Practice Essentials
Traumatic brain injury (TBI), also known as acquired brain injury, head injury, or brain injury, causes substantial disability and mortality. It occurs when a sudden trauma damages the brain and disrupts normal brain function. TBI may have profound physical, psychological, cognitive, emotional, and social effects.
Classification
Primary and secondary injuries
-
Primary injury: Induced by mechanical force and occurs at the moment of injury; the 2 main mechanisms that cause primary injury are contact (eg, an object striking the head or the brain striking the inside of the skull) and acceleration-deceleration [1]
-
Secondary injury: Not mechanically induced; it may be delayed from the moment of impact, and it may superimpose injury on a brain already affected by a mechanical injury [1]
Focal and diffuse injuries
These injuries are commonly found together; they are defined as follows:
-
Focal injury: Includes scalp injury, skull fracture, and surface contusions; generally caused by contact
-
Diffuse injury: Includes diffuse axonal injury (DAI), hypoxic-ischemic damage, meningitis, and vascular injury; usually caused by acceleration-deceleration forces
Measures of severity
See the list below:
-
Duration of loss of consciousness: Classified as mild (mental status change or loss of consciousness [LOC] < 30 min), moderate (mental status change or LOC 30 min to 6 hr), or severe (mental status change or LOC >6 hr)
-
Posttraumatic amnesia (PTA): The time elapsed from injury to the moment when patients can demonstrate continuous memory of what is happening around them [4]
Complications
Complications include the following:
-
Posttraumatic seizures: Frequently occur after moderate or severe TBI
-
Hydrocephalus
-
Deep vein thrombosis: Incidence as high as 54% [5]
-
Heterotopic ossification: Incidence of 11-76%, with a 10-20% incidence of clinically significant heterotopic ossification [6]
-
Spasticity
-
Gastrointestinal and genitourinary complications: Among the most common sequelae in patients with TBI
-
Gait abnormalities
-
Agitation: Common after TBI
-
Chronic traumatic encephalopathy (CTE)
Long-term physical, cognitive, and behavioral impairments are the factors that most commonly limit a patient's reintegration into the community and his/her return to employment. They include the following:
-
Insomnia
-
Cognitive decline
-
Posttraumatic headache: Tension-type headaches are the most common form, but exacerbations of migraine-like headaches are also frequent
Outcome measures
The following tools are commonly used to measure outcome after TBI [11, 12] :
-
Functional Independence Measure (FIM): An 18-item scale used to assess the patient's level of independence in mobility, self-care, and cognition
-
Glasgow Outcome Scale (GOS)
-
Disability Rating Scale (DRS): Measures general functional changes over the course of recovery after TBI (see the image below)
Epidemiology
Traumatic brain injury (TBI), also known as acquired brain injury, head injury, or brain injury, causes substantial disability and mortality. It occurs when a sudden trauma damages the brain and disrupts normal brain function. TBI may have profound physical, psychological, cognitive, emotional, and social effects. Mild TBI appears to be vastly underdiagnosed in the setting of systemic trauma, even in trauma centers. [13]
According to the Healthcare Cost and Utilization Project’s National (Nationwide) Inpatient Sample, about 214,110 TBI-related hospitalizations occurred in the United States in 2020, with the Centers for Disease Control and Prevention (CDC) reporting that 69,473 TBI-related deaths in occurred 2021. Males were found to have an almost two-fold risk of hospitalization for TBI compared with females, according to the 2020 statistics, and an almost three-fold risk of TBI-associated death, according to the 2021 figures. [14]
The two sources also found that the greatest number and rate of TBI-related hospitalizations and deaths were in persons aged 75 years or older, with this population making up about 32% and 28% of such hospitalizations and deaths, respectively. [14]
Mortality rates after brain injury are highest in people with a severe TBI. In the first year after a TBI, people who survive are more likely to die from seizures, septicemia, pneumonia, digestive conditions, and all external causes of injury than are other people of similar age, sex, and race. [15] However, the mortality rate after severe TBI has decreased since the late 20th century. [16]
See also the following related Medscape Drugs & Diseases topics:
Initial Evaluation and Management of CNS Injury
Neurocritical Care for Severe Pediatric Traumatic Brain Injury
Traumatic Brain Injury (TBI) - Definition, Epidemiology, Pathophysiology
Pathophysiology
Classification as Primary or Secondary injury
TBI may be divided into primary injury and secondary injury. Primary injury is induced by mechanical force and occurs at the moment of injury. Secondary injury is not mechanically induced. It may be delayed from the moment of impact, and it may superimpose injury on a brain already affected by a mechanical injury. [1]
Primary injury
The 2 main mechanisms that cause primary injury are contact (eg, an object striking the head or the brain striking the inside of the skull) and acceleration-deceleration. Primary injury due to contact may result in injury to the scalp, fracture to the skull, and surface contusions. Primary injury due to acceleration-deceleration results from unrestricted movement of the head and leads to shear, tensile, and compressive strains. These forces can cause intracranial hematoma, diffuse vascular injury, and injury to cranial nerves and the pituitary stalk. [1]
Contusions are distinct areas of swollen brain tissue. [17] They are typically found on the poles of the frontal lobes, the inferior aspects of the frontal lobes, the cortex above and below the operculum of the sylvian fissures, and the lateral and inferior aspects of the temporal lobes.
