Practice Essentials
Head trauma accounts for 80% or more of the traumatic injuries leading to death in US children older than 1 year. Most pediatric head trauma occurs secondary to motor vehicle accidents, falls, assaults, recreational activities, and child abuse. See the image below.
See Pediatric Concussion and Other Traumatic Brain Injuries, a Critical Images slideshow, to help identify the signs and symptoms of traumatic brain injury (TBI), determine the type and severity of injury, and initiate appropriate treatment.
Signs and symptoms
Patients with head trauma may experience one or a combination of primary injuries, including the following:
-
Scalp injury
-
Skull fracture (eg, basilar skull fracture)
-
Concussion
-
Contusion
-
Intracranial and/or subarachnoid hemorrhage
-
Epidural and/or subdural hematoma
-
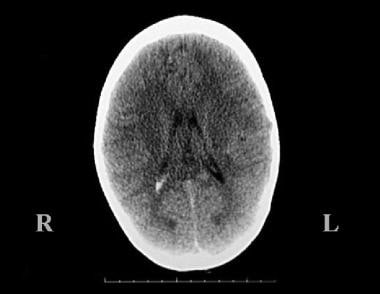
Intraventricular hemorrhage (see the image below)
-
Penetrating injuries
-
Diffuse axonal injury
Patients with severe head trauma are at increased risk of developing cerebral edema, respiratory failure, and herniation secondary to increased intracranial pressure.
See Presentation for more detail.
Diagnosis
Patients with head trauma often have multiple organ injuries. Assessment of patients with severe head injuries includes a primary survey and a secondary survey.
The primary survey is a focused physical examination directed at identifying and treating life-threatening conditions present in a trauma patient—thereby preventing secondary brain injury—and includes evaluation of the following:
-
Airway (eg, presence of foreign bodies, facial lacerations, bone instability, tracheal deviation, circumoral cyanosis), breathing (eg, apnea, hypoventilation), and circulatory status (eg, Cushing triad of bradycardia, hypertension, altered respiration)
-
Neurologic status (eg, alert, verbal, pain, unresponsive [AVPU] system; pediatric Glasgow Coma Scale [GCS])
The secondary survey of patients with head trauma is a detailed examination and assessment of individual systems—with the goal of identifying all traumatic injuries and directing further treatment—and includes evaluation of the following:
-
Head (eg, cervical deformity, step-off, malalignment; lacerations; depressions; Battle sign or retroauricular/mastoid ecchymosis; raccoon eyes/periorbital ecchymosis; hemotympanum; cerebrospinal fluid otorrhea and rhinorrhea; bulging of fontanel)
-
Respiratory patterns (eg, apnea, Cheyne-Stokes, hyperventilation, apneustic respiration)
-
Neurologic status (eg, dilated/pinpoint pupil(s), Horner syndrome, eye deviation, retinal hemorrhage, motor/sensory dysfunction)
Testing
The following laboratory studies are used to assess children with head trauma:
-
Serial complete blood counts
-
Blood chemistries (eg, amylase and lipase levels)
-
Coagulation profile (including prothrombin time, international normalized ratio, activated partial thromboplastin time, fibrinogen level)
-
Type and crossmatch
-
Arterial blood gas
-
Blood or urine toxicology screening
Imaging studies
Radiologic studies used to evaluate pediatric head injuries include the following:
-
Computed tomography (CT) scanning of the head: Most useful imaging study for patients with severe head trauma or unstable multiple organ injury [1]
-
Magnetic resonance imaging (MRI) of the brain: More sensitive than CT scanning for intracranial evaluation of TBIs
-
Ultrasonography: For neonates and small infants with open fontanels; focused point-of-care ultrasonography has a high specificity for pediatric skull fractures [2]
Procedures
Monitoring of intracranial pressure is indicated in the following patients:
-
Salvageable patients with severe TBI and an abnormal CT scan
-
Those with severe TBI and a normal CT scan in the presence of unilateral/bilateral motor posturing or a systolic blood pressure below the fifth percentile for age
-
Conscious patients with CT findings suggesting risk of neurologic deterioration
-
Inability to perform serial neurologic exams due to pharmacologic sedation/anesthesia
Removal of cerebrospinal fluid via external ventricular drains or lumbar drains may be necessary in patients with increased intracranial pressure.
