Background
Hyperkalemia is defined as a serum potassium concentration greater than the upper limit of the normal range; the range in children and infants is age-dependent, whereas the range for adults is approximately 3.5-5.5 mEq/L. The upper limit may be considerably high in young or premature infants, as high as 6.5 mEq/L. [1] Because hyperkalemia can cause lethal cardiac arrhythmia, it is one of the most serious electrolyte disturbances. [2]
Teach patients to recognize the symptoms of hyperkalemia, such as palpitations, dizziness, and weakness.
Pathophysiology
Potassium is the primary intracellular cation; more than 95-98% of the total body potassium is found in the intracellular space, primarily in muscle. [3] Normal homeostatic mechanisms serve to precisely maintain the serum potassium level within a narrow range. The primary mechanisms for maintaining this balance are the buffering of extracellular potassium against a large intracellular potassium pool (via the sodium-potassium pump) and urinary excretion of potassium.
Under normal, nonpathologic conditions, approximately 90% of potassium excretion occurs in the urine, with less than 10% of potassium excreted through sweat or stool. Within the kidneys, potassium excretion occurs mostly in the principal cells of the cortical collecting duct (CCD). Urinary potassium excretion depends on adequate luminal sodium delivery to the distal convoluted tubule (DCT) and CCD, as well as the effect of aldosterone and other adrenal corticosteroids with mineralocorticoid activity.
Laboratory hyperkalemia (fictitious or pseudohyperkalemia) can easily occur because of hemolysis, tissue lysis, and "milking" of extremities (which can introduce a significant amount of interstitial fluid into the blood sample) during phlebotomy, especially with heel-poke and finger-stick phlebotomy, which are commonly performed in infants and small children. Hemolysis can also be caused by fist clenching during phlebotomy or during prolonged tourniquet application, which can also lead to an acidotic sample with resultant hyperkalemia). Blood sampled "upstream" of an intravenous line with potassium-containing fluid (or from a multiple lumen central venous catheter where the sampling lumen is near the lumen containing potassium-rich infusate) can have falsely elevated levels of potassium that do not reflect circulating levels.
Similarly, serum potassium levels may be falsely lowered by sampling upstream of a catheter delivering fluid deficient in potassium or when a small blood sample is obtained and placed in testing media low in potassium, which may be the case with specific point-of-care analyzers. [4] When in doubt, blood samples should be obtained and tested using standard methods.
Thrombocytosis can also lead to false elevations of serum potassium levels. The normal serum potassium level is 0.4 mEq/L higher than the plasma level because of potassium release during clot formation. For every 100,000/mL elevation in the platelet count, the serum potassium increases by approximately 0.15 mEq/L. This can easily be corrected based on a measurement of whole blood potassium level. A similar effect on serum but not plasma potassium can also be seen with leukocytosis.
True hyperkalemia is caused by one of the following three basic mechanisms, although the root cause for any individual patient is often multifactorial:
-
Increased K+ intake: Increased K+ intake is most commonly caused by intravenous or oral potassium supplementation. Packed RBCs (PRBCs) also carry potentially high concentrations of potassium that can lead to hyperkalemia during PRBC transfusion. [5] Since serum potassium levels represent only a small percentage (usually < 2-5%) of total body potassium stores, long-term increases in potassium intake are only rarely associated with significant serum hyperkalemia, unless excretion is inadequate.
-
Decreased potassium excretion: The most common cause of decreased potassium excretion leading to hyperkalemia is oliguric renal failure. Other causes include primary adrenal disease (eg, Addison disease, salt-wasting forms of congenital adrenal hyperplasia), hyporeninemic hypoaldosteronism, renal tubular disease (pseudohypoaldosteronism I [6, 7] or II [8] ), or medications (eg, angiotensin-converting enzyme [ACE] inhibitors, angiotensin II receptor blockers [ARBs], spironolactone or other potassium-sparing diuretics).