Intracranial hematoma is the most common cause of death and clinical deterioration after TBI. Hematomas are categorized as follows [1] :
-
Epidural hematomas - These are usually caused by fracture of the temporal bone and rupture of the middle meningeal artery. With epidural hematomas, clotted blood collects between the bone and the dura. Because the source of bleeding is arterial, this type of hematoma can grow quickly and create pressure against the brain tissue.
-
Subdural hematomas - Such hematomas are usually caused by rupture of the bridging veins in the subdural space. They can grow large enough to act as mass lesions, and they are associated with high morbidity and mortality rates.
-
Subarachnoid hematomas - These result from damage to blood vessels in the posterior fossa stalk.
Diffuse axonal injury (DAI) is one of the most common and important pathologic features of TBI. It constitutes mostly microscopic damage, and it is often not visible on imaging studies. The main mechanical force that causes DAI is rotational acceleration of the brain, resulting in unrestricted head movement. Rotational acceleration produces shearing and tensile forces, and axons can be pulled apart at the microscopic level. Microscopic evaluation of the brain tissue often shows numerous swollen and disconnected axons. Rapid stretching of axons is thought to damage the axonal cytoskeleton and, therefore, disrupt normal neuron function. [18]
Secondary injury
Secondary injury may occur hours or even days after the inciting traumatic event. Injury may result from impairment or local declines in cerebral blood flow (CBF) after a TBI. Decreases in CBF are the result of local edema, hemorrhage, or increased intracranial pressure (ICP). As a result of inadequate perfusion, cellular ion pumps may fail, causing a cascade involving intracellular calcium and sodium. Resultant calcium and sodium overload may contribute to cellular destruction. Excessive release of excitatory amino acids, such as glutamate and aspartate, exacerbates failure of the ion pumps. As the cascade continues, cells die, causing free radical formation, proteolysis, and lipid peroxidation. These factors can ultimately cause neuronal death. [19]
The exact role of the inflammatory response in secondary injury is not known. However, it is believed to contribute to cell damage. [19, 20]
Clinical conditions associated with the risk of a decreased CBF are arterial hypotension, hypoxemia, intracranial hemorrhage and malignant brain edema, and hyperthermia. [19]
Classification as Focal or Diffuse Injury
Another injury classification based on clinical and neuroradiologic evaluation has been proposed. In this classification, TBI would be described as focal or diffuse. Focal injuries include scalp injury, skull fracture, and surface contusions and are generally be caused by contact. Diffuse injuries include DAI, hypoxic-ischemic damage, meningitis, and vascular injury and are usually caused by acceleration-deceleration forces. These 2 forms of injury are commonly found together.
See also the following related Medscape Drugs & Diseases topic:
Measures of Severity
The classification of TBIs plays an important role in determining the patient's treatment, rehabilitation potential, and prognosis.
Glasgow Coma Scale
The most common classification system for TBI severity is based on the Glasgow Coma Scale (GCS) score determined at the time of injury. The GCS is a 3- to 15-point scale used to assess a patient's level of consciousness and level of neurologic functioning. [2, 3] It consists of 3 sections, each of which is scored: best motor response, best verbal response, and eye opening (Table 1). A total score of 3-8 for the 3 sections indicates severe TBI, a score of 9-12 indicates moderate TBI, and a score of 13-15 indicates mild TBI.
Table 1. Glasgow Coma Scale (Open Table in a new window)
Score |
Best Motor Response |
Best Verbal Response |
Eye Opening |
1 |
None |
None |
None |
2 |
Decerebrate posturing |
Mutters unintelligibly |
Opens to pain |
3 |
Decorticate posturing |
Inappropriate speech |
Opens to command |
4 |
Withdraws to pain |
Confused |
Opens spontaneously |
5 |
Localizing response to pain |
Alert and oriented |
NA |
6 |
Obeys commands |
NA |
NA |
Total* |
1-6 |
1-5 |
1-4 |
Source—Teasdale and Jennett, 1974. [3] Note—NA = not applicable. * The total of the motor, verbal, and eye-opening scores (range, 3-15) indicates the severity of a TBI, as follows: 3-8 is severe TBI, 9-12 is moderate TBI, and 13-15 is mild TBI. |
|||
Loss of consciousness
The duration of loss of consciousness (LOC) is another measure of the severity of a TBI (Table 2). [21]
Table 2. Severity of TBI Based on the Duration of LOC (Open Table in a new window)
Severity of TBI |
Finding |
Mild |
Mental status change or LOC < 30 min |
Moderate |
Mental status change or LOC 30 min to 6 h |
Severe |
Mental status change or LOC > 6 h |
Source—Greenwald et al, 2003. [21] |
|
Other classifications of severity
As early as 1932, Russell introduced the concept of posttraumatic amnesia (PTA) and later defined it as the time elapsed from injury to the moment when patients can demonstrate continuous memory of what is happening around them. [4] Lack of accurate records may make this system difficult to use retrospectively. Zafonte found that the duration of PTA (as measured by using the Galveston Orientation and Amnesia Test) appeared to be a significant predictor of functional outcome after a TBI and may best reflect the overall severity of injury. [22, 23]
Relatively uncommon measures of severity include the number of days that are required to achieve a total GCS score of 15, the number of days that are needed to achieve a GCS motor score of 6, and the Abbreviated Injury Scale Head score.