See Workup for more detail.
Management
The goal of medical care of pediatric patients with head trauma is to recognize and treat life-threatening conditions and to eliminate or minimize the role of secondary injury. Consult with a neurosurgeon. If child abuse is suspected, the mechanism of injury is unknown or unexplained, or the history is inconsistent, contact a child advocacy team or child protective services.
Resuscitation and treatment of life-threatening conditions
Treatment of children with severe head injury includes management of the following:
-
Airway
-
Cardiovascular and circulatory status
-
Intracranial pressure and cerebral perfusion
-
Bleeding
-
Seizure(s)
-
Temperature
-
Analgesia, sedation, and neuromuscular blockade
Surgery
Surgical intervention in pediatric patients with head trauma may be required and includes the following:
-
Surgical decompression
-
Craniotomy and surgical drainage
-
Surgical debridement and evacuation
-
Surgical elevation
-
Decompressive craniotomy with duraplasty
Pharmacotherapy
Pharmacologic therapy in patients with head trauma is directed at controlling intracranial pressure through the administration of sedatives and neuromuscular blockers, diuretics, and anticonvulsants.
The following medications are used in the management of pediatric head trauma:
-
Nondepolarizing neuromuscular blockers (eg, vecuronium)
-
Barbiturate anticonvulsants (eg, thiopental, pentobarbital, phenobarbital)
-
Benzodiazepine anxiolytics (eg, midazolam, lorazepam)
-
Diuretics (eg, furosemide, mannitol)
-
Anesthetics (eg, fentanyl, propofol)
-
Anticonvulsants (eg, phenytoin, fosphenytoin)
See Treatment and Medication for more detail.
Background
Trauma is a leading cause of death in children older than 1 year in the United States, with head trauma representing 80% or more of these injuries. In approximately 5% of head trauma cases, patients die at the site of the accident. Head trauma has a high emotional, psychosocial, and economic impact because these patients often have comparatively long hospital stays, and 5-10% require discharge to a long-term care facility. [3]
Most head injuries in children occur secondary to motor vehicle accidents, falls, assaults, recreational activities, and child abuse. The percentage of each contributing factor differs between studies, and the distribution varies according to age, group, and sex.
Patients with head trauma may experience one or a combination of primary injuries, including scalp injury, skull fracture, basilar skull fracture, concussion, contusion, intracranial hemorrhage, subarachnoid hemorrhage, epidural hematoma, subdural hematoma, intraventricular hemorrhage, penetrating injuries, and diffuse axonal injury.
The goal of medical care of patients with head trauma is to recognize and treat life-threatening conditions and to eliminate or minimize the role of secondary injury. Patients with severe head trauma are at increased risk of developing cerebral edema, respiratory failure, and herniation secondary to increased intracranial pressure (ICP).
Brain Trauma Foundation guidelines suggest that cardiopulmonary resuscitation should be the foundation upon which treatment of intracranial hypertension must be based and that in the absence of any obvious signs of increased ICP, no prophylactic treatment should be initiated; if instituted, prophylactic treatment has the potential to interfere with optimal resuscitation.
Anatomy
The anatomic characteristics of the child's brain render it more susceptible than the adult brain to certain types of injuries following head trauma. [4] The head is larger in proportion to the body surface area, and stability is dependent on the ligamentous rather than bony structures. Due to their smaller stature, pediatric pedestrians are at significant risk of direct brain injury from automobile crashes, as their heads may be the site of initial impact and will absorb a higher percentage of the forces applied. Although infants and young children may tolerate intracranial pressure (ICP) increases better because of open sutures, the presence of open fontanelles and sutures does not preclude the presence of elevated intracranial pressure; ICP monitoring may be important in this population, as well as in older patients with traumatic brain injury.
Pathophysiology
Both primary and secondary injuries are described in pediatric patients with head trauma, and the presence of these injuries affects outcome.
