Types of Therapeutic Injections
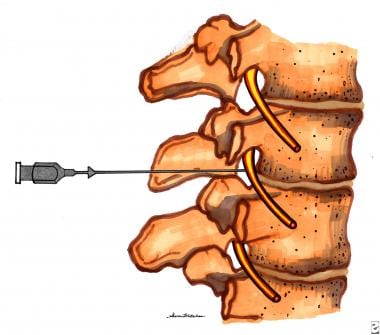
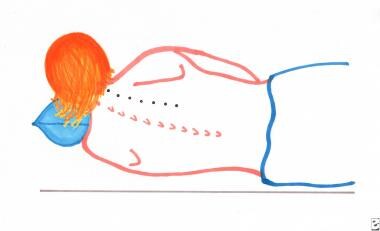
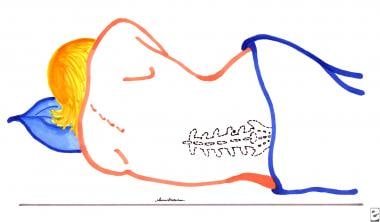
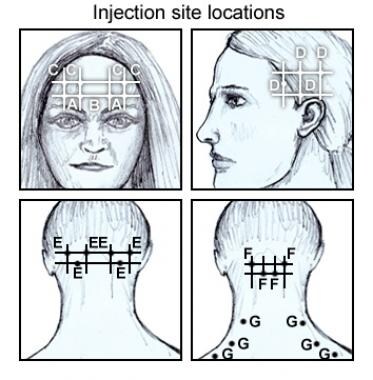
This article focuses on the use of therapeutic injections (see the image below) to treat acute and chronic pain syndromes. Discussion of this topic begins with an overview of regional anesthesia, which includes the pharmacology of frequently administered medications and basic information regarding equipment and safety. The spectrum of injection procedures and their indications for specific pain disorders and pathoanatomic regions is addressed to include therapeutic options for the various tissues or structures characteristic of each area or syndrome.
See Pain Management: Concepts, Evaluation, and Therapeutic Options, a Critical Images slideshow, to help assess pain and establish efficacious treatment plans.
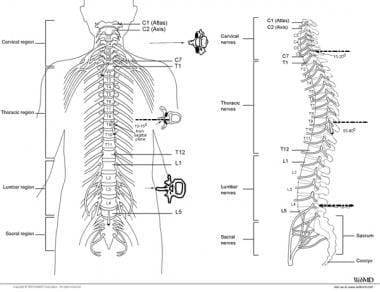
The following anatomical divisions are somewhat arbitrary and overlap in some cases; however, this mode of presentation should prove relevant and accessible by using a format to address pain complaints by region and target tissues located in the spine, extremities, head and face, autonomic nervous system, and some viscera. A discussion of the clinical use of botulinum toxin is incorporated at the end of the article.
Neural blockade and similar injection procedures often are prescribed for therapeutic benefits; however, they also can be useful for diagnostic, prognostic, or prophylactic indications, or for a combination of these purposes.
Therapeutic blocks are appropriate for alleviating acute pain, especially in a self-limiting disorder (eg, postoperative, posttraumatic, or acute visceral pain syndromes). In general, they have been advocated to alleviate acute pain or an exacerbation of chronic pain and to provide direct and localized therapeutic action, especially in patients in whom pain is accompanied by swelling and inflammation. They help the patient (1) maintain an ambulatory or outpatient treatment status; (2) maintain participation in a physical therapy or rehabilitation program; (3) decrease the need for analgesics; and (4) in some cases, avoid or delay surgical intervention.
Sympathetic blocks in causalgia and reflex sympathetic dystrophy (ie, complex regional pain syndromes) permit more effective application of adjunctive treatment techniques including physical therapy and medication. In some cases, therapeutic injections help the practitioner gain patient cooperation, which may have been compromised not only by pain but also by fear, poor nutrition, and deconditioning.
Diagnostic blocks often help the treating practitioner determine the anatomic origin(s) of the patient's pain. These procedures also may facilitate differentiation of a local from a referred somatic pain source, a visceral from a somatic pain source, or a peripheral from a central etiology. Selective blocks can help determine which peripheral tissues are primary pain generators. In cases of presumed complex regional pain syndromes, neural blockade can be used to establish relative contributions of somatic and sympathetic nervous systems.
Prognostic blocks are intended to provide information regarding the efficacy of a planned neurolytic or neurosurgical ablative procedure or potential surgical outcomes. These blocks also may help the practitioner and patient decide whether to proceed with surgery or ablative procedures.
Prophylactic blocks are used to delay and reduce postoperative pain, to prevent complications caused by posttraumatic or visceral pain, to decrease the duration of hospitalization and convalescence, and to prevent development of certain chronic pain syndromes such as autonomic dystrophy and phantom limb pain.