Another system for assessing TBI severity is the Simplified Motor Score (SMS). The SMS is a 3-point scale developed to address the perceived limitations of the GCS, such as its complexity and poor interrater reliability.
Table 3. Simplified Motor Score (Open Table in a new window)
Score |
Best Motor Response |
0 |
Withdraws to pain or worse |
1 |
Localizes pain |
2 |
Obeys commands |
A study by Thompson et al determined that in an out-of-hospital setting, the SMS was similar to the GCS score for predicting TBI outcomes. [24]
Medical Complications
Posttraumatic seizures
Posttraumatic seizures (PTS) frequently occur after moderate or severe TBI. Seizures are usually general or partial, and absence seizures are uncommon. Seizures are classified according to the time elapsed after the initial injury: Immediate seizures occur in the first 24 hours. Early seizures occur in the first 2-7 days, and late seizures occur after 7 days.
The incidence of late PTS is in the range of 5-18.9%. Risk factors include chronic alcoholism, older age at the time of injury, and a history of seizure disorder. Approximately one half to two thirds of patients with these risk factors develop late PTS within the first year after injury. [25] If a patient with TBI has 1 PTS, his or her likelihood of having another is approximately 50%. [26]
A study by Majidi et al, using information from the National Trauma Data Bank, indicated that the rate of early, in-hospital seizures among patients with TBI is 0.4%, with seizure patients more likely to have African-American ethnicity, moderate TBI, a history of alcohol dependence, fall as the mechanism of injury, and subdural hematoma. The study also suggested that TBI patients with in-hospital seizures have higher rates of complications such as pneumonia, acute respiratory distress syndrome, acute kidney injury, and increased intracranial pressure. Moreover, seizure patients in the study tended to have worse hospital outcomes, with a higher rate of discharge to nursing facilities. [27]
Temkin showed that prophylactic use of phenytoin is effective during the first week after a TBI. [28] However, the author recommended discontinuation after 1 week if no seizures develop because of its lack of effect in preventing late PTS and because of possible cognitive adverse effects.
Although phenytoin maybe effective in preventing seizures in the first week after a TBI, at least 50% of patients with TBI have late seizure activity for which phenytoin may not be effective.
Hydrocephalus
Hydrocephalus is characterized as communicating or noncommunicating on the basis of the causative obstruction. Noncommunicating hydrocephalus occurs secondary to an obstruction in the ventricular system before the point at which cerebrospinal fluid (CSF) exits the fourth ventricle. Communicating hydrocephalus is the most common form after TBI and occurs when the obstruction is in the subarachnoid space. [29]
Patients with hydrocephalus can clinically present with nausea, vomiting, headache, papilledema, obtundation, dementia, ataxia, and/or urinary incontinence. The diagnosis is based on clinical suspicion, diagnostic imaging, and radio-isotope cisternography. Treatment usually consists of lumbar puncture or shunt placement.
Deep vein thrombosis
Deep vein thrombosis (DVT) is common in persons with TBI, with an incidence as high as 54%. [5] In patients with TBI, risk factors for DVT include immobility, lower extremity fracture, paralysis, and disruption in coagulation and fibrinolysis.
Complications of DVT include pulmonary embolism (PE), postthrombotic syndrome, and recurrence. Because DVT can result in PE, it can be critical. Given the rapid decline in pulmonary function when a PE has completely occluded the pulmonary capillary system, sudden death may be the first clinical sign. [30] Other clinical signs of PE include shortness of breath, chest pain, and pulmonary crackles; these are usually present with small emboli. However, clinical signs and symptoms are often absent in the patient with DVT. Therefore, a high index of suspicion and timely medical intervention are of utmost importance.
The most common modalities for detecting DVT are venous Doppler ultrasonography and contrast-enhanced venography. Venography remains the criterion standard for diagnosing DVT. Noninvasive Doppler ultrasonography is most commonly used because of its low risk of adverse effects compared with venography. [31]
Prophylaxis for DVT should be started as soon as possible. These measures include use of elastic compression stockings, intermittent pneumatic compression, vena cava filters, warfarin, unfractionated heparin (UH), and/or low–molecular weight heparin (LMWH). Mechanical methods of prophylaxis are generally used in patients with a high risk of bleeding or in combination with anticoagulation. [31] The choice of prophylaxis should be patient specific and based on his/her existing comorbidities.
