Practice Essentials
Cyclospora cayetanensis is an intestinal coccidia that infects the gastrointestinal (GI) tract of both immunocompetent and immunocompromised hosts. This organism was first described in human feces in 1979. Since the advent of the acquired immunodeficiency syndrome (AIDS) epidemic, C cayetanensis has been increasingly recognized as an enteric pathogen. [1]
Cyclospora species are ubiquitous and infect a variety of animals, birds and reptiles. Humans are the only known hosts of C cayetanensis.
Causes of cyclosporiasis include consumption of infected water or produce or exposure to the organism during travel to countries where it is endemic. Immunosuppression is a risk factor for chronic cyclosporiasis in endemic areas or among travelers to these areas. [2]
Discuss proper food and water precautions needed with patients who are traveling to endemic regions to prevent this and other infections transmitted through the fecal-oral route.
Pathophysiology
Cyclospora species are variably acid-fast, round-to-ovoid organisms that measure 8-10 µm in diameter. Cyclospora species exogenously sporulate and have 2 sporocysts per oocyst. Transmission follows ingestion of oocysts in fecally contaminated water or produce. Direct person-to-person transmission is considered unlikely because the oocysts are not infectious when excreted; the oocysts undergo sporulation outside the human host before becoming infective. The median incubation period is 1 week, during which time the organism invades enterocytes of the small intestine.
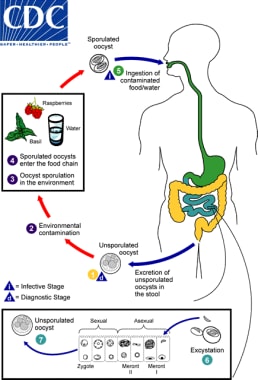 Life cycle of Cyclospora. (1) When freshly passed in stools, the oocyst is not infective; thus, direct fecal-oral transmission cannot occur and this differentiates Cyclospora from another important coccidian parasite, Cryptosporidium. (2) In the environment, sporulation occurs after days or weeks at temperatures between 22°C to 32°C, resulting in division of the sporont into two sporocysts, each containing two elongate sporozoites (3). Fresh produce and water can serve as vehicles for transmission (4) and the sporulated oocysts are then ingested in contaminated food or water (5). The oocysts exist in the gastrointestinal tract, freeing the sporozoites which invade the epithelial cells of the small intestine (6). Inside the cells, they undergo asexual multiplication and sexual development to mature into oocysts which will be shed in stools (7). The potential mechanisms of contamination of food and water are still under investigation. Courtesy of the CDC (http://phil.cdc.gov/phil/home.asp).
Life cycle of Cyclospora. (1) When freshly passed in stools, the oocyst is not infective; thus, direct fecal-oral transmission cannot occur and this differentiates Cyclospora from another important coccidian parasite, Cryptosporidium. (2) In the environment, sporulation occurs after days or weeks at temperatures between 22°C to 32°C, resulting in division of the sporont into two sporocysts, each containing two elongate sporozoites (3). Fresh produce and water can serve as vehicles for transmission (4) and the sporulated oocysts are then ingested in contaminated food or water (5). The oocysts exist in the gastrointestinal tract, freeing the sporozoites which invade the epithelial cells of the small intestine (6). Inside the cells, they undergo asexual multiplication and sexual development to mature into oocysts which will be shed in stools (7). The potential mechanisms of contamination of food and water are still under investigation. Courtesy of the CDC (http://phil.cdc.gov/phil/home.asp).
Cyclospora species are characterized by an anterior polar complex that allows penetration into host cells, but the life cycle of the parasite and the mechanisms by which it interacts with human host target cells to cause disease are poorly understood.
Epidemiology
United States statistics
The prevalence of infection in endemic areas is estimated at 2% to 18% (including asymptomatic and symptomatic infections) and for developed countries prevalence is estimated at 0.1% to 0.5%). [3] Cases in the developed countries are usually associated with outbreaks from recognized contaminated food and water.
