Practice Essentials
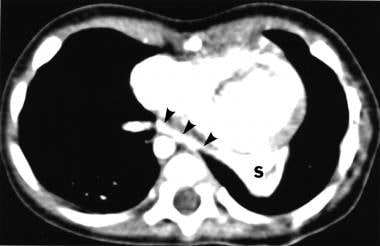
Pulmonary sequestration is a cystic or solid mass composed of nonfunctioning primitive tissue that does not communicate with the tracheobronchial tree and has anomalous systemic blood supply. It is a type of congenital thoracic malformation. It may present as a lung infection on physical examination and chest imaging. Its blood supply is from the systemic circulation rather than the pulmonary circulation. (See the image below.) Multiple feeding vessels may be present in 15-20% of cases. The two forms of pulmonary sequestration are intrapulmonary, which is surrounded by normal lung tissue, and extrapulmonary, which has its own pleural investment. Other congenital malformations may be present. [1]
Signs and symptoms of pulmonary sequestration
Examination of the lungs may reveal signs consistent with consolidation. Occasionally, patients may have a systolic bruit or continuous murmur over the affected area.
Although an intrapulmonary sequestration is usually diagnosed later in childhood or adolescence, symptoms may begin early in childhood with multiple episodes of pneumonia. A chronic or recurrent cough is common.
Many patients with extrapulmonary sequestration present in infancy with respiratory distress and chronic cough.
See Presentation for more detail.
Diagnosis of pulmonary sequestration
Imaging studies
Chest radiography is indicated. Computed tomography (CT) scanning with contrast and magnetic resonance angiography (MRA) are also highly useful in revealing the presence of systemic arteries, which are the major diagnostic feature of pulmonary sequestration. Real-time ultrasonography and Doppler imaging are reliable methods of demonstrating the systemic origin of blood supply as well.
See Workup for more detail.
Management of pulmonary sequestration
Management of an asymptomatic pulmonary sequestration with no connection to the surrounding lung is controversial; however, most references advocate resection of these lesions because of the likelihood of recurrent lung infection, the need for larger resection if the sequestration becomes chronically infected, and the possibility of hemorrhage from arteriovenous anastomoses.
See Treatment for more detail.
Pathophysiology
Pulmonary sequestration is believed to result from abnormal diverticulation of foregut and aberrant lung buds. [2]
The most frequently supported theory of sequestration formation involves an accessory lung bud that develops from the ventral aspect of the primitive foregut. The pluripotential tissue from this additional lung bud migrates in a caudal direction with the normally developing lung. It receives its blood supply from vessels that connect to the aorta and cover the primitive foregut. These attachments to the aorta remain to form the systemic arterial supply of the sequestration. [3]
Early embryologic development of the accessory lung bud results in formation of the sequestration within normal lung tissue. The sequestration is encased within the same pleural covering. This is the intrapulmonary variant. In contrast, later development of the accessory lung bud results in the extrapulmonary type that may give rise to communication with the GI tract. Both types of sequestration usually have arterial supply from the thoracic or abdominal aorta. Rarely, the celiac axis, internal mammary, subclavian, or renal artery may be involved. [4]
Intrapulmonary sequestration occurs within the visceral pleura of normal lung tissue. Usually, no communication with the tracheobronchial tree occurs. The most common location is in the posterior basal segment, and nearly two thirds of pulmonary sequestrations appear in the left lung. Venous drainage is usually via the pulmonary veins. [5] Foregut communication is very rare, and associated anomalies are uncommon.
Extrapulmonary sequestration is completely enclosed in its own pleural sac. It may occur above, within, or below the diaphragm, and nearly all appear on the left side. No communication with the tracheobronchial tree occurs. Venous drainage is usually via the systemic venous system. Foregut communication and associated anomalies, such as diaphragmatic hernia, are more common.
Epidemiology
United States statistics
Pulmonary sequestration represents approximately 6% of all congenital pulmonary malformations. [6] Intrapulmonary sequestrations are the most common form, and 60% of these are found in the posterior basal segment of the left lower lobe. Overall, 98% occur in the lower lobes. Bilateral involvement is uncommon. About 10% of cases may be associated with other congenital anomalies. [7] A case of intrapulmonary sequestration associated with a bronchogenic cyst has been reported. [8]
Extrapulmonary sequestrations occur on the left in 95% of cases. Of these, 75% are found in the costophrenic sulcus on the left side. They may also be found in the mediastinum, pericardium, and within or below the diaphragm. They are associated with other congenital malformations in more than 50% of cases, such as congenital diaphragmatic hernias, congenital pulmonary airway malformation (CPAM) type II (hybrid lesions), and congenital heart disease. [9]
Sex- and age-related demographics
In the extrapulmonary form, males are affected approximately 4 times more often than females. Incidence is equal in males and females in the intrapulmonary type. [10]
More than one half of intrapulmonary sequestrations are diagnosed in later childhood or even in adulthood. Neonates and infants are usually asymptomatic. [11] In contrast, more than one half of extrapulmonary sequestrations are diagnosed in patients younger than 1 year. Often, this is because other congenital anomalies are present, including congenital diaphragmatic hernia, cardiac malformations, and GI malformations.
Prognosis
In the absence of perioperative complications, surgical resection of the abnormal segment is usually curative. Prognosis may also be determined by the presence of any accompanying anomalies.
A study by Trabalza Marinucci et al, which compared the outcomes of pediatric and adult patients who underwent surgical treatment of pulmonary sequestration, found that early surgery during childhood may prevent the development of respiratory symptoms. Patients who received a prenatal diagnosis and underwent surgery after the age of 1 year were more likely to have symptoms than those who were treated before the age of 1 year (57% vs 23%; P = .08). [12]
Morbidity/mortality
The morbidity and mortality rates are exceedingly low if resection of the mass precedes repeated infection. Postoperative results are uniformly good. [13]
-
The multicystic lesion in the left lower lobe seen on the chest radiograph of this patient was causing repeated respiratory infections.
-
The sequestration (S) is linked by an aberrant vessel (arrows).