A study by Frisoli et al suggested that in patients with traumatic intracranial hemorrhage, the initiation of early venous thromboembolism (VTE) chemoprophylaxis (ie, less than 24 hours after injury) is safe. Outcome rates, including for radiographic intracranial hemorrhage expansion, the need for delayed decompressive surgery for refractory intracranial pressure elevation, and all-cause mortality, were similar to those for patients who underwent VTE chemoprophylaxis more than 48 hours after injury. [32]
Treatment for DVT and/or PE in patients with TBI is similar to treatment for these conditions in the general population. Treatment generally consists of the administration of an immediate-acting anticoagulant (UH or LMWH), followed by chronic anticoagulation with warfarin (target international normalized ratio [INR], 2-3). Heparin or LMWH should be continued until the desired INR is achieved and stable. The duration of anticoagulation is specific to the indication and the patient. [33] Use of anticoagulation in the patient with TBI could increase the risk for intracerebral hemorrhage. Each patient should be evaluated for his/her risk of intracerebral hemorrhage and of falling.
A retrospective study by Dhillon et al indicated that in patients with TBI, propranolol may reduce the risk of VTE. The report looked at intensive care unit patients with TBI who had an Injury Severity Scale (ISS) score of 25 or greater. The investigators found that the adjusted VTE rate in patients in whom at least one dose of propranolol was administered within 24 hours of admission was lower than that in patients who received no propranolol while hospitalized, with the adjusted odds ratio being 0.20. The study pointed to the fact that in TBI, a survival advantage can be achieved through the administration of agents, such as propranolol, that interfere with the TBI-related intrinsic catecholamine response. Nonetheless, it was noted that the mechanism behind propranolol’s apparent association with VTE reduction requires further examination. [34]
Heterotopic ossification
Heterotopic ossification is described as ectopic bone formation in the soft tissue surrounding the joints. In TBI, the incidence of heterotopic ossification is 11-76%, with a 10-20% incidence of clinically significant heterotopic ossification. [6] Heterotopic ossification generally causes joint pain and decreases range of motion (ROM). It is often associated low-grade fever, peri-articular swelling, peri-articular warmth, and peri-articular erythema.
In decreasing order of frequency, heterotopic ossification occurs in the hips, knees, elbows, shoulders, hands, and spine. Risk factors associated with the development of heterotopic ossification after TBI are a posttraumatic coma lasting longer than 2 weeks, limb spasticity, and decreased mobility. The risk of heterotopic ossification is greatest during the first 3-4 months after injury. [30]
The pathophysiology of heterotopic ossification remains unclear. However, inappropriate differentiation of mesenchymal cells into osteoblasts is believed to be the basic defect. Autonomic dysregulation (due to increased vascularity and venous hemostasis), humoral factors, and local inflammatory mediators contribute to the development of heterotopic ossification.
Laboratory and radiologic data are critical in the diagnosis of heterotopic ossification. Although serum alkaline phosphatase levels and erythrocyte sedimentation rates are nonspecific markers, they are often elevated in the early phases of heterotopic ossification. Therefore, elevated levels might suggest additional evaluation.
Three radiologic modes are useful for diagnosing heterotopic ossification: plain radiography, ultrasonography, and triple-phase bone scanning. Triple-phase bone scanning reveals heterotopic ossification the earliest. Plain radiographic and ultrasonographic findings may lag behind results of bone scans because of lack of early calcification in heterotopic ossification. Plain radiographic findings lag behind triple-phase bone scan results by 2-3 weeks. However, plain radiography can be used early to rule out an underlying fracture.
The mainstay of preventing heterotopic ossification in patients with TBI is ROM exercise. The use of forceful ROM is somewhat controversial because it is thought to be a cause of heterotopic ossification, but data from human studies have not demonstrated this mechanism.
The prophylactic role of nonsteroidal anti-inflammatory drugs (NSAIDs), low-dose radiation, or bisphosphonates remains unclear. NSAIDs and etidronate can help with pain management. The risks and benefits of these drugs in managing established heterotopic ossification should be assessed.
Heterotopic ossification may result in functional impairment, and patients may require surgical excision. To minimize risk of recurrence, surgical excision has traditionally been delayed 12-18 months to allow the heterotopic bone to mature. However, authors have questioned this delay. [6]
Spasticity
Tone is defined as resistance to stretch or movement across a joint during relaxation. Spasticity is defined as velocity-dependent increase in tone. Rigidity is also a function of tone, but it is defined as the non–velocity-dependent increase in tone. These 3 terms are not interchangeable.
In one inpatient rehabilitation unit, spasticity was found in an estimated 25% of patients with TBI. [35]
Spasticity is most often encountered in lesions of the upper motor neurons, whereas rigidity is most common in disorders of the basal ganglia. The morbidity associated with spasticity is variable, because in some people, spasticity may assist in leg extension for walking or finger flexion for grasping. Prolonged low tone after TBI is generally predictive of poor motor recovery.
Guidelines for the treatment of spasticity are generally based on (1) any resulting limitation in function, (2) pain, (3) prevention of contracture, and (4) assistance with positioning. [35] First-line treatments for spasticity are correct positioning of the involved body segment and ROM exercises. Second-line treatments include splinting, casting, and other modalities.
Treatment varies according to whether the spasticity is generalized or local. Generalized spasticity is usually treated systemically. Dantrolene sodium is preferred in patients with TBI because of its lack of cognitive and sedative adverse effects.