For patient education resources, see the patient education articles Chronic Pain, BOTOX® Injections, and Pain After Surgery.
Guidelines for Therapeutic Application
Numerous technical and medical factors are pertinent to avoid potential pitfalls or complications when considering application of injections for the many indications outlined in the introduction. Historically, these procedures have been used empirically, often resulting in variable or temporary benefit, despite risk and potential complications. For these reasons, some of the basic clinical principles for use and safety are reviewed.
Practitioner criteria
A practitioner who intends to perform therapeutic injections should be qualified by education, training, and experience to diagnose and manage the specific disorder(s) to be treated, including the capacity to determine whether diagnostic evaluation has been complete and that verification of the disorder to be treated has been conclusive. Knowledge of the natural history and expected clinical course of these disorders should influence the practitioner's judgment as to what procedure should be performed, necessity of the procedure, and likelihood of success, and lead to true informed consent.
The treating practitioner should be aware of alternative or accessory therapies that can be applied before or following procedural intervention, and which may enhance the efficacy of treatment. Knowledge of the advantages, disadvantages, and limitations of each procedure, and the ability to manage complications, should be considered requisite. Knowledge of the anatomy and pharmacology of injected substances coupled with adequate experience and technical skill for performing prospective procedures are also requisite. The practitioner should be licensed with privileges to perform therapeutic procedures in the appropriate medical care settings.
Procedural methodology
Prior to performing or even scheduling injection procedures, the practitioner is obliged to assess the patient thoroughly, including the history of the present illness, past medical history, medications, and drug allergies, and the extent to which operant and psychological factors are salient with regard to the illness at hand. Of course, all such information should be documented thoroughly.
Prior to any medical treatment, especially neural blockade or therapeutic injection, the practitioner should inform the patient fully regarding technique, indications for the procedure, operative complications, typical time for convalescence, and cost.
The patient's pretreatment status should be documented carefully. A flow sheet and medical chart to record the procedure and document any complications or side effects from pretreatment to posttreatment is standard. On-call practitioner advice and care should also be available. Any and all adverse effects, whether related to the injection or not; objective observations such as changes in temperature, color, and/or edema affecting an extremity or other pertinent body region; and assessment of therapeutic efficacy should be documented.
Digital video or still photographic documentation of the physiological appearance of the involved extremity or anatomical region and, in some cases, the procedure, provide the practitioner with a visual record of the injection locale, including any preoperative cosmetic problems such as skin lesions, scars, or deformities. Postoperative photographic recording also can be obtained for comparison.
Further objective and meaningful information can be obtained using preoperative and postoperative visual analogue scales (VAS), pain and disability scales, quality-of-life measures, and injection-specific questionnaires. The purpose and medical necessity for therapeutic injection also should be well documented. Appropriate subspecialty consultation may be necessary in some cases to support the preoperative diagnosis and the medical necessity for application of specific procedures.
Furthermore, the use of adjunctive guidance such as electromyography (EMG), ultrasound, and radiologic studies is recommended in some cases. Injections are rarely the only suggested treatment; therefore, expectations regarding the extent to which the procedure may provide pain or symptom relief should be explained to the patient preoperatively. Most therapeutic injections are not curative; therefore, any assumption that a procedure is a panacea should be dismissed.
Technical Application
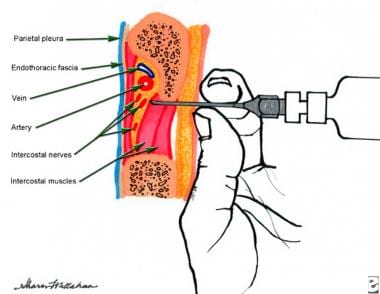
Needles and basic manipulation techniques
The application of therapeutic injections and regional anesthesia requires knowledge of equipment that includes needles, syringes, and catheters. The Luer lock is a conical tip that allows easy exchange of needle to syringe and is named after the person who developed it. Today, most needles are disposable, with the bevel cut in 3 planes to minimize tissue laceration and discomfort. Needles that are used for deep injection during regional block should incorporate a security bead on their shafts so that the needle can be retrieved if the needle hub separates from the shaft.
Generally, disposable straight needles with a beveled or pencil-point shaped tip are used for spinal interventional procedures. Spinal and deep injections are best accomplished with a styletted needle, which has an outer cannula through which a smaller needle or catheter can be inserted. The inner stylet seals the cannula and prevents tissue from entering the cannula as the needle is advanced. The stylet should always remain entirely within the cannula when there is forward movement of the needle. Many advocate the use of a short needle bevel to reduce neural and vascular trauma. [1] Rounded needle tips have been advocated for puncturing the dura to access the subarachnoid space.
