Overview
Background
Many early reports described inflammation in and around the appendix, but it was not until 1886 that Reginald Fitz provided an accurate description of the disease process. Fitz was the first to elucidate the clinical history, physical findings, and pathology and was also the first to advocate appendectomy as the cure.
In 1887, Thomas Morton performed the first successful appendectomy in the United States. In 1889, Nicholas Senn was one of the first surgeons to diagnose acute appendicitis correctly, perform an appendectomy, have the patient recover, and report the case. In this same year, Charles McBurney described the clinical findings of acute appendicitis, including the point of maximal tenderness, which still bears his name.
Indications
Appendectomy is indicated once the diagnosis of appendicitis or perforated appendicitis has been made. An exception would be a well-localized appendiceal perforation in a child who is clinically well. This presentation allows initial nonoperative treatment with definitive treatment months later with an interval appendectomy.
Contraindications
Almost no contraindications exist to the surgical treatment of appendicitis. It should be kept in mind, however, that certain patients with unrecognized perforated appendicitis may present in a state of florid septic shock. In these patients (and even in those who are not so ill), one must ensure that the patient receives adequate fluid resuscitation and appropriate broad-spectrum antibiotics before proceeding to the operating room.
Technical considerations
Considerations to be addressed in planning surgical therapy include the choice between open and laparoscopic appendectomy and the choice between emergency appendectomy and initial conservative management followed by appendectomy some time later.
Procedural planning
Open versus laparoscopic appendectomy
Laparoscopic appendectomy is increasingly being favored. Potential advantages of laparoscopic appendectomy include reduced postoperative pain, a lower wound infection rate, a shorter length of stay (–0.6 days), and a faster return to daily activities, including school and gym. After an appropriate learning curve, the difference in operating time between open appendectomy and laparoscopic appendectomy has been shown to be of no statistical significance.
Another advantage of laparoscopic appendectomy is that it affords the surgeon the ability to evaluate the entire abdomen, which can be useful or diagnostic with adolescent female patients, in whom gynecologic conditions can often imitate appendicitis. Laparoscopic appendectomy is also useful for patients in whom the diagnosis is in question and patients who are obese.
A large retrospective study showed that the technique of appendectomy, open versus laparoscopic, did not appear to affect the incidence of intra-abdominal abscesses. [1]
Emergency versus interval appendectomy
The ideal management approach for pediatric patients with a perforated appendix remains controversial. In such cases, the choice is between appendectomy performed emergently and—if the child is clinically well—initial conservative management, with appendectomy at a later date when the acute inflammation has subsided. This delayed surgical treatment is referred to as interval appendectomy and is generally performed 8-12 weeks after the initial episode.
Advocates of interval appendectomy point to the relatively high rate of recurrent appendicitis without this procedure, the possibility of missed pathologic diagnoses, [2] and the low complication rates associated with this approach. Opponents argue that the rate of recurrent disease is insignificant, and they cite concerns about the morbidity associated with interval appendectomy.
Some authors have advocated interval appendectomy only if a fecalith is present on imaging studies, on the grounds that such a finding significantly increases the risk of recurrent disease. Ein et al noted a 72% rate of recurrent appendicitis in patients with a fecalith. [3]
When a patient undergoes interval appendectomy, the laparoscopic approach is preferred because it enables the surgeon to visualize a wider area of the abdomen, to lyse any postinflammatory adhesions that may be present, and to avoid the need for extending an open incision in case of abnormal anatomy.
The complication rate for interval appendectomy is reported to be 12-23%, which is less than the 26% complication rate associated with emergent appendectomy in perforated appendicitis. These numbers are based on relatively small studies with different protocols, which limits their usefulness for direct comparison. However, a large meta-analysis did show a significantly greater morbidity for immediate surgery than for conservative treatment with interval appendectomy (35.6% vs 13.5%). [4]
A study by Whyte et al suggested that interval laparoscopic appendectomy may be performed as an outpatient procedure. [5] In this study, 12 of 24 patients were discharged the evening of the procedure, and of the patients who were admitted, 9 stayed only 1 night. This encouraging report notwithstanding, laparoscopic appendectomy has well-known complications that should not be forgotten, including wound infection, abscess, sepsis, and ileus.
