Background
In 1881, Litten first described an intraretinal hemorrhage associated with subarachnoid hemorrhage in the German literature. [1] However, Terson's description of vitreous hemorrhage following subarachnoid hemorrhage in 1900 is now associated with this syndrome. Terson syndrome has been more broadly applied to intraocular hemorrhages associated with other causes of rapidly increased intracranial pressure beyond subarachnoid hemorrhages. [2, 3, 4, 5, 6, 7, 8, 9]
Problem
Terson syndrome originally was defined by the occurrence of vitreous hemorrhage in association with subarachnoid hemorrhage. Terson syndrome now encompasses any intraocular hemorrhage associated with intracranial hemorrhage and elevated intracranial pressures. Intraocular hemorrhage includes the development of subretinal, retinal, preretinal, subhyaloidal, or vitreal blood. The classic presentation is in the subhyaloidal space. [10]
Epidemiology
Consecutive case series have reported an incidence of 17-28% of intraocular hemorrhage with subarachnoid hemorrhage. This association is statistically associated with the severity of the subarachnoid hemorrhage based on the Hunt-Hess classification system of subarachnoid hemorrhages. [11, 12] The incidence of vitreous hemorrhage is much lower (3-13%). [13, 14, 15, 16] Papilledema and unconsciousness are both positively correlated with Terson syndrome. [17]
Etiology
Terson syndrome has been described most commonly in subarachnoid hemorrhages due to ruptured cerebral aneurysms. Although early studies attempted to link this syndrome with aneurysms of the anterior communicating artery, statistical analysis has not correlated it with a specific aneurysmal location. [18] Other reports include such causes as strangulation, trauma, hypertension, tumor, and perioperative and postoperative intracranial bleeding. [4, 14] Iatrogenic events resulting in rapidly increased intracranial pressure have also been reported. [6, 7]
Pathophysiology
The pathogenesis of Terson syndrome has been controversial. The earliest reports assumed that the intracerebral blood directly connected with the intraocular space through the lamina cribrosa. While electron microscopy of the optic nerve anatomy has not demonstrated a communication between the 2 spaces, 1 case report has demonstrated bilateral optic nerve sheath hemorrhages following rupture of an anterior choroidal artery aneurysm resulting in a Terson syndrome. [19] Pathological specimens have not shown any blood in the optic nerve sheath within 3 mm of the globe.
A 2010 postmortem retrospective series demonstrated areas of multifocal optic nerve hemorrhages, suggesting that the blood in the nerve sheath may originate from the vessels directly supplying the nerve rather than from the main inciting intracerebral source of bleeding. [10]
Another mechanism suggests that a sudden rise in the venous pressure caused by the intracerebral bleeding is transmitted to the eye and results in intraocular bleeding. However, experimental studies have shown that the intravenous pressures are not high enough to create an intraocular hemorrhage. [20]
The sudden rise in intracranial pressure probably is the primary inciting event in Terson syndrome. Intracranial pressure is transmitted through the optic nerve sheath to the swollen optic nerve head, which occludes the retinal and choroidal anastomoses at the level of the lamina cribrosa. The elevated venous pressure generated in the retinal venous system is assumed to rupture the superficial retinal vessels, resulting in intraocular hemorrhages. [21] A case report supports this theory by demonstrating peripapillary fluorescein leakage in a patient with vitreous hemorrhage secondary to a subarachnoid hemorrhage. [21]
A case series of Terson syndrome patients was analyzed with scanning laser ophthalmoscopy, which revealed blood spreading along vessels. The data, combined with SD-OCT results and intraoperative observations of those Terson syndrome patients, suggest that blood may enter the vitreous cavity around the retinal vessels surrounding the optic disc. [22] Because of these assumptions regarding the pathogenesis of the syndrome, the definition of Terson syndrome now includes any intraocular hemorrhage associated with intracranial bleeding and acutely increased intracranial pressure. Attempts have been made to correlate Terson syndrome with the intraocular hemorrhages seen in shaken baby syndrome because of the similarity in clinical findings in the eye and the brain, but acute tractional forces may be an additional factor contributing to the intraocular hemorrhage in the latter.