In theory, rounded tips gently spread the dural fibers and may reduce the incidence of dural cuts that cause post spinal tap headaches. Caution must be exercised with long bevel needles because the soft metal tip is more likely to develop a hook or barb at the tip after striking a bony surface or with prolonged use during a procedure. Furthermore, needles with a smaller caliber (less than 20 gauge) or with a length greater than 3.5 inches are more difficult to steer through tissues of low resistance.
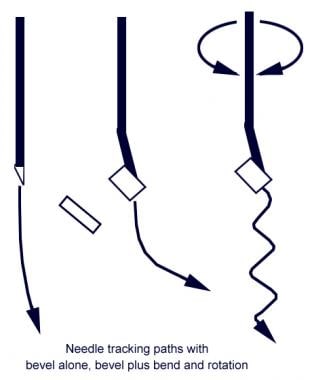
Knowing how to manage the bevel of the outer cannula and inner stylet are key to successful needle navigation. The hub of the needle usually has a notch that corresponds to the face of the bevel needle tip. After puncturing the skin, as the needle is advanced through the deeper soft tissues, the needle tip tends to veer slightly in the direction opposite to the hub notch; therefore, enter the skin as close to the target as feasible. The tendency for a needle to travel in a curved trajectory can be useful at times and can be enhanced by placing a small 5-10° bend in the tip. When traveling a significant distance with a bent needle tip, the needle must be continually rotated to prevent it from straying off course, which may cause significant tissue disruption.
To counter this potential problem, a larger coaxial needle can be placed just proximal to the target, and then if a curved trajectory facilitates steering just beyond the needle tip, a bent needle can be inserted through the larger needle, which allows it to swerve or turn in the direction necessary to reach the anatomical objective.
The needle hub is held with the thumb on top pointing toward the notch. The index and middle fingers are place opposite the thumb at the junction of the hub and needle. The needle is pushed by the thumb and can be steered by turning the notch in a direction that is 180° opposite to the target. This maneuver places the sharp edge of the needle tip toward the direction that the needle is intended to travel. The stylet should always be contained entirely within the cannula while the needle is moving forward.
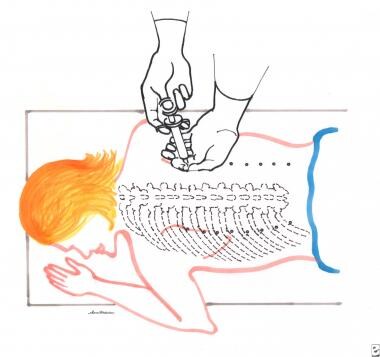
Before skin entry, the angle of the needle tip and its trajectory define its course. However, after the needle passes into deeper soft tissues, it cannot be steered by redirecting or pushing it sideways. Bowing of the needle is a technique, whereby, pressure is established both at the skin surface and at the proximal end of the needle. The needle bows toward the surface pressure. The hub is moved in a direction opposite to the notch, causing the needle to arc and the needle tip to travel in the same trajectory as the bow, opposite to the notch. Turning the hub changes the course of the needle, but always in a direction that is opposite to the bowed posture of the needle. See images below.
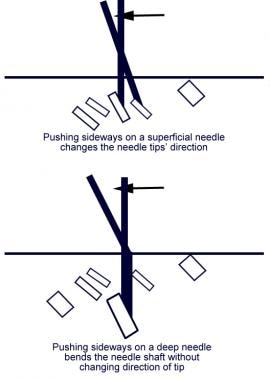 Pushing sideways on a superficial needle changes the needle tips' direction. Pushing sideways on a deep needle bends the needle shaft without changing direction of tip.
Pushing sideways on a superficial needle changes the needle tips' direction. Pushing sideways on a deep needle bends the needle shaft without changing direction of tip.
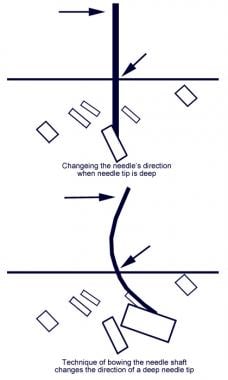 Changing the needle's direction when needle tip is deep. Technique of bowing the needle shaft changes the direction of a deep needle tip.
Changing the needle's direction when needle tip is deep. Technique of bowing the needle shaft changes the direction of a deep needle tip.
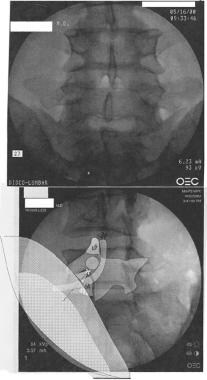
The needle should always be advanced slowly over short distances with frequent monitoring by fluoroscopy. The operating practitioner needs to be aware to move his hands out of the path of the x-ray beam when using intermittent fluoroscopy. The needle tip position can be determined by tissue feel (soft tissue vs bone), fluoroscopic visualization [lateral, oblique and AP planes] and using radiopaque contrast. Fluoroscopic localization requires an AP and lateral of the needle or one fluoroscopy view and contact with an identifiable bony landmark. Contacting bone during the procedure offers a unique opportunity to know needle tip position.