In a prospective, multicenter study of 43,399 pediatric patients treated for head injuries in US emergency rooms, Quayle et al found that the most common mechanisms of injury in the overall population were the following [5] :
-
Falls from any distance (27%)
-
Falls while standing, walking, or running (11%)
-
Collisions with a stationary object when walking or running (6%)
-
Motor vehicle crashes (9%)
-
Bicycle crashes (4%)
Falls were the most frequent cause of traumatic brain injury (TBI) for children under age 12, whereas assaults, motor vehicle accidents, and sports activities were the most frequent cause of injuries for adolescents. Overall, 98% of head injuries were classified as mild.
A large proportion of injuries caused by motor vehicle or bicycle crashes occurred when the child was not using a seat belt (36%) or a helmet (72%). [5] Among the 16% of patients in a motor vehicle crash who were diagnosed with a TBI, 52% were not using a seat belt. Of the 4% of bicycle crash patients with a TBI, 93% were not wearing a helmet.
Among the 37% of children who underwent cranial computed tomography (CT) scanning, TBIs were identified in 7%, and 3% had skull fractures without intracranial findings. The most common injury identified on CT scan was subdural hematoma, followed by subarachnoid hemorrhage and cerebral contusion.
Primary injuries
The primary injury occurs at the time of impact, either via direct injury to the brain parenchyma or via injury to the long white-matter tracts through acceleration-deceleration forces. [6]
Direct injury to the brain parenchyma occurs as the brain makes forceful contact with the bony protuberances of the calvaria or is penetrated by bony fragments or a foreign body. Impact on the brain at the time of the insult results in a coup injury, whereas contrecoup injury occurs as the brain is forced against the bony protuberances opposite the point of the impact.
Intracranial hemorrhage (ICH) may also result from shearing or laceration of vascular structures. Although exceptions occur, epidural hematomas are usually secondary to arterial injury, while subdural hematomas are usually secondary to venous injury. Because of the higher arterial blood pressure, epidural hematomas may enlarge very rapidly, while subdural hematomas generally develop more gradually. However, subdural hematomas are typically associated with underlying direct tissue injury, which is less common with epidural hematomas.
Acceleration-deceleration forces cause shearing of the long white-matter tracts, leading to axonal disruption and secondary cell death.
Secondary injuries
The secondary injury is represented by systemic and intracranial events that occur in response to the primary injury and further contribute to neuronal damage and cell death. [6]
The systemic events are hypotension, hypoxia, and hypercapnia and may occur either as a direct result of primary injury to the central nervous system (CNS) or as a consequence of associated injuries in a person with multiple traumas. Because of many factors (eg, higher brain metabolic activity, limited substrate availability, delay in seeking care), secondary brain injury commonly leads to greater morbidity than primary injury, while the reverse is true in adults.
The intracranial events are a series of inflammatory changes and pathophysiologic perturbations that occur immediately after the primary injury and continue over time. The nature of these events is poorly understood but has received greater attention due to the impact of secondary injury in pediatric traumatic brain injury.
Inflammatory changes are the result of a cascade of biomolecular alterations triggered by the initial insult, leading to microcirculatory disruption and neuronal disintegration. A series of factors such as free radicals, free iron, and excitatory neurotransmitters (glutamate, aspartate) are the result of these inflammatory events, and their presence contributes to negative outcomes. These pathophysiologic events include cerebral edema, increased ICP, hyperemia, and ischemia. Apoptotic neuronal cell death is more prevalent than necrotic neuronal cell death in pediatric patients, likely secondary to the role that apoptosis plays in the development of the pediatric brain.
Altered autoregulation of cerebral blood flow
Because the brain has minimal ability to store energy, it depends primarily on aerobic metabolism. The delivery of oxygen and metabolic substrate to the brain is maintained by a constant supply of blood, referred to as cerebral blood flow (CBF). CBF, defined as the amount of blood in transit through the brain at any given point in time, is estimated to be 50 mL/100 g/min in a healthy adult and is known to be much higher in children. However, the minimum amount necessary to prevent ischemic injury remains unknown.
