Background
Pediatric small bowel obstructions have a variable etiology, with processes that can be divided into acute intestinal obstructions and chronic, partial intestinal obstructions. These conditions can be further subdivided into those that present in the immediate postnatal period (congenital intestinal obstructions) and those that occur later in childhood. (See Etiology, Presentation, and Workup.)
Congenital obstructive lesions of the intestines can be viewed as intrinsic (atresia, stenosis, meconium ileus, aganglionic bowel in Hirschsprung disease) or extrinsic (malrotation, congenital bands, internal hernias, duplications).
 Pediatric Small Bowel Obstruction. Small bowel obstruction is visible on a plain radiograph caused by intussusception in a 5-month-old patient.
Pediatric Small Bowel Obstruction. Small bowel obstruction is visible on a plain radiograph caused by intussusception in a 5-month-old patient.
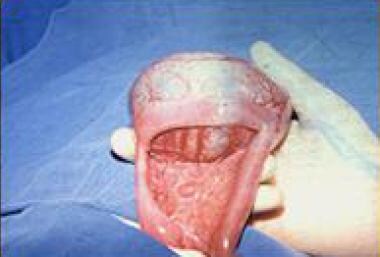
 Pediatric Small Bowel Obstruction. The surgical photograph depicts a transition zone in a patient with small bowel obstruction.
Pediatric Small Bowel Obstruction. The surgical photograph depicts a transition zone in a patient with small bowel obstruction.
Intestinal obstruction should be suspected in any child with persistent vomiting, abdominal distention, and abdominal pain. Delayed diagnosis and treatment can have devastating consequences. Infants and young children with intestinal obstruction present with feeding intolerance, irritability, vomiting, pain, and abdominal distention. Undiagnosed or improperly managed obstructions can progress to intestinal ischemia, which in turn can progress to necrosis, perforation, and sepsis when left untreated. [1] (See Prognosis, Presentation, and Workup.)
Pathophysiology
The normal small bowel contains gas and chyle, which is the sum of food and salivary, gastric, biliary, pancreatic, and intestinal secretions. Chyle continues to accumulate even without oral intake. Intrinsic or extrinsic small bowel obstruction leads to accumulating secretions that dilate the intestine proximal to the obstruction. Increased peristaltic contractions and intraluminal pressure may cause frequent loose stools and flatus early in the disease course. Vomiting is also an important sign of obstruction in children, and its characteristics can suggest the level of the obstruction.
Intestinal absorption, lymphatic drainage, and perfusion are compromised when intraluminal pressure exceeds capillary and venous pressure in the bowel wall. First, lymphatic obstruction occurs because of the lower pressure in these vessels. This is followed by venous obstruction, which accelerates edema formation because blood can enter the affected bowel segment but does not have a drainage route. Finally, the continued increase in bowel wall pressure eventually blocks arterial flow. Bowel ischemia ensues when capillary blood flow stops, allowing bacterial translocation into the peritoneal cavity, which can then lead to peritonitis and sepsis. Perforation can develop as the ischemia leads to bowel necrosis. Moreover, massive third spacing of fluids can lead to shock, further contributing to morbidity and mortality. This sequence may occur more rapidly in a closed-loop obstruction because there is no proximal escape for pressurized bowel contents.
Etiology
A wide variety of diagnoses can cause small bowel obstruction in children, such as the following:
-
Adhesive small bowel obstruction
-
Intestinal volvulus
-
Malrotation
-
Intussusception
-
Hirschsprung disease
-
Meckel diverticulum
-
Omphalomesenteric duct remnant (Meckel band)
-
Mesenteric and omental cysts
-
Necrotizing enterocolitis
-
Incarcerated hernias
-
Small intestinal atresia or stenosis
-
Meconium ileus/distal intestinal obstruction syndrome
-
Internal hernia
-
Enteric duplications
-
Inflammatory bowel disease
-
Intestinal neoplasm
-
Foreign material from previous operations, such as surgical staples after laparoscopic appendectomy (rare) [4]
A sampling of the many etiologies that can cause small bowel obstruction in children are discussed in greater detail below.