Also, when the needle tip is resting on bone, it is unlikely to be in a dangerous venue, such as a blood vessel, neural tissues, or the intrathecal space. Injection of radiopaque dye can be used to further establish certainty of the needle location. Water-soluble contrasts are benign, even when injected into the intravascular or intrathecal space; however, the presence of contrast may obscure view of the needle's tip for continued placement. The operator must know the needle tip's location before injecting any active medication. If injected radiocontrast dye washes away rapidly from the needle tip during the injection be wary, because the contrast may be entering a blood vessel. The dye should stay at the injection site. [2]
Pharmacology: Local anesthetics
The application of any injectable substance can lead to allergic, idiosyncratic, or adverse side effects. Previous suspicious or unfavorable responses may be verified through prior hospital or office records. In some cases, a small amount of the substance in question may be injected subcutaneously to test the patient's reaction to exposure.
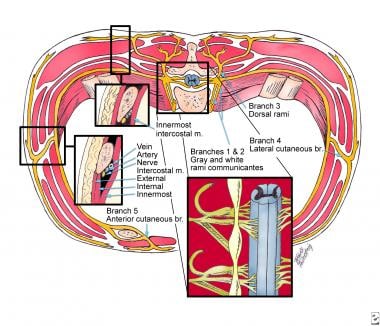
Safe and effective use of local or regional anesthesia requires thorough knowledge of the pharmacology of local anesthetics (LAs). Local infiltration for neural blockade can be accomplished by using dilute concentrations of LAs, as they rapidly penetrate the various tissues around targeted nerve endings. When large-diameter nerves are targeted, the quantity of drug reaching the central axonal core is reduced because of incomplete penetration of surrounding epineurium, perineurium, endoneurium, fat, blood vessels, and lymphatics, which can constitute as much as 40% of the peripheral nerve diameter.
Some of the injected substance is absorbed by local blood during its diffusion, which acts as another important mechanism for reducing the amount of drug that actually reaches the nerve axon. Higher concentration of LAs may cause local vasomotor paralysis, which increases local blood flow and enhances systemic absorption. Blood flow through injected tissues can be reduced by using an LA solution mixed with epinephrine, which decreases systemic absorption and improves penetration of the anesthetic to its target. Therefore, the vascularity of various tissues should be considered when deciding on the LA concentration and amount of injectate. Absorption into the bloodstream not only reduces potency of the injected material at the target site, but also increases systemic side effects. Low concentrations of LAs typically are used to block smaller, lightly myelinated and unmyelinated nerve fibers, such as C, A-delta, and B-preganglionic sympathetic fibers.
Several clinical characteristics should be considered when choosing an LA. The latency of onset of anesthetic action is an important clinical property; however, concentration, total dose, distance between the injection site and target, and relative penetrance of the compound also should be considered. Penetrance depends on target-tissue characteristics, including the thickness of superimposed, fibrous, and other intervening tissues. Tissue penetrance of specific LAs determines latency of onset and intensity of induced anesthesia. Duration of LA action depends on pharmacodynamic properties of the anesthetic, concentration, total dose, and vascularity of the region under scrutiny. LA toxicity relates to all of these factors and also to biotransformation.
All LAs have the same basic chemical structure with an aromatic and amino end joined by an intermediate chain. The amino esters use an ester link between the aromatic and intermediate chain. These drugs include cocaine, procaine, 2-chloroprocaine, and tetracaine. Cocaine was the first anesthetic used clinically and continues to be used for topical airway anesthesia because it is unique among LAs in also being a vasoconstrictor. The amino amides contain an amide link between the aromatic and intermediate chain. These medications include lidocaine, mepivacaine, prilocaine, oral pivacaine, bupivacaine, and etidocaine.
Lidocaine is a widely used LA because of its rapid onset, potency, and tissue penetration. Within this group bupivacaine is also a popular and frequently used LA for peripheral nerve block and epidural or spinal anesthesia. Commercially available concentrations of this drug range from 0.125-0.75%. Altering the concentration of bupivacaine can elicit a separate sensory or motor neural blockade, ie, lower concentrations primarily induce a sensory block, whereas higher concentrations cause motor blockade. Bupivacaine alters myocardial conduction more dramatically than lidocaine; therefore, the need for cardiorespiratory monitoring during the use of LAs should be emphasized.