In a nonblinded randomized comparison of early with interval appendectomy in 131 children with perforated appendicitis, Blakely et al found that early appendectomy significantly reduced the time away from normal activities. [6] The overall adverse event rate after early appendectomy was significantly lower than that after interval appendectomy. A prospective randomized study by the same author noted that hospital charges and costs were significantly lower for early appendectomy compared with interval appendectomy. [7]
This area is a popular topic of current research. To date, however, no large-scale prospective randomized trials have compared continued conservative management with interval laparoscopic appendectomy for perforated appendicitis.
A review of the pediatric literature on the use of interval appendectomy after successful nonoperative treatment of appendiceal mass concluded that despite the lack of prospective studies comparing routine interval appendectomy with nonoperative treatment without interval appendectomy, available data suggest that 80% of children with an appendiceal mass may not need interval appendectomy. [8] A prospective study to evaluate the natural history of this condition against the morbidity and costs of interval appendectomy is warranted.
Periprocedural Care
Preprocedural evaluation
In some equivocal cases of pediatric appendicitis, preoperative imaging may be indicated (eg, to confirm the diagnosis or assess the need for operative versus nonoperative treatment). Modalities include computed tomography (CT), ultrasonography, and radiography (see the images below).
A study by Bachur et al that reviewed trends in the use of ultrasonography and CT for children with appendicitis reported that among children with suspected appendicitis, the use of ultrasonography has increased substantially as the use of CT has declined due to campaigns against ionizing radiation exposure. Despite the increased reliance on the diagnostically inferior ultrasonography, important condition-specific quality measures, including the frequency of appendiceal perforation and ED revisits, remained stable, and the proportion of negative appendectomy declined slightly. [9, 10, 11]
 CT scan depicting distended tubular structure descending into pelvis and containing round calcification (ie, appendicolith).
CT scan depicting distended tubular structure descending into pelvis and containing round calcification (ie, appendicolith).
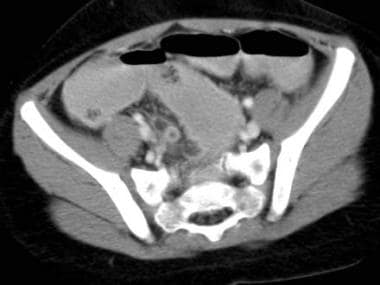 CT scan revealing enhancing tubular structure descending into pelvis. Periappendiceal inflammation and streaking (so-called dirty fat) is noted surrounding appendix.
CT scan revealing enhancing tubular structure descending into pelvis. Periappendiceal inflammation and streaking (so-called dirty fat) is noted surrounding appendix.
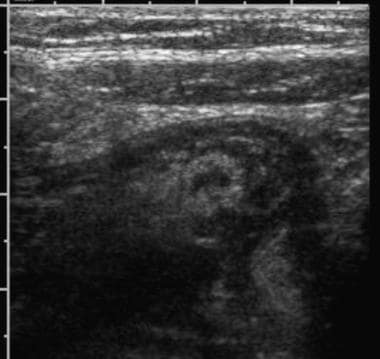 Ultrasonographic examination of right lower quadrant reveals noncompressible tubular structure larger than 6 mm (shown in cross-section). Discomfort was noted as probe was depressed over this structure. Small amount of free fluid is also noted surrounding appendix.
Ultrasonographic examination of right lower quadrant reveals noncompressible tubular structure larger than 6 mm (shown in cross-section). Discomfort was noted as probe was depressed over this structure. Small amount of free fluid is also noted surrounding appendix.
 Ultrasonographic examination of right lower quadrant reveals noncompressible tubular structure larger than 6 mm (shown in cross-section). Discomfort was noted as probe was depressed over this structure. Small amount of free fluid is also noted surrounding appendix.
Ultrasonographic examination of right lower quadrant reveals noncompressible tubular structure larger than 6 mm (shown in cross-section). Discomfort was noted as probe was depressed over this structure. Small amount of free fluid is also noted surrounding appendix.
Patient preparation
Before incision, patients should be adequately resuscitated with fluids and should receive preoperative prophylactic antibiotics.
