longus and the extensor pollicis brevis tendons at the lateral border of the anatomic snuffbox.
-
The Finkelstein test is performed by having the patient make a fist with the thumb inside the fingers. The clinician then applies ulnar deviation of the wrist to reproduce the presenting symptoms of dorsolateral wrist pain. Some authors refer to this same maneuver as Eichhoff’s test.