Intussusception
Intussusception is the most common cause of intestinal obstruction in infants and children aged 3 months to 6 years. Approximately 60% of children are younger than 1 year, and 80-90% are younger than 2 years. [5] The peak age of presentation is between the ages of 5 and 10 months. Intussusception is more common in males.
Intussusception occurs when a proximal segment of the intestine (the intussusceptum) telescopes or invaginates into the lumen of another immediately adjacent distal segment (the intussuscipiens). Intussusceptions are believed to begin with an intestinal spasm around a lead point; the bowel relaxes just distally to this spasm, which allows the longitudinal muscle fibers to draw the contracted portion of bowel into the relaxed portion. In 95% of cases, the intussusception is in the ileocecal area. Ileoileal and colocolic intussusceptions are rare. Occasionally, an ileoileal intussusception of the terminal ileum may progress through the ileocecal valve, a condition known as ileoileocolic intussusception. See the image below.
 Pediatric Small Bowel Obstruction. This is a surgical photograph of an 8-month-old patient with ileocolic intussusception.
Pediatric Small Bowel Obstruction. This is a surgical photograph of an 8-month-old patient with ileocolic intussusception.
Primary and secondary intussusception
Most intussusceptions are idiopathic, also known as primary intussusception. A lead point is identified in only 1.5-12% of cases; these cases are classified as secondary intussusception. [6]
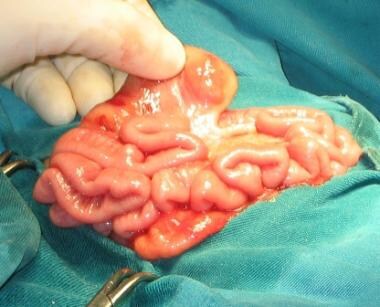
 Pediatric Small Bowel Obstruction. The surgical photograph was obtained in an 8-month-old boy with intussusception. The surgeon's finger is inserted into the intussusceptum, and the intussuscipiens is seen entering the distal bowel. No lead point was identified.
Pediatric Small Bowel Obstruction. The surgical photograph was obtained in an 8-month-old boy with intussusception. The surgeon's finger is inserted into the intussusceptum, and the intussuscipiens is seen entering the distal bowel. No lead point was identified.
 Pediatric Small Bowel Obstruction. Small bowel obstruction is visible on a plain radiograph caused by intussusception in a 5-month-old patient.
Pediatric Small Bowel Obstruction. Small bowel obstruction is visible on a plain radiograph caused by intussusception in a 5-month-old patient.
Primary intussusception accounts for 90-95% of children with intussusception; commonly, a viral etiology is suspected because of this condition's seasonal predisposition for spring and autumn, as well as a higher incidence of adenoid hypertrophy in children who suffer intussusceptions. Cough and diarrhea are common symptoms preceding intussusception, further suggesting that viral infections may be a cause. [7]
Gastroenteritis, rotavirus infection, or allergic stimuli are believed to cause intestinal lymphoid tissue to swell and become a lead point for intussusception. [8] An analysis by Okimoto et al of 71 stool samples from pediatric patients with intussusception indicated that adenovirus is also a risk factor for the development of intussusception. [9] Additionally, although the risk is quite small, some studies have demonstrated an increased risk of intussusception after the administration of monovalent rotavirus vaccination. [10, 11] Given the well-documented benefits of rotavirus vaccination, its benefits likely outweigh the small risk of intussusception. Nonetheless, currently monovalent (RV1, Rotarix) and pentavalent (RV5 RotaTeq) rotavirus vaccines are contraindicated in children with a history of intussusception.