If simple appendicitis is suspected, a single agent (eg, a second-generation cephalosporin such as cefoxitin) or an extended-spectrum penicillin combination (eg, ampicillin-sulbactam) is adequate. In fact, the only aspect of antibiotic treatment of appendicitis in the pediatric population for which ample class I and class II data are available is the use of perioperative antibiotics in patients with acute, nonperforated appendicitis. [12]
If a perforated appendix is suspected, triple antibiotic therapy may be administered; however, many studies have determined that this approach offers no advantages over single-agent antibiotic therapy, as long as adequate gram-negative and anaerobic coverage is provided. [12] A single-agent approach may also offer improvements in length of stay, pharmacy charges, and hospital charges and is clearly superior with regard to ease of administration by nurses. [13]
The procedure is done with the patient supine and under general anesthesia.
Monitoring and follow-up
The postoperative course is dictated by the status of the appendix at operation. In the case of uncomplicated acute appendicitis, it should be possible to discharge the patient 24-36 hours after the operation. Requirements for discharge include lack of fever, adequate pain control on oral analgesics, and sufficient oral intake to maintain hydration.
Perforated appendicitis necessitates a longer hospital stay for intravenous (IV) antibiotic treatment. These children are usually treated with triple antibiotics. Criteria for adequate treatment vary. The author requires patients to be afebrile for 48 hours before being discharged home. The relevant criteria for acute appendicitis must also be met, including a white blood cell (WBC) count within the reference range.
Patients should return for follow-up about 1-2 weeks after discharge. The wound should be examined for evidence of inflammation, and the patient should be checked for fever. This visit gives the surgeon an excellent opportunity to review the pathology report with the patient and ensure that nothing unusual (eg, a carcinoid tumor) was found.
Technique
Approach considerations
Once the patient has been placed under general anesthesia, the abdomen should be reexamined. Because voluntary guarding has ceased to be an issue, it is sometimes possible to palpate an abdominal mass at this time.
Two approaches to appendectomy are acceptable: open and laparoscopic. Which operation is performed in a given instance depends on the individual surgeon's preference. To date, prospective randomized studies have not determined that one approach is superior to the other. [14, 15]
Open appendectomy
A transverse right lower quadrant incision is made, usually at the McBurney point. If an abdominal mass was palpated after the induction of anesthesia, the exact location of the incision can be shifted so that it is centered over the mass. The incision is made lateral to the rectus abdominis but can be extended medially should greater exposure be required.
The external oblique aponeurosis is sharply divided along the direction of its fibers, and the underlying internal oblique and transversalis muscles are split with Kelly clamps. The peritoneum is divided transversely, and the peritoneal cavity is entered.
If the appendix is visualized, it can be easily delivered into the wound. If the appendix is not immediately apparent, it can be located by identifying the taeniae coli and tracing these muscular bands distally. This path leads directly into the cecum and then the appendix.
If a normal-appearing appendix is identified, other pathologic conditions should be sought. The distal ileum should be examined for evidence of creeping fat (characteristic of Crohn disease). The right lower quadrant should be inspected for suspicious lymph nodes; if any such nodes are present, 1 or more samples should be obtained for pathologic review. The ileum should be identified and followed back at least 2 ft to identify a potential Meckel diverticulum. If no other pathology is observed after these maneuvers, the appendix is removed in the standard fashion.
Once the appendix is delivered into the wound, the mesentery is divided between ligatures. The base of the appendix is then crushed with a clamp and ligated at this site. The exposed mucosa can then be cauterized with the scalpel blade just used to divide the appendix. The stump can be left as is or can be inverted with a pursestring suture or Z-stitch. The wound is then usually closed in layers with absorbable sutures.
For a perforated appendix, the approach is identical, though the incision used may be larger. The goals are to remove the gangrenous appendix and any gross contamination contained within the peritoneal cavity. Liters of irrigation fluid may be used if contamination is severe. The wound may be left open or may be closed with interrupted subcutaneous sutures, with wicks of gauze left between the sutures. The wicks are removed 3-5 days after the operation.
Laparoscopic appendectomy
Before placement of the initial trocar, the stomach and bladder are decompressed. Either a closed or an open insertion technique through the base of the umbilicus may be safely used, allowing the placement of a 5-mm or 12-mm port through this site without compromise of cosmesis. The abdomen is insufflated to 10-15 mm Hg, depending on the size of the child.