CBF is influenced by mean arterial blood pressure (MAP), ICP, blood viscosity, metabolic products, and brain vessel diameter. CBF should not be confused with cerebral blood volume (CBV), which represents the amount of blood present in the brain vasculature. Because brain tissue and CSF volumes remain relatively stable, acute changes in CBV are mostly responsible for acute changes in ICP. CBV depends primarily on the diameter of intracranial vessels, so therapeutic interventions to reduce intracranial blood vessel diameter (vasoconstriction) are the most effective methods to acutely reduce elevated ICP. Hyperventilation, in the acute phase, decreases ICP by decreasing CBV via alkalosis-induced cerebral vasoconstriction.
The brain maintains constant blood flow through a mechanism known as autoregulation. This process occurs over a wide range of blood pressures through changes in cerebral resistance in response to fluctuations in MAP pressure. At a MAP of 60-150 mm Hg, CBF is maintained. At 60 mm Hg, the cerebral vasculature is maximally dilated. At 150 mm Hg, it is maximally constricted. (These are adult ranges; pediatric ranges are unknown but are likely age-dependent.) Fluctuations of MAP beyond either end of this range lead to alterations in CBF and contribute to ischemia or disruption of the blood-brain barrier.
Several mechanisms are known to affect autoregulation of CBF; they may be divided into the following categories:
-
Metabolic products
-
Arterial blood gas content
-
Myogenic factors
-
Neurogenic factors
-
Endothelium-dependent factors
The effects of these mechanisms are not fully known, and their mechanism of action is still under experimental investigation.
CBF is closely linked to cerebral metabolism. Although the mechanism of coupling is not clearly defined, it is thought to involve vasodilators released from neurons. Several factors have been implicated, such as adenosine and free radicals. Pathophysiologic states that are known to increase metabolic activity (eg, fever and seizure activity) lead to an increase in CBF.
CBF can be altered by changes in the partial pressure of oxygen or carbon dioxide. Alteration in the partial pressure of oxygen acts on the vascular smooth muscle through mechanisms that remain unclear. Hypoxia causes vasodilatation with significant increase in CBF. Increases in oxygen pressure result in dose-dependent vasoconstriction, although to a less pronounced degree than hypoxia-induced vasodilation.
Hypercarbia increases CBF up to 350% of normal, while hypocapnia produces a decrease in blood flow. The mechanism appears to involve alteration in tissue pH that leads to changes in arteriolar diameter. This mechanism is preserved even when autoregulation is lost. However, renal compensation for respiratory alkalosis causes tissue pH levels to normalize, restoring CBF, which limits the effectiveness of prolonged hyperventilation for control of elevated ICP.
The myogenic mechanism was long considered to be the most important in the autoregulation process. Changes in the actin-myosin complex were thought to lead to rapid changes in the vasculature diameter, thus affecting the CBF. It has now been shown that changes in the actin-myosin complex mostly cause dampening of arterial pulsation and have little direct effect on cerebral autoregulation.
The neurogenic mechanism is represented by the effect of the sympathetic system on the cerebral vasculature. The sympathetic nervous system shifts autoregulation toward higher pressures, whereas sympathetic blockade shifts it downward.
Studies have identified nitric oxide (NO) as one of the factors affecting cerebral autoregulation; it does so by producing relaxation of cerebral vessels. NO is present in several conditions, such as ischemia, hypoxia, and stroke. It is generated by different cells at rest but also under direct stimulation by factors such as cytokines.
Alterations in CBF during periods of hyperoxia, hypoxia, hypercarbia, and hypocarbia occur due to changes in local NO production. Vasodilation from somatosensory stimulation occurs through changes in neurogenic NO production, and impaired vasodilation associated with endothelial dysfunction appears to be due (at least in part) to the production of reactive oxygen species and reduced NO bioavailability. [7]
TBI may lead to loss of autoregulation through alteration of any of these mechanisms. One study found that mild TBIs are more likely than orthopedic injuries to cause transient or persistent increases in postconcussive symptoms during the first year after injury. [8] These mechanisms represent the foundation on which the medical management of increased ICP and cerebral perfusion pressure (CPP) is based in patients with TBI.