Other drugs used to manage spasticity include baclofen, tizanidine, clonidine, and benzodiazepines. Their use may be limited because of their sedative and cognitive adverse effects. Local treatments for spasticity include chemical neurolysis with phenol or alcohol injections and with botulinum toxin type A and type B injections.
GI and GU complications
GI and GU complications remain among the most common sequelae in patients with TBI. Some of the most frequent GI complications are stress ulcers, dysphagia, bowel incontinence, and elevated levels on liver function tests. Underlying constipation and/or impaired communication and mobility are often the causes of bowel incontinence. The use of oral stool softeners, laxatives, and rectal suppositories may facilitate full bowel evacuation and improve incontinence.
GU complications include urethral strictures, urinary tract infections, and urinary incontinence. An appropriate workup to evaluate GU symptoms and rule out infection is indicated. When the causes of urinary incontinence are impaired communication and mobility, a trial of a timed voiding is indicated to manage overflow incontinence. Patients are taken to the bathroom and given the opportunity to void without instrumentation every 2 hours during the day and every 4 hours overnight.
If the patient is unable to void or cannot evacuate the urinary bladder to completion, intermittent straight catheterization may be necessary in the acute recovery period. Although not preferred, diapers and condom catheters may be needed if urinary incontinence does not improve.
Voiding dysfunction and upper urinary tract status were studied in 57 survivors of coma resulting from TBI. Direct statistical links were found between urge incontinence, detrusor overactivity, and poor neurologic functional outcome, as well as between detrusor overactivity and right hemisphere injuries, and between impaired detrusor contractility and left hemisphere damages. [36]
Gait abnormalities
Martini et al performed gait analysis on subjects with and without a remote concussion history, measuring velocity, step length, stride width, and time in single-leg versus double-leg stance. They found that subjects with a remote concussion history showed slowed walking velocity, greater time in double-leg stance, and less time in single-leg stance, speculating that the patients with concussion histories are trying to limit injury risk from falls. They suggest that patients with even remote concussion histories may have prolonged risk for fall injuries. [37]
Chronic traumatic encephalopathy
Persons with a history of repetitive brain trauma, including boxers and American-style football players, are at risk for developing chronic traumatic encephalopathy (CTE), a progressive degenerative disease. [38] Degenerative changes, which can begin months to decades after the patient’s last brain trauma, include atrophy of the cerebral hemispheres, medial temporal lobe, thalamus, mammillary bodies, and brainstem. The condition is also characterized by ventricular dilatation and by fenestration of the cavum septum pellucidum, as well as the accumulation of phosphorylated tau in the brain, with deposits of the protein being found in the sulci and in perivascular areas of the cerebral cortex. [39]
According to a consensus panel of the National Institute of Neurological Disorders and Stroke/National Institute of Biomedical Imaging and Bioengineering, the pathognomonic lesion of CTE is “an accumulation of abnormal hyperphosphorylated tau (p-tau) in neurons and astroglia distributed around small blood vessels at the depths of cortical sulci and in an irregular pattern.” [40]
A study by Armstrong et al of 11 cases of CTE found dotlike lesions to be consistently present in the brain, suggesting a similarity between CTE and both argyrophilic grain disease and Parkinson disease dementia. [41]
Symptoms of CTE include memory loss, confusion, impaired judgment, reduced impulse control, aggression, explosive anger, depression, and progressive dementia. [42, 43, 44, 45]
According to a report from the US Department of Veterans Affairs and Boston University, 87 of 91 deceased former players for the National Football League (NFL) (96%) who donated their brains for study were found to have CTE (although the donors had, prior to death, expressed concern that they might have CTE and so may have had a higher proportion of the disease than does the overall population of former NFL players). [46, 47]
A study by Eagle et al indicated that in former professional players of American-style football, those suffering from depression, anxiety, and sleep apnea have a greater likelihood of a premortem diagnosis of CTE. The report, on about 4000 former professional football players, found that the odds ratio (OR) for such diagnosis in those with depression was 9.5, and in those with both depression and anxiety, 12.2. In subjects with a combination of depression and anxiety, those who also had sleep apnea had an OR of 2.7. [48]
See also the following related Medscape Drugs & Diseases topic:
Agitation
Posttraumatic agitation is common after TBI. Baguley and colleagues found that 25% of patients with TBI were classified as being aggressive during the follow-up periods in their 5-year study. [49] Furthermore, aggression was consistently associated with depression or young age at the time of injury.
Corrigan developed a 14-item instrument, the Agitated Behavior Scale (ABS), to quantify levels of agitation after TBI (see image below). [50] Bogner and colleagues found the ABS a reliable instrument for measuring agitation in patients following TBI. [51]
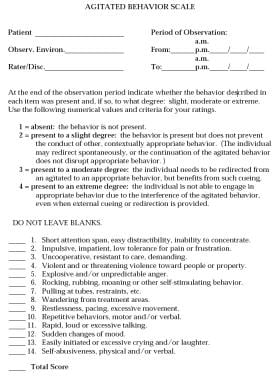 Agitated Behavior Scale, developed by John D Corrigan, PhD, ABPP, Professor, Department of Physical Medicine and Rehabilitation, The Ohio State University. Permission for publication granted by Dr. Corrigan.