First, the camera port is placed in the umbilicus. Then, under direct visualization, two 5 mm ports are placed. Depending on the surgeon's preference, one port may be placed in the right lower quadrant and the other in the left lower quadrant, or both ports may be placed in the left lower quadrant.
The cecum and appendix are mobilized in a lateral-to-medial direction. The appendix is grasped, and an opening is made in its mesentery near the base of the appendix. An endoscopic stapler or detachable snare loop is used to divide the base of the appendix, and the mesoappendix is controlled with vascular staples or an electrocautery. The appendix is then removed through the umbilical port; if the appendix is enlarged or friable, this may necessitate the aid of a laparoscopic specimen collection bag.
As is the case with open appendectomy, irrigation may be used. However, a prospective randomized trial showed that there was no advantage to irrigation of the peritoneal cavity over suction alone during laparoscopic appendectomy for perforated appendicitis. [16]
Laparoscopic techniques for appendectomy in children have been developed that make use of a single-site approach. [17] Single-incision multiport laparoscopic (SIMPL) appendectomy in children and adolescents appears to be feasible.
Multiple prospective, randomized studies comparing single-incision versus standard 3-port laparoscopic appendectomy have shown no advantages of one technique over the other with respect to complications, [18, 19, 20] but they differ in their cosmetic satisfaction scores. [19, 21] Longer operating times were noted in the single-incision cohort. [18, 22] Increased postoperative pain in the single-incision group was noted by some authors, [21, 22] whereas some reported no differences in postoperative pain scores [19] between the groups, and yet others noted less pain in the single-incision group. [18]
Complications of appendectomy
Postoperative complications are typically infectious. The most common complication is wound infection, especially with a perforated appendix. Fever and wound erythema are classic hallmarks. The wound should be opened to allow drainage of the pus. Healing by second intention is the rule. Oral antibiotics are used on an outpatient basis for mild infections, whereas intravenous (IV) antibiotics and hospitalization are reserved for patients who have evidence of cellulitis, sepsis, or both.
Intra-abdominal abscesses, most commonly pelvic, occur postoperatively in about 5% of cases of perforated appendicitis. If the abscess is unilocular, it may be drained with percutaneous techniques under the guidance of computed tomography (CT). If multiple intraloop abscesses are present or if the unilocular abscess is not accessible with drainage techniques, operative exploration and drainage are required. Short-term complications of intra-abdominal abscesses include sepsis, ileus, and even bowel obstruction.
Postoperative small bowel obstruction is a rare complication of laparoscopic appendectomy in children. Overman et al found that staples used during the appendectomy were often the cause of the obstruction. [23]
A complication rarely observed in the current era is pylephlebitis, or septic portal vein thrombosis. This condition is typically due to Escherichia coli from an unrecognized and untreated intra-abdominal septic source. Patients have fevers, jaundice, and eventually hepatic abscesses. The diagnosis is made by means of CT, which reveals gas and thrombus within the portal vein. Prompt treatment involves eradication of the intra-abdominal source of infection, as well as the administration of broad-spectrum antibiotics.
Another complication that receives significant attention is the possibility of infertility in females who have had perforated appendicitis. Many investigators have studied this group of patients. Urbach et al demonstrated in a case-control study that neither acute appendicitis nor perforation of the appendix was a statistically significant factor for tubal infertility. [24] This finding has been confirmed by many other investigators in multiple countries, and it is now clear that perforated appendicitis in females does not lead to tubal infertility. [25, 26]
-
CT scan depicting distended tubular structure descending into pelvis and containing round calcification (ie, appendicolith).
-
CT scan revealing enhancing tubular structure descending into pelvis. Periappendiceal inflammation and streaking (so-called dirty fat) is noted surrounding appendix.
-
Ultrasonographic examination of right lower quadrant reveals noncompressible tubular structure larger than 6 mm (shown in cross-section). Discomfort was noted as probe was depressed over this structure. Small amount of free fluid is also noted surrounding appendix.
-
Ultrasonographic examination of right lower quadrant reveals noncompressible tubular structure larger than 6 mm (shown in cross-section). Discomfort was noted as probe was depressed over this structure. Small amount of free fluid is also noted surrounding appendix.
-
Perforated appendicitis.