Several agents are used to prolong or modify the action of LAs. As already discussed, epinephrine causes vasoconstriction, which reduces vascular and systemic absorption of the drug from the intended site of action, lowers the risk of systemic toxicity, and enhances LA efficacy on the target tissue. Epinephrine is the agent most often combined with LAs, which have a short to moderate duration of action. Epinephrine is contraindicated in some patients because of side effects or drug sensitivity or when a compromise of blood flow should be avoided (ie, when used in distal portions of the extremities, especially with coexisting peripheral vascular disease). Phenylephrine and norepinephrine (NE) also have been used as vasoconstrictors for spinal anesthesia; however, they do not appear to provide any significant advantage over the more commonly used epinephrine.
Alkalinizing agents are thought to facilitate the onset of action and prolong neural blockade when combined with LAs; however, recent double-blind studies in humans have failed to substantiate that this actually occurs. Nevertheless, addition of sodium bicarbonate to bupivacaine still is advocated to produce faster onset of epidural blockade with longer duration.
Corticosteroids
Injectable corticosteroids have been traditionally advocated to treat pain and inflammation associated with a myriad of musculoskeletal conditions, except when infection or skin breakdown is present at the target site, or in patients with poorly controlled diabetes. [3] Several therapeutic actions have been proposed for their beneficial effects. [4] They reduce inflammation by inhibiting the synthesis or release of a number of proinflammatory substances, including arachidonic acid and its metabolites (eg, prostaglandins, leukotrienes), some cytokines (eg, interleukins 1 and 6, tumor necrosis factor-α), and other acute phase reactants. [5] Other proposed mechanisms of action include a direct membrane-stabilization effect, reversible inhibition of nociceptive C-fiber transmission, and modulation of nociceptive input within the dorsal horn substantia gelatinosa neurons.
Continuous large doses of a corticosteroid adversely affect collagen synthesis, and, therefore, connective tissue strength. [6, 7] Frequency of injections and dosages must be monitored by the practitioner to prevent generalized or focal immune suppression such as infection or impaired soft tissue healing. [3] Therefore, the amount of corticosteroids that can be applied over time to a specific tissue area can be detrimental, although the exact dose/time curve remains unknown. [3] Concomitant use of medications that alter corticosteroid effects or clearance is usually not salient when injections are provided intermittently.
Practitioner preference among commonly used injectable corticosteroids is often arbitrary. Corticosteroid esters have long been preferred because of their relative safety and efficacy. The relative solubility of these solutions is considered a factor when determining the appropriate injectate. [3] Highly soluble steroids such as betamethasone sodium phosphate-acetate are rapidly absorbed and pose a lower risk for connective tissue injury, such as tendon rupture, fat atrophy, and muscle wasting. Relatively insoluble steroid esters have a longer duration of action. [3]
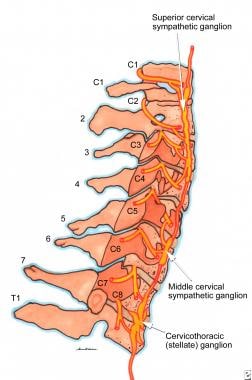
Corticosteroids are among the most commonly used active substances for spinal intervention. Particulate steroids should not be placed into the cervical foramina, because foraminal arteries, specifically the radiculomedullary artery, can be occluded by the injection. Foraminal artery occlusion is also a consideration between spinal levels T10 to L4. Particulate steroids, when injected into a foraminal spinal artery, can cause paralysis, even death. [8]
Commonly experienced adverse reactions from corticosteroid injections include dizziness, nervousness, facial flushing, insomnia, and transient increased appetite. [9] Flare-up of pain intensity at the injection site may occur, lasting for 24-48 hours in 10% of patients [9] and presumed related to a local inflammatory response to corticosteroid crystals. [3] The likelihood of a flare-up reaction is reduced by using a soluble, rapidly absorbed steroid. Rest and physical therapy are sometimes necessary in these cases. In addition, adverse reactions may occur in persons who have active peptic ulcer disease, ulcerative colitis, active infection, hypertension, congestive heart failure, renal disease, and psychiatric illness. [9]
Hyperglycemia in known diabetics warrants careful postprocedural monitoring. Other less serious side effects of corticosteroids include injection site hyperpigmentation, subcutaneous fat atrophy, peripheral edema, dyspepsia, and malaise. Systemic responses frequently occur even in local injections of corticosteroids. Allergic reactions to systemic glucocorticoids in slow-release formulations have been reported to occur up to 1 week after injection. [9]
Fluoroscopy and radiation safety
Fluoroscopy has transformed interventional pain management, not only for more precise needle placement, but also for venturing into new treatment venues, especially within the spinal canal. Precise needle placement allows practitioners to address multiple spinal pain generators with injections that include placement of radiographic contrast, local anesthetics, and corticosteroids into the epidural space, intra-articular facet joints, sacroiliac joints, and intervertebral discs. Symptomatic facet joints can be identified by median branch nerve blocks and then ameliorated with radio-frequency neurotomy or chemical neurolysis. New technologies have evolved, such as the use of spinal cord stimulators and a host of intradiskal procedures, including electrothermal coagulation, percutaneous mechanical disk decompression, laser disc decompression and radiofrequency intradiskal/annular neurolysis.