Agitated Behavior Scale, developed by John D Corrigan, PhD, ABPP, Professor, Department of Physical Medicine and Rehabilitation, The Ohio State University. Permission for publication granted by Dr. Corrigan.
Before posttraumatic agitation is treated, other medical conditions should be considered. After TBI, the patient may be uncomfortable, and impaired recognition and an inability to communicate are often agitating factors. Pain is a common (but often overlooked) cause of posttraumatic agitation. Combined with a diminished ability to communicate and/or an inability to cope with pain, agitation is not surprising. Furthermore, clinicians should consider the possibility of infection, electrolyte imbalance, adverse effects of drugs, psychosis, and insomnia.
Environmental modifications are usually the first treatment. Minimizing unnecessary stimuli and assisting with tools for orientation may help to reduce the onset of agitation. External stimuli, such as noisy rooms, bright lights, and frequent visitors, should be minimized. Use of centrally acting drugs that may exacerbate agitation should be minimized. Physical restraints often exacerbate posttraumatic agitation and should not be used routinely. Restraints should be used only as a last resort to secure patient, staff, and visitor safety. However, the use of less restrictive restraints, such as net-covered beds (eg, Vail beds), has become acceptable and popular in the treatment of the agitated patient with a brain injury.
In addition to environmental and behavioral modifications, various drugs, such as high-dose beta blockers, anticonvulsants, and antidepressants (particularly selective serotonin re-uptake inhibitors [SSRIs]), have had some success in the management of posttraumatic agitation. [52] Brooke and colleagues found that the intensity of agitation was significantly lower in patients with TBI who were treated with propranolol than in subjects who were treated with placebo. [53] In addition, amantadine has shown some usefulness in reducing posttraumatic agitation. [54, 55] Case studies support the use of lamotrigine [56] or divalproex [57] to manage posttraumatic agitation.
The use of antipsychotics to treat posttraumatic agitation is controversial. Their effects on cognition and recovery are poorly studied. Antipsychotics may cause excessive drowsiness, exacerbate cognitive deficits, and inhibit neuronal recovery. Stanislav suggested that select areas of cognition may improve after thioridazine and haloperidol are discontinued. [58]
Symptoms Of TBI
Long-term physical, cognitive, and behavioral impairments are the factors that most commonly limit a patient's re-integration into the community and his/her return to employment.
In a study by Kraus and colleagues of 235 patients, the symptoms most commonly reported 6 months after mild TBI were fatigue (43%), weakness (43%), memory deficits (40%), headache (36%), and dizziness (34%). [59] Other investigators found similar complaints after mild TBI. [60, 61] The symptoms have collectively been referred to as postconcussion syndrome. [62] Kraus and co-authors found that approximately 83% of patients with mild TBI reported 1 or more physical complaints at the end of their 6-month follow-up period. [59, 63]
Insomnia
In one study, patients with TBI reported higher rates of sleep changes than did sex-matched control subjects (80% vs 23%). [29] The TBI group reported more nighttime awakenings and longer sleep-onset latency than did the other group. Increased levels of anxiety and depression were risk factors that may have partly accounted for increased complaints of excessive daytime sleepiness.
A cross-sectional case-comparison study by Wei et al found a high prevalence of sleep disturbances, including obstructive sleep apnea (OSA), insomnia, and daytime sleepiness, in adults aged 65 years or above who had suffered traumatic brain injury (TBI). The investigators reported a significant correlation in older adults between male gender and OSA, while the presence of higher degrees of depression and pain was correlated with insomnia, and the occurrence of insomnia was associated with daytime sleepiness. The data also indicated that the correlation of OSA and insomnia with low quality of life is significant in the older population. [64]
Light therapy may mitigate TBI-related sleep disturbances. In a small study that included 18 adults with a history of at least 1 mild TBI and sleep disturbance that developed after, or was exacerbated by, the most recent injury, morning bright-light therapy led to improvements in sleep, cognition, emotion, and brain function. [65, 66]
Cognitive decline
Khateb and colleagues found that patients with chronic TBI who were treated with donepezil had slight improvements in neuropsychological test results, including in speed of processing, learning attention, and divided attention. [67] Light therapy may also be helpful. [66]
Posttraumatic headache
Walker and co-authors found that nearly 38% of patients with moderate or severe TBI had acute posttraumatic headache, usually daily and most commonly in the frontal region. [68] Almost all of the patients who reported posttraumatic headache at 6 months also reported symptoms at 12 months.