Various conditions have been implicated as causes of secondary intussusception, including Meckel diverticulum, polyps, small bowel lymphoma, duplication cysts, vascular malformations, inverted appendiceal stumps, parasites, Henoch-Schönlein purpura (HSP, also called immunoglobulin [Ig]A vasculitis), cystic fibrosis, hemolytic-uremic syndrome, celiac disease, and Clostridium difficile colitis. [6] Meckel diverticulum is the most commonly identified pathologic lead point in most case series in children. [5]
Neoplastic masses can also act as lead points for intussusception, including primary tumors such as lymphomas and carcinomas, as well as metastatic disease. In particular, intestinal lymphomas are a frequent culprit that should be suspected in older children presenting with intussusception. Tumors causing intussusception primarily affect the duodenum and jejunum, and treatment includes surgical resection of the tumor once intussusception has been diagnosed. [12] Children undergoing extensive retroperitoneal dissections, such as that required for neuroblastoma or Wilms tumor resections, are also at risk of postoperative intussusceptions. These intussusceptions typically involve the small bowel alone and occur within 2 weeks after a previous laparotomy. [13]
Intussusception has also been described in patients with parasites, particularly Ascaris lumbricoides. [14] In Henoch-Schönlein purpura, mucosal hematomas are thought to act as lead points. [15]
Finally, Peutz-Jeghers syndrome (PJS) is a rare cause of intussusception in older children; in this condition, hamartomatous polyps, usually located in the small bowel, act as the lead point. van Lier et al studied 110 patients with PJS, finding that 69% of them presented with at least one episode of intussusception, with 95% of those intussusceptions located in the small bowel and 92.5% requiring surgical correction. [16] Most polyps acting as lead points were larger than 10 mm; thus, the authors recommended endoscopic surveillance with resection of larger polyps (10-15 mm) to prevent intussusception in patients with PJS. [16] Similarly, familial polyposis coli and juvenile polyposis can also cause intussusceptions.
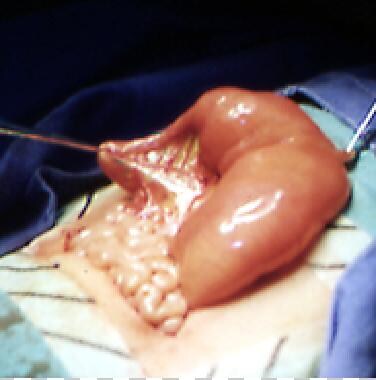
 Pediatric Small Bowel Obstruction. The surgical image depicts a laparotomy on a 7-month-old girl with ileocolic intussusception.
Pediatric Small Bowel Obstruction. The surgical image depicts a laparotomy on a 7-month-old girl with ileocolic intussusception.
Incarcerated hernia
Inguinal hernias are very common in children and are more common in premature infants. [17] Hernias can cause small bowel obstruction when they become incarcerated, meaning the contents of the hernia sac cannot be reduced back into the abdominal cavity. Incarcerated hernias may contain small bowel, the appendix (Amyand hernia), omentum, or, rarely, a Meckel diverticulum (Littre hernia). In girls, the ovary and/or fallopian tube are frequently incarcerated. When a part of the bladder wall or bowel wall is contained in the hernia sac, it is called a sliding hernia. Incarceration is the most common complication associated with inguinal hernias, with the risk thought to be increased among premature infants. [18, 19]
 Pediatric Small Bowel Obstruction. This image reveals small bowel obstruction caused by an incarcerated inguinal hernia in a 2-month-old infant with bilateral inguinal hernias as well as an umbilical hernia.
Pediatric Small Bowel Obstruction. This image reveals small bowel obstruction caused by an incarcerated inguinal hernia in a 2-month-old infant with bilateral inguinal hernias as well as an umbilical hernia.
Umbilical hernias are extremely common in children, and most close spontaneously. They very rarely incarcerate and therefore very rarely cause small bowel obstruction. Similarly, epigastric hernias are very common in children but rarely incarcerate. Femoral hernias do tend to incarcerate but are extremely rare in children.
Malrotation
Intestinal malrotation refers to errors of midgut rotation around the superior mesenteric artery axis and the subsequent fixation of the midgut in the peritoneal cavity. The primitive gut, which forms during the fourth week of embryonal life, is divided into the foregut, midgut, and hindgut. The largest of these, the midgut, is the only portion that undergoes rotation by herniating extraembryonically into the umbilical cord and rotating 270° in a counterclockwise direction around the superior mesenteric artery on its journey back to the abdominal cavity by 11 weeks' gestation. This produces the normal C-shaped configuration of the duodenum and results in the cecum coming to rest in the right lower quadrant of the abdomen. See the images below.