-
Transcellular potassium shifts: In a transcellular potassium shift, a hydrogen ion enters a cell and leads to decreased K+ uptake by the cell in order to maintain electrical neutrality. Acidosis is the most common cause of hyperkalemia due to transcellular potassium shift, but any process that leads to cellular injury or death (eg, tumor lysis syndrome, rhabdomyolysis, crush injury, massive hemolysis) can cause hyperkalemia, as intracellular potassium is released by disruption of the cell membrane. Other causes of hyperkalemia due to transcellular shift of potassium include propofol ("propofol infusion syndrome"), [9] toxins (digitalis intoxication or fluoride intoxication), succinylcholine, beta-adrenergic blockade, strenuous or prolonged exercise, insulin deficiency, malignant hyperthermia, and hyperkalemic periodic paralysis.
Plasma potassium levels are generally maintained at 3.5-5 mEq/L in adults, with higher levels in neonates and small infants. levels greater than 7 mEq/L can lead to significant hemodynamic and neurologic consequences, while levels exceeding 8.5 mEq/L can cause respiratory paralysis or cardiac arrest and can quickly be fatal. High levels of potassium cause abnormal heart and skeletal muscle function by lowering cell-resting action potential and preventing repolarization, leading to muscle paralysis. Classic electrocardiographic (ECG) findings begin with tenting of the T wave (as is shown in the image below), followed by lengthening and eventual disappearance of the P wave and widening of the QRS complex. [10]
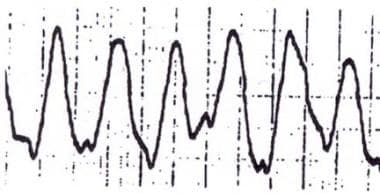
Prior to asystole, the QRS and T wave may merge to form a sinusoidal wave (as is shown in the image below).
Table. Select Factors Affecting Plasma Potassium (Open Table in a new window)
Factor |
Effect on Plasma K+ |
Mechanism |
Aldosterone |
Decrease |
Increases sodium resorption, and increases K+ excretion |
Insulin |
Decrease |
Stimulates K+ entry into cells by increasing sodium efflux (energy-dependent process) |
Beta-adrenergic agents |
Decrease |
Increases skeletal muscle uptake of K+ |
Alpha-adrenergic agents |
Increase |
Impairs cellular K+ uptake |
Acidosis (decreased pH) |
Increase |
Impairs cellular K+ uptake |
Alkalosis (increased pH) |
Decrease |
Enhances cellular K+ uptake |
Cell damage |
Increase |
Intracellular K+ release |
Succinylcholine |
Increase |
Cell membrane depolarization |
Etiology
Although the etiology of hyperkalemia can be multifactorial, differential diagnoses include fictitious hyperkalemia and hyperkalemia due to increased potassium intake, transcellular potassium shift, or decreased potassium excretion.
Fictitious hyperkalemia may be caused by the following:
-
Hemolysis, tissue lysis, or tissue ischemia during phlebotomy [8]
-
Contamination of blood sample with potassium-containing fluids
-
Thrombocytosis or leukocytosis (affects serum K+ but not plasma K+)
Hyperkalemia due to increased K+ intake may be due to the following:
-
Intravenous (IV) or oral potassium
-
Maintenance K+ in IV or oral solutions combined with decreased renal function
Hyperkalemia due to transcellular K+ shift may be caused by the following:
-
Metabolic acidosis
-
Acute tubular necrosis
-
Electrical burns
-
Thermal burns
-
Cell depolarization
-
Head trauma
-
Rhabdomyolysis
-
Digitalis toxicity
-
Fluoride toxicity [17]
-
Cyclosporin A [18]
-
Methotrexate [19]
-
Propofol infusion syndrome
-
Tumor lysis syndrome
-
Succinylcholine use in a child with neuromuscular disease, prolonged bed rest (including patients in intensive care units), or more than 24 hours after crush or burn injury [20]
Hyperkalemia due to decreased K+ excretion may result from the following:
-
Acute renal failure
-
Primary adrenal disease (Addison disease, salt-wasting congenital adrenal hyperplasia)
-
Hyporeninemic hypoaldosteronism
-
Renal tubular disease
Certain types of medications (eg, potassium sparing diuretics, angiotensin-converting enzyme [ACE] inhibitors, angiotensin II blockers, trimethoprim, nonsteroidal anti-inflammatory agents [NSAIDs]) may also lead to the development of hyperkalemia.