Etiology
Most head injuries occur secondary to motor vehicle accidents, falls, assaults, recreational activities, and child abuse. The percentage of each contributing factor differs between studies, and the distribution varies according to age, group, and sex. A few factors (eg, seizure disorder, attention deficit disorder, and alcohol and drug use) are known to enhance the vulnerability of the child or adolescent with respect to this type of trauma. Infants and young children are more vulnerable to abuse because of their dependency on adults and their inability to defend themselves.
Motor vehicle accidents account for 27-37% of all pediatric head injuries. In most cases involving children younger than 15 years, the victim is a pedestrian or a bicyclist; pedestrian accidents in children aged 5-9 years are the second most frequent cause of death. Young adults aged 15-19 years tend to be passengers involved in motor vehicle accidents, and alcohol is often a contributing factor.
Falls are the most common cause of injury and the leading cause of traumatic brain injury in children aged 0-4 years. [9]
Recreational activities have a seasonal distribution, with peaks during spring and summer months. They represent 21% of all pediatric brain injuries, with the largest vulnerable group aged 10-14 years.
Assault accounts for 10% of all pediatric brain injuries, and firearm-related injuries account for 2%. Child abuse has been identified as the cause of brain injury in 24% of pediatric patients younger than 2 years; it was suspected in another 32%. The risk of abusive head trauma (AHT) appears to decrease with increasing maternal age and increasing gestational age at birth. [10] Factors that appear to associated with AHT include lack of or poor prenatal care, maternal single status, documented social concerns, as well as missing maternal prenatal data for antenatal care, partner status, social concerns, and substance abuse. [10]
In children younger than 3 years, the depth of head injury can be successfully used to determine injury causes and mechanisms. [11]
Epidemiology
In the United States, the estimated annual incidence of pediatric head injury is approximately 200 per 100,000 population. This number includes all head injuries that result in hospitalization, death, or both in persons aged 0-19 years.
Age-, sex-, and race-related demographics
The distribution of head trauma is relatively stable throughout childhood. An increase in the incidence of head trauma was identified in two age groups. At approximately age 15 years, a dramatic increase occurs, mainly in males, related to their involvement in sports and driving activities. Infants younger than 1 year also have an elevated incidence of head trauma, which is attributed to falls and child abuse. [12]
Males are twice as likely to sustain head injuries as females and have four times the risk of fatal trauma. Black adolescent males account for most of the firearms-related CNS injuries in the pediatric population.
Prognosis
The overall outcome for children with head injuries is better than that for adults with the same injury scores. [13, 14, 15] Time to maximum recovery after injury is longer in children (months to years) than in adults (typically about 6 months). Patients with multiple organ injuries, including head trauma, generally have a far worse outcome than those with head injury alone.
Outcome assessment based on the Pediatric Glasgow Coma Scale (PGCS) can be used as an early predictor, but this scale has limitations regarding long-term outcome. Mechanism of injury appears to be a significant predictor of clinical and functional outcomes at discharge for equivalently injured patients. [16]
According to the National Center for Health Statistics, mortality from head trauma is 29% in the pediatric population. [17] These data are based on death certificate information, and 29% could be an underestimation of the actual rate. Data reported by studies in trauma centers show that head injury represents 75-97% of pediatric trauma deaths.
Patients with severe head trauma and a PGCS score of 3-5 have a mortality of 6-35%; this figure increases to 50-60% for those with a PGCS score of 3. Of those with a PGCS score of 3-5 who survive, 90% require rehabilitation after hospital discharge, and most of them eventually return to school.
Risk factors associated with increased mortality for children suffering from abusive, non-accidental head trauma include, not surprisingly, low GCS (3 or 4-5), retinal hemorrhage, intraparenchymal hemorrhage and cerebral edema. Surprisingly, presence of a chronic subdural hematoma is associated with survival. [18]
Short-term memory problems and delayed response times are reported in 10-20% of children with moderate-to-severe head injury (PGCS score, 6-8), especially if the coma lasts longer than 3 weeks. Patients with a PGCS score of 6-8 are most likely to regain consciousness within 3 weeks, but one-third are left with focal neurologic deficits and learning difficulties, especially when coma persists beyond 3 weeks. [19]
More than half of children with a PGCS score of 3-5 have permanent neurologic deficits. Patients with a PGCS score of 3 have particularly poor neurologic outcomes.