 Pediatric Small Bowel Obstruction. An upper gastrointestinal contrast study shows a malrotation with lack of a normal C-shaped duodenum and the small bowel "hanging" on the right side of the abdomen.
Pediatric Small Bowel Obstruction. An upper gastrointestinal contrast study shows a malrotation with lack of a normal C-shaped duodenum and the small bowel "hanging" on the right side of the abdomen.
 Pediatric Small Bowel Obstruction. This imaged is a contrast enema study showing an abnormally located cecum in a patient with malrotation.
Pediatric Small Bowel Obstruction. This imaged is a contrast enema study showing an abnormally located cecum in a patient with malrotation.
For unknown reasons, midgut rotation can arrest at any point, most commonly rotating 180° and leaving the cecocolic loop in the right upper quadrant. The duodenojejunal limb remains in a position of nonrotation, and the cecocolic limb has partial rotation (usually approximately 90° instead of 180°). The end result is that the cecum winds up in the mid-upper abdomen, and the abnormally positioned cecum is fixated to the right lateral abdominal wall by bands of peritoneum (Ladd bands). The Ladd bands cross the duodenum and can cause extrinsic compression and obstruction of the duodenum. This configuration leaves a narrow mesenteric root and creates a predisposition to clockwise volvulus of the midgut around an axis formed by the superior mesenteric artery. Midgut volvulus is a surgical emergency and can lead to complete necrosis of the midgut if not managed expeditiously (see the image below). The Ladd bands themselves can also obstruct the duodenum, which can create a more chronic, partially obstructive picture even in the absence of volvulus.
 Pediatric Small Bowel Obstruction. The surgical photograph shows necrotic bowel in a patient with midgut volvulus.
Pediatric Small Bowel Obstruction. The surgical photograph shows necrotic bowel in a patient with midgut volvulus.
Postoperative adhesions
Adhesions following intra-abdominal surgery are a very common cause of small bowel obstruction, often occurring in areas of ischemia or serosal damage. [1, 20] Laparotomy for inflammatory conditions renders a patient particularly prone to adhesive small bowel obstruction. Postsurgical onset of obstructive symptoms is variable. [21] The incidence of adhesive small bowel obstructions appears to be lower after laparoscopic procedures compared to open. [22]
Mesocolic (internal) hernia
Mesocolic (internal) hernias are rare rotational abnormalities in which nonfixed colonic and duodenal mesenteries allow formation of potential spaces for bowel herniation. [23, 24] Mesocolic hernias can be right-sided or left-sided and can occasionally incarcerate and strangulate. In addition, they can occasionally cause more chronic and intermittent partial obstructions. Iatrogenic internal hernias can also occur postoperatively if a mesenteric defect is not properly closed. See the image below.
Necrotizing enterocolitis
Necrotizing enterocolitis (NEC) is a common neonatal emergency that primarily affects premature neonates and low-birth-weight infants—it is associated with significant morbidity and mortality. [25] NEC can occasionally present with an obstructive picture in the acute setting. In addition, small bowel obstructions can present later after recovery from a prior episode of NEC. These obstructions are frequently caused by strictures. However, the most common location for NEC strictures is the colon.
Meckel diverticulum
Meckel diverticulum is the most common small bowel congenital malformation, with an estimated incidence of 1.2% in autopsy studies. [26] It is characterized by a true diverticulum (including the four layers of the intestinal wall) arising from an incompletely obliterated omphalomesenteric duct (see the image below).
Although mostly asymptomatic, Meckel diverticulum can cause symptoms in the setting of gastrointestinal bleeding from heterotopic gastric mucosa within the diverticulum or with the development of Meckel diverticulitis. The diverticulum itself does not typically cause obstruction. However, Meckel diverticulum can act as a lead point for intussusception. In addition, an omphalomesenteric duct remnant or band is occasionally associated with the diverticulum and can act as point of obstruction, volvulus, or internal herniation.