Chronic posttraumatic headache is common, and the pathophysiology is not well understood. Tension-type headaches are the most common form, but exacerbations of migrainelike headaches are also frequent. [69]
A study by Ashina et al found that among individuals suffering from persistent posttraumatic headache following mild TBI, the pain in 61% of them manifested as chronic migrainelike headache. In 29% of cases, combined episodic migrainelike and tension-type–like headache was reported, while 9% of individuals had chronic tension-type–like headache only. Stress, lack of sleep, and bright lights served as the most frequent headache triggers. The mean headache frequency for all 100 patients in the report was 25.4 days per month. [70]
Treatment of posttraumatic headache is similar to that of primary headache if structural lesions or abnormalities are absent. [69]
Posttraumatic depression
Mood disorders, particularly depression, are common sequelae of TBI. Major depression is found in about 40% of patients hospitalized for TBI. [71] Depression after TBI is further associated with cognitive decline, [7, 8, 9, 10] anxiety disorders, substance abuse, dysregulation of emotional expression, and aggressive outbursts. [72] Whitnall and colleagues reported that persistent disability (5-7 years after TBI) was strongly associated with depression and anxiety, and that it was more poorly associated with initial severity or persistent cognitive impairments. [73]
Dikmen et al found that the following factors are predictive of posttraumatic depression: educational level less than high school, unstable work history prior to injury, and alcohol abuse. [72]
Treatment options for posttraumatic depression include counseling, participation in support groups, and antidepressant medication. Early after TBI, a grief reaction is common, and this is better treated with supportive therapies than with other approaches. If drugs are used, their profiles, including their adverse effects and interactions, must be carefully considered to prevent worsening sedation or cognitive impairment. Methylphenidate and sertraline are beneficial in treating posttraumatic depression. [74]
Methylphenidate is commonly used to treat patients with hypo-arousal, initiation, and attention problems associated with TBI. Methylphenidate may hasten recovery after TBI. The positive effects of methylphenidate are improved speed in processing and sustained attention. [75] By potentiating dopamine, amantadine may improve arousal, attention, and executive functions. [76]
Outcome Measures
Tools to effectively measure outcome are needed to quantify results. [77] Outcome measures can be used to assess the effectiveness of different treatments.
Three tools commonly used to measure outcome after TBI are the Functional Independence Measure (FIM), [11] the Glasgow Outcome Scale (GOS), [12] and the Disability Rating Scale (DRS).
The FIM is one of the most widely used measures of function in rehabilitation (Table 3). It is an 18-item scale used to assess the patient's level of independence in mobility, self-care, and cognition. However, it may lack sensitivity in patients with very low or very high levels of function. Therefore, the FIM may be an inadequate outcome measure for patients at either extreme of TBI recovery.
Table 4. Functional Independence Measure (Open Table in a new window)
Clinical Area |
|
Self-care |
A. Eating |
B. Grooming |
|
C. Bathing |
|
D. Dressing - upper body |
|
E. Dressing - lower body |
|
F. Toileting |
|
Sphincter control |
G. Bladder management |
H. Bowel management |
|
Transfers |
I. Bed, chair, wheelchair |
J. Toilet |
|
K. Tub, shower |
|
Locomotion |
L. Walking, wheelchair |
M. Stairs |
|
Motor subtotal score: |
|
Communication |
N. Comprehension |
O. Expression |
|
Social interaction |
P. Expression |
Q. Problem solving |
|
R. Memory |
|
Cognitive subtotal score: |
|
TOTAL FIM SCORE: |
|
Source—Keith et al, 1987. [11] |
|
The GOS is a scoring system commonly used to rate outcomes after TBI (Table 4). [12]
Table 5. Glasgow Outcome Scale (Open Table in a new window)
Score |
Rating |
Definition |
1 |
Dead |
Nonsurvival |
2 |
Persistent vegetative |
Minimal responsiveness |
3 |
Severe disability |
Conscious but disabled; dependent on others for daily support |
4 |
Moderate disability |
Disabled but independent; can work in sheltered setting |
5 |
Good recovery |
Resumption of normal life despite minor deficits |
Source—Jennett and Bond, 1975. [12] |
||
The DRS (see the image below) is intended to accurately measure general functional changes over the course of recovery after TBI, where a score of 0 indicates no disability and 29 indicates an extreme vegetative state. [78] The DRS includes 8 items, including the GCS score and disability and return-to-work measures.