Other new treatment methods include vertebroplasty and kyphoplasty for vertebral fractures. Fluoroscopy allows more precise localization of both stellate and lumbar paravertebral sympathetic blocks, visceral sympathetic blocks, celiac plexus and superior hypogastric plexus blocks, and neurolysis of the Impar ganglion.
Several studies have demonstrated the comparative accuracy of experienced injectors and anesthesiologists using fluoroscopy compared with previous blind injection techniques and have shown a superior success rate with imaged needle guidance. [10]
Manchikanti et al advocate fluoroscopy as medically necessary for the performance of epidural corticosteroid injections. [11] Dye injection may reveal incorrect needle placement or inadequate penetration of the injectate to the level of pathology. Fluoroscopy eliminates the question of incorrect or suboptimal needle placement as compared with blind injections and can provide evidence of accurate needle positioning. Documentation of dye spread often mimics the probable flow of corticosteroids and other active medications, and therefore may correlate with the patient's response to treatment. Unintentional intravascular injection may occur during procedures despite negative aspiration through the needle. Vascular locations can be suspected when the contrast dye seems to wash away from the site of the needle tip after it is injected. Limited reasons for not using fluoroscopy include the avoidance of radiation, the cost of fluoroscopy, or allergy to contrast agents.
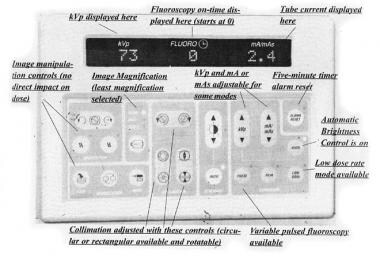
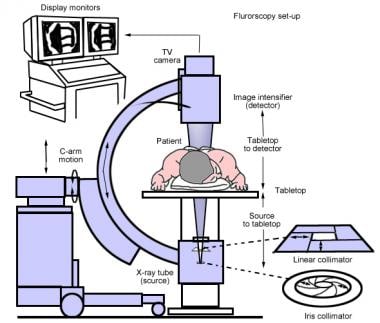
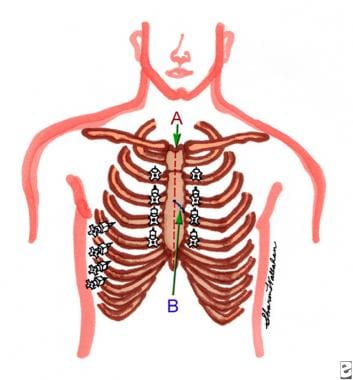
The fluoroscopy machine is primarily composed of an x-ray tube, image intensifier, C-arm, and control panel. See image below.
The electron flow, called tube current, is generated through an electrically heated negatively charged filament (cathode) and is expressed in milliamperes (mA). The x-ray tube fires a beam of electrons through a high voltage vacuum tube forming x-rays that are emitted through a small opening. X-rays are generated by engaging a high-voltage switch with the output expressed as the kilovolt peak (kVp). These x-rays pass into and through human tissue creating electrically charged ions. The image intensifier collects electromagnetic particles that pass through the patient and transforms them into a usable image that can be visualized on a television monitor. X-ray production ceases immediately when the switch is released. For this reason, radiation management in fluoroscopy is best accomplished by keeping the amount of beam-on time as short as possible. [12] See image below.
The C-arm facilitates optimal positioning of the fluoroscope for the practitioner to get the most favorable view, (eg, posterior-anterior, oblique, and lateral views of the patient). The control panel allows the technician to manually adjust the quality of the image or leave it to the automatic brightness control (ABC). The quality of the image contrast depends on the balance between the tube voltage and current. A higher kVp setting increases the penetrability of the x-ray beam, but reduces the contrast of the x-ray image, whereas the tube current increases both intensity and penetration. Balance of the tube current and tube voltage (kVp) creates the optimal contrast and image resolution.
This is usually accomplished by the ABC system, whereby the computer automatically analyzes the image contrast and makes the appropriate adjustments to the kVp and mA to achieve the best balance between contrast and brightness of the image with the lowest dose-rate to the patient. Dose-rates are greater depending on the thickness or size of the patient. As patient size increases, image quality decreases, patient dose increases, and exposure rates to personnel increase. The control panel also allows for magnification and collimation of the image. [13]
Radiation concepts and safety
X-rays are a form of electromagnetic energy. When transferred through matter, x-rays ionize human tissue and produce electrically charged ions that can induce molecular changes, potentially leading to somatic and genetic damage. Radiologic nomenclature describes radiation quantities using terminology such as the absorbed dose, effective dose, equivalent dose, and Dose-area-product. A roentgen (R) measures exposure to ionizing radiation equivalent to the electrical charge per unit mass of air (1R=2.58x10-4 coulombs/kg of air). The concentration of energy that is deposited locally into a tissue is called the absorbed dose. This is measured in units of gray (Gy) or milligray (mGy). One gray of absorbed dose is equivalent to the energy deposition of 1 joule in 1 kg of tissue mass. Doses lower than 1 Gy generally do not cause notable acute effects other than slight cellular changes.