Enteric duplication
Duplications of the alimentary tract make up a group of rare malformations that vary greatly in appearance, size, location, and symptoms. They have been reported to occur anywhere along the gastrointestinal tract, although most are located in the terminal ileum near the ileocecal valve. Duplications are seen in 1 of every 4500 autopsies; 85% of cases are detected by age 2 years. [27] These cystic structures generally cause symptoms through mass effect, and duplications can cause partial or complete small bowel obstructions (see the image below).
 Pediatric Small Bowel Obstruction. The surgical photograph is that of a 3-year-old male patient with an obstructive, noncommunicating ileal duplication.
Pediatric Small Bowel Obstruction. The surgical photograph is that of a 3-year-old male patient with an obstructive, noncommunicating ileal duplication.
Jejunoileal atresia
Jejunoileal atresia is believed to result from intrauterine mesenteric vascular accidents. The extent of atresia and the appearance of the atretic intestinal segment vary according to the timing and degree of the disruption of the mesenteric blood supply (see the images below). Jejunoileal atresias are classified into the following four types based upon anatomic characteristics:
-
Type 1: No discontinuity in the bowel, obstruction from a diaphragm or web, no mesenteric defect
-
Type 2: Discontinuous bowel connected with a fibrous cord, no mesenteric defect
-
Type 3a: Presence of a gap between discontinuous bowel with a mesenteric defect
-
Type 3b (“apple peel” or “Christmas tree” atresia): Presence of a large gap and mesenteric defect between a discontinuous proximal atresia and distal small bowel that is shortened and coiled around its mesentery
-
Type 4: Presence of multiple atresias, often appearing as a “string of sausages”
 Pediatric Small Bowel Obstruction. An upper gastrointestinal contrast study demonstrates a jejunal atresia with a proximal dilated atretic bowel and lack of passage of contrast material into the distal small bowel.
Pediatric Small Bowel Obstruction. An upper gastrointestinal contrast study demonstrates a jejunal atresia with a proximal dilated atretic bowel and lack of passage of contrast material into the distal small bowel.
 Pediatric Small Bowel Obstruction. This is a surgical photograph of the patient in the previous image, depicting the proximal dilated atretic jejunum.
Pediatric Small Bowel Obstruction. This is a surgical photograph of the patient in the previous image, depicting the proximal dilated atretic jejunum.
 Pediatric Small Bowel Obstruction. The surgical image depicts a laparotomy on a 2-day-old female patient with congenital small bowel obstruction. A type I jejunal atresia without mesenteric gap and a grossly dilated proximal intestine is seen.
Pediatric Small Bowel Obstruction. The surgical image depicts a laparotomy on a 2-day-old female patient with congenital small bowel obstruction. A type I jejunal atresia without mesenteric gap and a grossly dilated proximal intestine is seen.
 Pediatric Small Bowel Obstruction. The surgical photograph was obtained in a newborn with a type IIIa jejunal atresia. Note the dilated proximal bowel pouch, the mesenteric V-shaped defect, and the thin, nondilated distal jejunum.
Pediatric Small Bowel Obstruction. The surgical photograph was obtained in a newborn with a type IIIa jejunal atresia. Note the dilated proximal bowel pouch, the mesenteric V-shaped defect, and the thin, nondilated distal jejunum.
 Pediatric Small Bowel Obstruction. This surgical photograph was obtained from a newborn with type IIIb (“apple peel” or “Christmas tree”) atresia. Note the shortened distal small bowel coiled around its mesentery.
Pediatric Small Bowel Obstruction. This surgical photograph was obtained from a newborn with type IIIb (“apple peel” or “Christmas tree”) atresia. Note the shortened distal small bowel coiled around its mesentery.
Duodenal obstructions
Duodenal obstructions in newborns may be partial or complete and secondary to extrinsic or intrinsic abnormalities. Duodenal atresia and stenosis are intrinsic obstructions believed to be caused by failure of recanalization of the duodenum after the embryologic cord stage. Duodenal atresia and stenosis are relatively rare causes of obstruction. Duodenal atresia has a high rate of associated anomalies.
The anatomic classification of duodenal atresia is as follows:
-
Type I: Luminal web or membrane
-
Type II: Complete atresia connected by a fibrous cord
-
Type III: Complete atresia with a mesenteric gap between the affected intestinal segments
 Pediatric Small Bowel Obstruction. This contrast-enhanced upper gastrointestinal film shows a duodenal atresia in a 2-day-old newborn.