Presentation
The neurologic symptoms are related to intracranial bleeding. Reported visual acuities range from 20/20 to light perception, but they often are difficult to obtain secondary to the impaired neurologic status of the patient. [23] The degree of visual loss is related to the degree and extent of the intraocular hemorrhage.
The intraocular hemorrhage is often bilateral and superficial to the retina. Intraretinal or subretinal hemorrhages have been reported but are less frequent. However, these may be more difficult to diagnose in the setting of vitreous or subhyaloidal hemorrhage. Preretinal hemorrhage can develop into vitreous hemorrhage weeks after the initial inciting event. [10, 24, 25] The intraocular hemorrhage may be difficult to diagnose immediately because the ophthalmologist may be restricted from dilating the patient for neurologic monitoring. A decreased red reflex can be helpful in evaluating a patient who is comatose, and B-scan ultrasonography can further establish the extent of vitreous hemorrhage in lieu of a dilated funduscopic examination.
Indications
Strict guidelines for treatment have not been established by clinical studies. Patients have responded well to observation. [24, 26]
Assuming patients are stable enough for surgery following intracranial hemorrhage, indications for a vitrectomy include the following:
-
Nonclearing vitreous hemorrhage in patient who is monocular or dense binocular vitreous hemorrhage [27]
-
Retinal detachment with vitreous hemorrhage [27]
-
Late complications of intraocular hemorrhage, such as epiretinal membrane formation (macular pucker) [29]
-
Occupational or rehabilitation necessity for rapidly cleared vision [30]
Vitrectomy has been shown to be effective in quickly and safely restoring vision in Terson syndrome, even in cases delayed months after the intracranial hemorrhage. [31] Better outcomes in the setting of Terson syndrome are seen in younger patients and when vitrectomy is performed sooner after the intracranial event. [27, 32]
Relevant Anatomy
The relevant anatomy in Terson syndrome includes the inner retinal vasculature, choroidal vasculature, chorioretinal anastomoses near the optic nerve head, and subarachnoid space surrounding the optic nerve.
Contraindications
Contraindications for a vitrectomy include a small intraocular hemorrhage with a high likelihood of spontaneous clearing or an intraocular hemorrhage that is already spontaneously clearing. Patients with Terson syndrome are often poor surgical candidates because of the severity of the intracranial hemorrhage and often do not survive the devastating event.
Prognosis
Patients presenting with Terson syndrome have more severe subarachnoid hemorrhages based on the Glasgow Coma Scale or Hunt-Hess scale. Reported mortality rates increase from 3- to 12-fold in these patients compared to those with subarachnoid hemorrhages without Terson syndrome. [14, 15, 16, 26, 25]
-
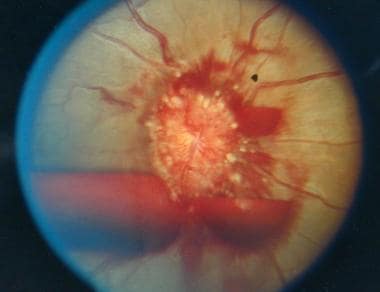
Right eye of a 28-year-old female with subarachnoid hemorrhage 1 week after intracranial surgery.
-
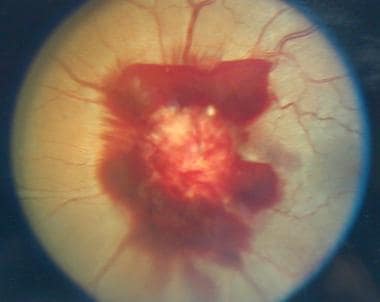
Left eye of a 28-year-old female with subarachnoid hemorrhage 1 week after intracranial surgery.