The absorbed dose rate describes the rate of dose accumulation in mGy/min. A typical skin entrance dose rate from fluoroscopy is about 30 mGyt/min. Effective dose is the quantity of radiation exposure affecting people who are not in a stationary or typically uniform space. It is the hypothetical dose received by the entire unprotected human body and poses the same health risk as the nonuniform dose received by an individual not wearing a protective apron. For the purposes of radiation protection, regulatory limits of whole-body exposures to personnel are given in terms of effective dose. This information is extracted from the data generated by film badges or other types of personal radiation monitors.
Therefore, the radiation-absorbed dose is the amount of energy deposited into human tissue from ionizing radiation sources and is measured in Gy. Biologic effects of radiation are caused by the ionization of water molecules within the cells, producing light highly reactive free radicals that damage macromolecules of DNA. The acute effects occur at relatively high-dose levels, such as those given during radiotherapy treatments or from accidents. Chronic effects are more often the result of long-term low-dose exposure. The most common radiation-induced injuries affect the skin. Unlike a thermal burn, x-ray injuries develop slowly and may not become apparent until days or weeks later. Potential effects vary in severity from erythema to dermal necrosis and skin cancer. Additionally, the probability of induced cancer or leukemia is increased in the exposed individual. The latent period between radiation overexposure and cancer may be as short as 2 years.
To measure the effective dose (whole body dose) from occupational radiation exposure, the measure termed rad is converted to the unit of occupational exposure, which is designated as the radiation-equivalent-man (REM). The unit of dose equivalent to REM is measured by using the sievert (Sv); one REM is equivalent to 1 rad, and 100 REM is equivalent to 1 Sv. Radiation dose equivalents of 0.25 Sv (25 REM) may lead to measurable hematologic depression. Whole body total radiation doses exceeding 100 REM may lead to nausea, fatigue, radiation dermatitis, alopecia, testicular disturbance, and hematologic disorders.
A maximal permissible dose (MPD) is the upper limit of the allowed radiation dose that an individual may receive without the risk of significant side effects. The annual whole body MPD limit for physicians is 50 mSv. The annual MPD for the lens of the eye is 150 mSv, and for the thyroid, gonads and extremities it is 500 mSv. The fluoroscopy's x-ray tube should be kept as far away from the patient as possible. Federal regulations limit the maximum output for C-arm fluoroscopy to 10 R/min at 12 in (30 cm) from the image intensifier. Beam collimation reduces the area being irradiated, thereby reducing the amount of x-rays received by the patient. The use of live fluoroscopy should be minimized as much as possible. Furthermore, magnification should be limited since it increases the amount of radiation to human tissue. Image magnification by a factor of 2 increases the amount of radiation by 4 times.
Radiation exposure to ionizing radiation is unavoidable when performing fluoroscopic procedures. Only necessary personnel should be present in the fluoroscopy room. The primary source of radiation to the practitioner during such procedures is from scatter that is reflected back from the patient. Less prominent is the role of radiation leakage from the equipment. The cardinal principals of radiation protection are (1) maximize the distance from the radiation source, (2) use shielding materials, and (3) minimize exposure time. Radiation scatter can also be reduced by using the lowest tube current (mA) that is compatible with a good x-ray image. In conventional fluoroscopy, the x-ray tube is located beneath the table and the image intensifier is above the table.
With a horizontal table, in this arrangement, most of the radiation scatter is in a downward direction and is absorbed into the floor or side panels of the table. In the opposite arrangement, it is often difficult to get adequate shielding to medical personnel. As mentioned, the beam-on time is the most important variable for controlling radiation exposure and should be kept to a minimum; most fluoroscopy machines are armed with a 5-minute alarm.
X-ray shielding can be fixed or mobile, including the commercially available protective apparel. Fixed shielding includes the thickness of walls, doors, and protective cubicles, which should have a lead equivalent of 1-3 mm. Mobile shielding is appropriate during fluoroscopy when a member of the staff needs to remain near the patient. Specific items of apparel that are used for personal shielding include lead aprons, gloves, thyroid shields, and glass spectacles.