Pediatric Small Bowel Obstruction. This contrast-enhanced upper gastrointestinal film shows a duodenal atresia in a 2-day-old newborn.
Annular pancreas
Annular pancreas is a rare congenital anomaly that causes an extrinsic duodenal obstruction. It occurs when the ventral pancreatic bud fails to rotate behind the duodenum, leaving pancreatic tissue fully encircling the second portion of the duodenum. This results in a nondistensible ring of pancreatic parenchyma and a functional stenosis. These lesions may coexist with duodenal atresia and stenosis. [28] An annular pancreas can be asymptomatic, or it can cause external compression on the second portion of the duodenum, which creates a partial or complete obstruction.
Meconium ileus
Meconium ileus occurs almost exclusively in neonates with cystic fibrosis and is usually its earliest clinical manifestation. The disease is caused by the accumulation of hyperviscous and thickened meconium that obstructs the distal small intestine and colon. Dilatation of the involved and obstructed bowel segment can also lead to volvulus or perforation (complicated meconium ileus). A similar pathologic process that causes distal small bowel obstruction can occur in older children with cystic fibrosis, referred to as distal intestinal obstruction syndrome (DIOS).
Hirschsprung disease
Hirschsprung disease is a functional distal bowel obstruction resulting from the abnormal development of the enteric nervous system and ensuing aganglionosis of the distal gut. It is an uncommon cause of small bowel obstruction, as the transition between ganglionic and aganglionic bowel is most commonly located in the colon. However, in cases of total colonic Hirschsprung disease, the transition does occur within the small intestine, with a resulting obstruction at that level.
Epidemiology
Congenital obstructions
Malrotation of the bowel with midgut volvulus occurs at a rate of 1 case per 6000 live births. [29] Jejunoileal atresia and stenosis have a combined reported incidence of 1 case per 1500-5000 live births. These conditions are common among patients with maternal polyhydramnios; 38% have jejunal atresia, and 15% have ileal atresia. Overall, atresias are almost equally divided between the jejunum (51%) and ileum (49%).
Jejunoileal atresia is twice as common as duodenal atresia and also occurs more commonly than colonic atresia. Duodenal atresia and stenosis, collectively, are relatively rare causes of obstruction that occur at a rate of just 1 case per 2,500-10,000 live births. [30, 31] The incidence of alimentary tract duplications is 1 case per 4500 population.
Sex-related differences
The male-to-female ratio for incarcerated hernias is 8:1. Hernias occur on the right in about 60% of males, on the left in 25%, and bilaterally in 15%. Females have bilateral inguinal hernias more often than do males. Most other causes of small bowel obstruction equally affect both sexes. Malrotation of the bowel with midgut volvulus can affect either sex. Neither duplication cysts nor jejunoileal atresia exhibit a sexual predilection.
Age-related differences
Adhesive small bowel obstruction can occur among patients of any age who have had prior abdominal surgery. Certain causes of small bowel obstruction, however, are more likely to present and be diagnosed within certain age groups.
Intussusception can occur at any time in life, but the idiopathic form is primarily a childhood disease, developing especially during infancy. Peak occurrence is in children aged 5-10 months; the average age is about 7-8 months. Most patients with inguinal hernias present during the first year of life. Approximately one third are younger than 6 months at the time of surgery.
Most patients with symptomatic malrotation of the bowel with midgut volvulus present in early infancy. Approximately 50% of patients present in the first month of life, and 80% present in the first year of life. Midgut volvulus has reportedly occurred in utero. Fewer patients (ie, 6-20%) present at ages older than 1 year; these patients tend to have a longer course of vague symptoms (eg, intermittent, bilious vomiting; chronic abdominal pain).
Most patients with duplication cysts present in early childhood or infancy, although some may not develop symptoms until much later. Many duplication cysts are diagnosed within the first week of life; 60% are identified during the first 6 months of life, and 85% are identified by age 1 year. Jejunoileal atresia causes obstruction in the immediate postnatal period.