A study that primarily investigated adult TBI patients revealed that diabetic TBI victims had an unfavorable mortality odds ratio (1.5), with the trend being worse for insulin-dependent diabetes patients than for noninsulin-dependent ones. [20] The study raises the question of whether insulin deficiency may contribute to TBI mortality, either along with or independent of glucose changes after TBI.
At the very least, this study points out that meticulous insulin and glucose management of diabetic TBI patients, matching insulin to carbohydrate administration as needed, may help reduce TBI mortality in this population. Care must still be taken not to induce hypoglycemic events in these critically ill patients while trying to avoid potentially harmful insulin deficiency. [20]
Complications
Long-term complications of head injury are common in children, and they are related to both primary and secondary injuries. [21, 22]
Seizures are more commonly observed with contusions (more so with subdural hematoma than with epidural hematoma), depressed skull fracture, and severe head injury (PGCS score, 3-5).
Leptomeningeal cyst or growing fracture represents extrusion of leptomeninges and brain tissue through a dural defect. Meningitis may develop secondary to basilar skull fracture, [23] penetrating injury, or other injuries that cause disruption of the dura mater.
Cranial nerve injury may develop secondary to basilar skull fracture, mass effect, or herniation. Oculomotor palsy is due to injury of cranial nerves VI, III, or IV. Trauma to nerve VII leads to facial nerve palsy. Hearing loss may occur because of injury of cranial nerve VIII.
Posttraumatic syndrome may develop after mild-to-moderate head trauma and consists of irritability, inability to concentrate, nervousness, and occasionally behavioral or cognitive impairment. Postconcussion symptoms may be more prevalent that previously reported, involve neurologic and nonneurologic components, and require attention to physical, cognitive, and emotional symptoms (especially for patients with persistent symptoms). [24]
Cortical blindness, described as an acute loss of vision after head trauma, usually resolves spontaneously within 24 hours. Several mechanisms have been implicated, including acute cerebral edema and transient vasospasm. Cortical blindness is now considered to result from minor transient alterations in brain function triggered by the traumatic event.
Trauma-induced migraine may begin from minutes to hours after the injury and may last from hours to days. Beta-blockers are the drugs of choice for this complication.
Hydrocephalus results from either an obstruction caused by an intraventricular hemorrhage or decreased reabsorption of CSF due to proteinaceous obstruction of the arachnoid villi.
Neurogenic pulmonary edema is thought to be due to medullary ischemia that leads to increased sympathetic tone with subsequent increase in pulmonary vascular pressure and a shift in blood distribution from the systemic to the pulmonary circulation.
Pulmonary infections are often present in patients with head trauma because of either an initial aspiration process or prolonged mechanical ventilation.
Patient Education
Children should be referred for early intervention and rehabilitation services. Both children and their families should be referred for psychosocial counseling. Children should be referred for neuropsychiatric testing, especially when learning difficulties are present.
Unfortunately, postnatal parental intervention does not appear to reduce the incidence of abusive head trauma (AHT) in infants and young children. In a study that compared AHT hospitalization rates in Pennsylvania before and during such intervention to that of five other states without universal parental AHT education over the same period (2003-2013), Pennsylvania incidence rate ratios for AHT hospitalizations increased 2.5% per 100,000 children aged 0-23 months, a nonsignificant difference from the 0.4% aggregate changes seen in the other five states. [25] The interventions included a brochure, an 8-minute video regarding infant crying and AHT, questions/answers with a nurse, and a signed participation commitment statement affirmation; however, only a little over one fifth (20.6%) of parents saw the brochure and video, and 5.7% had exposure to the entire intervention—out of 16,111 parents who completed the postnatal survey and 1,180,291 parents who signed the commitment statement. Of the 143 respondents who subsequently completed the 7-month survey, over three quarters (76.2%) self-reported gains in parental knowledge. [25]
-
Pediatric Head Trauma. Epidural hematoma with midline shift.
-
Pediatric Head Trauma. Subdural hematoma.
-
Pediatric Head Trauma. Intraventricular hemorrhage.
-
Pediatric Head Trauma. Epidural hematoma with acute neurologic deterioration.