Rarely, a Mendelian syndrome known as familial hyperkalemic hypertension (FHHt) or pseudohypoaldosteronism II may manifest as hyperkalemia in children. [8] The involvement of relatively newly discovered genes KLHL3 and CUL3 appear to play a role in the pathophysiology of FHHt. Clinicians should actively search for abnormalities in blood pressure in the setting of pediatric hyperkalemia with a normal glomerular filtration rate. [8]
Epidemiology
United States data
Hyperkalemia is a manifestation of a disease and is not a disease by itself. The incidence of hyperkalemia in the pediatric population is unknown, but is considered rare. [8] However, the prevalence of hyperkalemia in extremely low birth weight premature infants can exceed 50%. [21] Hyperkalemia in pediatric patients is most commonly associated with renal insufficiency, acidosis, and with diseases that involve defects in mineralocorticoid, aldosterone, and insulin function. [22] In addition, hemolysis in blood specimens owing to difficulties in obtaining samples may also be a factor. [8]
A cross-sectional analysis of data from the Chronic Kidney Disease in Children (CKiD) study showed the following factors increased the frequency of hyperkalemia in young patients: advanced stage CKD, glomerular disease, low carbon dioxide levels, and use of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers. [23]
International data
In a systematic review and meta-analysis of the prevalence and incidence of hyperkalaemia in observational studies, 26 studies comprising 1987-2020 general pediatric data from 19 countries showed a prevalence of hyperkalemia ranging from 5.5% (outpatient settings) to 17.3% (pediatric intensice care unit settings). [24] There was a 14% overall pooled mean prevalence of pediatric hyperkalemia. Of 23 studies comprising 1988-2020 neonatal intensive care data from 12 countries, the pooled mean prevalence was 28.0%. [24]
In the same review and analysis, one pediatric study reported an incidence of 22.0 cases per 100 person years in children receiving solid organ transplants who were on calcineurin inhibitors. [24]
Race-, sex-, and age-related demographics
No racial predilection nor sex-related predilection is observed. However, neuromuscular disorders including myotonic and muscular dystrophies and related disorders that can predispose patients to hyperkalemia with succinylcholine administration are more prevalent in males. [25]
Extremely low birth weight premature infants are particularly prone to hyperkalemia primarily due to immature renal function. Even otherwise full-term infants may have transient hyperkalemia and hyponatremia due to decreased responsiveness to aldosterone (pseudohypoaldosteronism I). [22]
Prognosis
Patient prognosis depends on the etiology of the hyperkalemia.
Morbidity/mortality
Sudden and rapid onset of hyperkalemia can be fatal. With slow or chronic increase in potassium levels, adaptation occurs via renal excretion, with fractional potassium excretion increasing by as much as 5-10 times the reference range.
Separately, hyperkalemia appears to be an independent risk factor for death in children with diarrhea requiring mechanical ventilation. [26]
The greatest risk factors for transfusion-associated hyperkalemia in children appear to be total transfused volume within 12 hours (tV-12) per kilogram as well as the age of red blood cell units. [14] In children with multiple comordities, an estimated 30% of estimated total blood volume (eTBV) may cause transfusion-associated hyperkalemia.
Complications
If untreated, severe hyperkalemia can result in cardiac arrhythmia or death.
Treatment of pseudohyperkalemia may result in hypokalemia; thus, treatment of non–life-threatening hyperkalemia should be deferred pending verification of hyperkalemia.
Failure to determine and treat the underlying disease process causing hyperkalemia can predispose patients to recurrent, life-threatening hyperkalemia.
-
Pediatric hyperkalemia. Peaked T waves.
-
Pediatric hyperkalemia. Sinusoidal wave.
-
Pediatric hyperkalemia. Hyperkalemia diagnosis and treatment flow chart.