Patients with duodenal atresia typically present in the first 24 hours of life. However, patients with duodenal stenosis may remain asymptomatic until later in childhood; symptom onset depends upon the degree of stenosis.
For annular pancreas, the age of onset of obstructive symptoms also varies. On occasion, symptoms do not develop until adulthood. However, many pediatric patients present in the newborn period with complete duodenal obstruction, often after the first feeding.
Meconium ileus and meconium plug syndrome present in the first few days of life. A rare entity similar to meconium ileus that presents later in life is called "meconium ileus equivalent" or "distal intestinal obstruction syndrome" (DIOS).
Necrotizing enterocolitis is primarily a disease seen in premature infants. However, approximately 10% of cases occur in term infants.
Prognosis
Mortality and morbidity in pediatric small bowel obstruction depend on the type of lesion that causes the intestinal blockage and the time elapsed before diagnosis and definitive treatment, which affects the extent to which bowel is compromised. Mortality is generally low for most diagnoses with early identification and treatment.
Clinical factors that appear to be useful for identifying strangulated small bowel obstruction include two or more of the following: intractable continuous abdominal pain, tachycardia, leukocytosis, abdominal distention with ultrasonographically proven ascites or wall thickness and reduced wall contrast enhancement. [32] If left untreated, strangulated obstructions can be lethal. Mortality rates may reach 65% if more than 75% of the small bowel is necrotic at the time of laparotomy. With extensive bowel loss, children can suffer from malnutrition due to short-bowel syndrome. [33]
Strictures and adhesions are late complications of treated obstructions. Other long-term outcomes are largely dependent on the underlying etiology of the small bowel obstruction. Long-term survival in patients with duodenal atresia or stenosis is approximately 86%, and most of the morbidity and mortality is related to cardiac anomalies. [34] The survival rate at 1 year is approximately 92% in patients with uncomplicated meconium ileus and 89% in patients with complicated disease. [35]
Necrotizing enterocolitis (NEC) carries a mortality of 15-30%. [36] Mortality is higher in surgically treated infants, reaching up to 50%, and depends on the extent of bowel involvement. Infants with pan-intestinal involvement show a 33% survival, compared with 69.5% survival for multifocal disease. Isolated NEC has an 88% survival. [37] Wright et al reported a particularly high (80%) mortality among premature neonates undergoing surgery for NEC. [38] Survivors of NEC frequently have long-term complications, including short bowel syndrome, abnormal growth, and neurodevelopmental delay. The incidence of intestinal failure among infants undergoing surgical treatment for NEC is relatively high and increased among those with a greater extent of bowel resection. [39]
-
Pediatric Small Bowel Obstruction. Small bowel obstruction is visible on a plain radiograph caused by intussusception in a 5-month-old patient.
-
Pediatric Small Bowel Obstruction. This barium enema study reveals a coil spring appearance caused by the tracking of barium around the lumen of the edematous intestine in intussusception.
-
Pediatric Small Bowel Obstruction. This image reveals small bowel obstruction caused by an incarcerated inguinal hernia in a 2-month-old infant with bilateral inguinal hernias as well as an umbilical hernia.
-
Pediatric Small Bowel Obstruction. This radiograph depicts the double-bubble sign characteristic of duodenal atresia.
-
Pediatric Small Bowel Obstruction. An upper gastrointestinal contrast study demonstrates a jejunal atresia with a proximal dilated atretic bowel and lack of passage of contrast material into the distal small bowel.
-
Pediatric Small Bowel Obstruction. This is a surgical photograph of the patient in the previous image, depicting the proximal dilated atretic jejunum.
-
Pediatric Small Bowel Obstruction. An upper gastrointestinal contrast study shows a malrotation with lack of a normal C-shaped duodenum and the small bowel "hanging" on the right side of the abdomen.
-
Pediatric Small Bowel Obstruction. This imaged is a contrast enema study showing an abnormally located cecum in a patient with malrotation.
-
Pediatric Small Bowel Obstruction. The surgical photograph shows necrotic bowel in a patient with midgut volvulus.
-
Pediatric Small Bowel Obstruction. Necrotic bowel is shown after surgical reduction of an intussusception.