The first known outbreak of cyclosporiasis in the United States occurred in 1990 in a Chicago hospital's physicians' dormitory and was attributed to an infected water source. [4, 5] Since then, multiple US epidemics of cyclosporiasis have been reported and have been attributed to infected Guatemalan raspberries [6, 7] basil, mesclun lettuce, [8, 9, 10, 11] imported Thai basil, [12] and snow peas. [13] Outbreaks in 2013 were reported in Texas related to infected cilantro and cases in Iowa and Nebraska related to contaminated salad mix. [14] Cyclosporiasis has also been reported as a cause of foodborne diarrhea in outbreaks due to domestic contamination from vegetable trays and precut salad mixes and produce such as romaine lettuce and green onions. [15, 16, 17] The Centers for Disease Control and Prevention (CDC) monitors the occurrence of cyclosporiasis in the United States and is a notifiable disease.
In August 2014, CDC was notified of 304 ill persons with confirmed Cyclospora infection in 2014. About 64% of cases were reported from Texas and 64% were reported in July 2014. Preliminary investigation linked cases in Texas with cilantro from Mexico; however, none of the cases outside Texas were linked to cilantro.
In August 2017, the CDC issued a Health Alert Network advisory following an increase in reported cases of cyclosporiasis. The advisory guides providers to consider a diagnosis of cyclosporiasis in patients who experience prolonged or remitting-relapsing diarrhea. Between May 1, 2017, and August 2, 2017, 206 cases of Cyclospora infections were reported to the CDC from 27 states. Eighteen cases required hospitalization; however, no deaths were reported. [18]
A decrease in the incidence of cyclosporiasis was reported in the United States (34 states reporting infections) from May to early August 2020 (1241 cases vs 2408 cases during the same period in 2019). US cases have typically increased in recent years; thus, this decrease may reflect the impact of the COVID-19 pandemic. [15]
International statistics
Worldwide, most fecal isolates have been obtained from residents of developing countries or from travelers returning from these regions. [19, 20] Cyclosporiasis is endemic in Haiti, Nepal, and Peru, with a strong seasonal predominance during rainy spring and summer months. Cyclosporiasis has also been reported in travelers returning from Mexico, Southeast Asia, Puerto Rico, Indonesia, [21] Morocco, Pakistan, and India. Cases have also been recognized in Kuwait [22] and China. [23]
Race-, sex-, and age-related demographics
No racial predilection has been reported.
Cyclosporiasis equally affects both genders.
Persons of all ages can be affected, although cyclosporiasis primarily affects children in developing countries where the disease is endemic.
Prognosis
Because infection is self-limited in the immunocompetent host, full recovery is expected. With treatment and prophylaxis to prevent relapses, infection in the immunocompromised host can generally be controlled.
Morbidity/mortality
Death is exceptionally rare. Very little morbidity results from this infection, except in persons with underlying immunosuppression, in whom chronic diarrhea can develop, resulting in weight loss and malabsorption.
-
Life cycle of Cyclospora. (1) When freshly passed in stools, the oocyst is not infective; thus, direct fecal-oral transmission cannot occur and this differentiates Cyclospora from another important coccidian parasite, Cryptosporidium. (2) In the environment, sporulation occurs after days or weeks at temperatures between 22°C to 32°C, resulting in division of the sporont into two sporocysts, each containing two elongate sporozoites (3). Fresh produce and water can serve as vehicles for transmission (4) and the sporulated oocysts are then ingested in contaminated food or water (5). The oocysts exist in the gastrointestinal tract, freeing the sporozoites which invade the epithelial cells of the small intestine (6). Inside the cells, they undergo asexual multiplication and sexual development to mature into oocysts which will be shed in stools (7). The potential mechanisms of contamination of food and water are still under investigation. Courtesy of the CDC (http://phil.cdc.gov/phil/home.asp).
-
Oocysts of C cayetanensis stained with modified acid-fast stain. Note the variability of staining in the four oocysts. Courtesy of the CDC (http://phil.cdc.gov/phil/home.asp).
-
Oocyst of C cayetanensis viewed under UV microscopy. Courtesy of the CDC (http://phil.cdc.gov/phil/home.asp).