Prognosis
Determining the patient's prognosis after TBI remains difficult and complex. The heterogeneity of patients' premorbid health status, the natures and severities of injury, the intervals from injury to initial treatment, the acute interventions, and the differences in follow-up create difficulty in developing a simple and accurate scoring system. [79]
Brown and co-authors found the following variables to be predictive of outcome [80] :
-
Initial GCS score
-
Duration of PTA
-
Amnesia [81]
-
Sex
-
Age
-
Years of education
A retrospective cohort study by Watanitanon et al found that among patients with moderate TBI, a poor outcome was twice as likely in those aged 45-64 years and five times as likely in patients over age 80 years, than it was in patients aged 18-44 years. [82]
Cuthbert et al investigated injury severity and sociobiologic and socioeconomic factors to predict discharge location (home vs not to home) in adults with moderate to severe TBI. They found GCS and acute hospital length of stay to be the most predictive in discharges to home versus not to home (ie, higher GSC and shorter LOS were more likely to be discharged to home). They also found that old age was associated with a decreased likelihood of discharge to rehabilitation and more likely to be discharged to subacute rehabilitation. [83]
Bogner and colleagues found that substance abuse contributed to the prediction of life satisfaction and productivity, while violent etiology was not a significant contributor to prediction. [84] Corrigan and co-authors found that a lack of pre-injury history of substance abuse and the possession, at the time of follow-up, of gainful employment were associated with higher life satisfaction 1-2 years after TBI. [85] An evaluation of the employment outcome in patients with moderate to severe TBI found that patients with comorbid psychiatric symptoms and impaired cognitive functioning are at the highest risk of long-term unemployment. [86]
Three-month GOS scores are powerful independent predictors of long-term outcome after severe TBI. [87, 88] Davis and colleagues found that GCS scores in the field and on the patient's arrival in the emergency department are highly predictive of mortality and of a need for neurosurgical care. [89] Davis's study also found that an increase in the GCS score from the field to the emergency department is highly predictive of survival. Studies have shown that the level of abnormality on brain computed tomography (CT) scans and the early loss of autoregulation of ICP are predictive of the outcome. [90, 91, 92]
In a secondary analysis of data on 365 patients with moderate or severe TBI from a randomized trial, Badri et al found that average ICP in the first 48 hours of monitoring independently predicted mortality as well as a composite endpoint of functional and neuropsychological outcome at 6 months. Average ICP, however, was not independently associated with neuropsychological functioning. [93] In patients with severe TBI due to acute subdural hematoma, TBI severity, age and neurological status are the primary factors influencing outcomes, and nonoperative management is associated with a significantly increased mortality risk. [94]
Further research is needed to develop simple prognostic tools. Improved prognostic tools, if available, would assist clinicians in planning for patients' long-term care and needs.
Questions & Answers
Overview
How common is traumatic brain injury (TBI)?
How is traumatic brain injury (TBI) classified?
How is traumatic brain injury (TBI) severity measured?
What are the possible complications of traumatic brain injury (TBI)?
What are the long-term impairments of traumatic brain injury (TBI)?
How are outcomes measured after a traumatic brain injury (TBI)?
What is the prevalence of traumatic brain injury (TBI) in the US?
Which patient groups are at highest risk for traumatic brain injury (TBI)?
What are the most common causes of traumatic brain injury (TBI)?
What is the mortality rate for traumatic brain injury (TBI)?
What is the pathophysiology of traumatic brain injury (TBI)?
What are mechanisms that cause primary traumatic brain injury (TBI)?
How are intracranial hematomas categorized in traumatic brain injury (TBI)?
What is the role of diffuse axonal injury (DAI) in traumatic brain injury (TBI)?
What is the pathophysiology of secondary traumatic brain injury (TBI)?
What are focal or diffuse classifications in traumatic brain injury (TBI)?
What is the role of the classification in the management of traumatic brain injury (TBI)?
What is the role of loss of consciousness (LOC) in the assessment of traumatic brain injury (TBI)?
What are the less commonly used methods to determine severity in traumatic brain injury (TBI)?
How is Simplified Motor Score (SMS) fused to determine severity in traumatic brain injury (TBI)?
What are posttraumatic seizures (PTS) in patients with traumatic brain injury (TBI)?
What are the signs and symptoms of hydrocephalus in traumatic brain injury (TBI)?
What is deep vein thrombosis (DVT) in traumatic brain injury (TBI)?
How is deep vein thrombosis (DVT) prevented in traumatic brain injury (TBI)?
How is deep vein thrombosis (DVT) treated in traumatic brain injury (TBI)?
What is heterotopic ossification in traumatic brain injury (TBI)?
How is heterotopic ossification diagnosed in traumatic brain injury (TBI)?
How is heterotopic ossification prevented in traumatic brain injury (TBI)?
How is heterotopic ossification treated in traumatic brain injury (TBI)?
What is spasticity in traumatic brain injury (TBI)?
How is spasticity treated in traumatic brain injury (TBI)?
What are the possible GI and genitourinary (GU) complications of traumatic brain injury (TBI)?
What are possible gait abnormalities in traumatic brain injury (TBI)?
What is chronic traumatic encephalopathy?
How is agitation evaluated in traumatic brain injury (TBI)?
How is agitation treated in patients with traumatic brain injury (TBI)?
What are the signs and symptoms of traumatic brain injury (TBI)?
How do sleep disturbances manifest in traumatic brain injury (TBI), and how is insomnia treated?
How is cognitive decline treated in chronic traumatic brain injury (TBI)?
How prevalent is acute posttraumatic headache in traumatic brain injury (TBI)?
How is chronic posttraumatic headache in traumatic brain injury (TBI) treated?
How is depression treated in traumatic brain injury (TBI)?
Which tools are used to measure outcome in patients with traumatic brain injury (TBI)?
How is the Glasgow Outcome Scale (GOS) used to determine outcomes for traumatic brain injury (TBI)?
What are the challenges to determining prognosis of traumatic brain injury (TBI)?
Which factors have been used to predict outcomes for traumatic brain injury (TBI)?
-
Disability Rating Scale (DRS).
-
Agitated Behavior Scale, developed by John D Corrigan, PhD, ABPP, Professor, Department of Physical Medicine and Rehabilitation, The Ohio State University. Permission for publication granted by Dr. Corrigan.