-
Pediatric Small Bowel Obstruction. The surgical photograph depicts a transition zone in a patient with small bowel obstruction.
-
Pediatric Small Bowel Obstruction. An incarcerated left inguinal hernia is noted.
-
Pediatric Small Bowel Obstruction. This photograph reveals a mesocolic hernia.
-
Pediatric Small Bowel Obstruction. The surgical image depicts a laparotomy on a 7-month-old girl with ileocolic intussusception.
-
Pediatric Small Bowel Obstruction. The surgical image depicts a laparotomy on a 2-day-old female patient with congenital small bowel obstruction. A type I jejunal atresia without mesenteric gap and a grossly dilated proximal intestine is seen.
-
Pediatric Small Bowel Obstruction. A barium enema study on a 1-year-old male patient depicts an ileocolic intussusception.
-
Pediatric Small Bowel Obstruction. The clinical photograph of a 5-month-old male patient reveals characteristic currant-jelly stools due to intussusception.
-
Pediatric Small Bowel Obstruction. The plain abdominal film on a 3-day-old newborn depicts the classic double-bubble sign for duodenal atresia.
-
Pediatric Small Bowel Obstruction. This contrast-enhanced upper gastrointestinal film shows a duodenal atresia in a 2-day-old newborn.
-
Pediatric Small Bowel Obstruction. The surgical photograph is that of a 3-year-old male patient with an obstructive, noncommunicating ileal duplication.
-
Pediatric Small Bowel Obstruction. This plain abdominal film was obtained in a 6-year-old male patient with CPID (cerebral palsy intellectual disability) and an organo-axial gastric volvulus. Note the grossly dilated and obstructed stomach. A gastrostomy feeding tube can be seen in place. Surgical staples from a previous laparoscopic fundoplication are seen near the diaphragmatic crura.
-
Pediatric Small Bowel Obstruction. This is a surgical photograph of an 8-month-old patient with ileocolic intussusception.
-
Pediatric Small Bowel Obstruction. The plain abdominal film of a premature baby born at 28 weeks of gestation reveals necrotizing enterocolitis. Note the "railroad sign" (pneumatosis intestinalis) in the hepatic flexure and "soap bubbles" in the descending colon.
-
Pediatric Small Bowel Obstruction. This clinical image of a micro-premature baby boy shows discoloration on the right lower quadrant of the abdomen due to intestinal perforation secondary to necrotizing enterocolitis. An umbilical catheter is in place.
-
Pediatric Small Bowel Obstruction. A plain abdominal film of a premature baby girl with necrotizing enterocolitis is shown. Note the air in the biliary tree and the grossly dilated bowel.
-
Pediatric Small Bowel Obstruction. This is a surgical photograph of a 1-year-old male patient who previously underwent a right radical nephrectomy for Wilms tumor. He presented to the emergency department with signs of a mechanical small bowel obstruction. A transition zone is clearly seen at the point where the small bowel is trapped on an internal hernia through a mesenteric gap.
-
Pediatric Small Bowel Obstruction. This sonogram reveals intussusception in a 9-month-old male patient.
-
Pediatric Small Bowel Obstruction. The surgical photograph was obtained in an 8-month-old boy with intussusception. The surgeon's finger is inserted into the intussusceptum, and the intussuscipiens is seen entering the distal bowel. No lead point was identified.
-
Pediatric Small Bowel Obstruction. The surgical photograph depicts loops of bowel passing through a mesenteric defect. The bowel segment proximal to the obstruction is dilated, purplish, distended, and hypoperistaltic. The bowel distal to the obstruction is decompressed and normal-looking.
-
Pediatric Small Bowel Obstruction. The surgical photograph was obtained in a newborn with a type IIIa jejunal atresia. Note the dilated proximal bowel pouch, the mesenteric V-shaped defect, and the thin, nondilated distal jejunum.
-
Pediatric Small Bowel Obstruction. The surgical photograph depicts a Meckel diverticulum.
-
Pediatric Small Bowel Obstruction. This surgical photograph was obtained from a newborn with type IIIb (“apple peel” or “Christmas tree”) atresia. Note the shortened distal small bowel coiled around its mesentery.