Typically, practitioners and assisting personnel are supplied with monitoring equipment in the form of a radiation or film badge that is packed with photographic film. These clips are typically light and slim for convenient placement on conventional clothing and apparel. Usually a "color badge" is worn outside the apron on the upper portion of the body, usually on the upper edge of the thyroid shield. This badge approximates radiation exposure to the lens of the eye. A second "behind the apron" badge is worn underneath lead apparel and clipped onto the waist of the practitioner. X-ray readings from this badge represent the actual dose to the gonads and major blood-forming organs.
Also, a finger or ring badge can be worn with the film facing the underside part of the hand nearest the radiation source. Badges may also be placed on protective eyewear. These badges are usually processed monthly to monitor the type and amount of radiation exposure received by each clinical participant. Results are reported as monthly and 12-month accumulated dosages. Prompt exchange of badges on a monthly basis is required in most medical facilities.
Radiocontrast agents
Radiographic contrast agents aid in the localization of anatomical structures. Iodine atoms within these agents provide greater x-ray attenuation compared with human tissues, including bone. Osmolality describes a measure of the numbers of particles in a specific solution. The hyperosmolality of contrast agents relates directly to their toxicity. Second-generation radiocontrast agents have more physiologic properties, are labeled nonionic, and are more commonly used for spinal injections. The 2 most commonly used radiocontrast agents are iopamidol (Isovue-M) and iohexol (Omnipaque). Both are absorbed rapidly into the bloodstream from intrathecal, epidural, and paraspinal tissue injections.
Plasma levels are measurable within an hour after injection. The mean half-life is 12 hours and 80-90% is excreted via the kidneys within 24 hours with minimal excretion via fecal route. Adverse reactions may be chemotoxic, osmolar-related, or allergic. Also, 90% of adverse effects occur within 15 minutes of exposure.
If an allergic reaction is suspected, patients should be observed for up to 60 minutes. The primary concern when using contrast media is unintentional intrathecal injection. For this reason, the above-mentioned water-soluble contrast media are recommended: iohexol (Omnipaque) or iopamidol (Isovue). Radiologic contrast media are not licensed for intrathecal use, but these 2 specific radiocontrast agents have not been reported to cause adhesive arachnoiditis and exhibit a low risk of seizures and neurotoxicity.
Patients at greater risk for an adverse reaction to radiocontrast media include those with a history of a previous adverse reaction, especially allergy. Any question regarding an allergic reaction can be avoided by giving oral prednisone 20-50 mg, ranitidine 50 mg, and diphenhydramine 25-50 mg orally 12-24 hours prior to exposure by injection. An additional 25 mg of diphenhydramine can be given by IV immediately before contrast injection. Further caution is required when administrating radiocontrast to patients with asthma; allergy/atopy; cardiac disease with decompensation, unstable arrhythmia, or recent MI; renal failure/nephropathy; feeble individuals with general debility (especially infants or the elderly); and patients with dehydration, metabolic disorders, or hematologic disorders.
Adverse reactions vary from chemotoxic reactions (such as thyrotoxicosis or nephrotoxicity) hyperosmolar responses, or more typical allergic responses characterized by vasomotor responses, cutaneous reactions, bronchospasm, cardiovascular effects (hypotension), or anaphylactoid reactions.
Although fluoroscopy has revolutionized the precise and accurate practice of interventional pain management, radiation safety training is required for any practitioner who uses fluoroscopy in his practice. Furthermore, injectable radiocontrast media and active therapeutic agents require additional knowledge. Practice in this area of subspecialty requires additional training through recognized medical certification agencies or societies. [14]
Although, fluoroscopy has revolutionized pain management by increasing the precision, safety, comfort, and outcomes of interventional techniques, the number of procedures and providers has increased.
All practitioner interventionalists must be adequately trained and experienced to prevent adverse events from harming patients and coworkers. Radiation safety training is required for any practitioner who uses fluoroscopy. Furthermore, injectable radiocontrast media and active therapeutic agents require additional knowledge. Practice in this area of subspecialty can be readily attained through additional training sponsored by reputable medical certification agencies or societies.
All somatic and spinal injection practices carry finite plausible risks that include medication allergies or side effects, unwanted violation of body structures with neural or vascular content, and the ultimate possibility of death as a treatment outcome. Complications that are common or unique to each procedure are discussed below. However, this article is intended only to provide information and not the skill, knowledge, mentoring, and experience necessary to perform the interventional methods outlined below.
University and other American Board of Medical Specialties (ABMS)-accredited fellowship programs are now commonly offered. Pain societies and certification agencies such as the American Board of Anesthesia and the American Society of Interventional Pain Physicians provide learned guidelines, assistance through teaching and coursework, and board certification examinations for physician interventionalists. Expertise in performing the outlined procedures is a matter of forethought, not afterthought.
Adverse Effects and Complications of Neural Blockade
Systemic toxic reactions to LAs can result from high blood levels of the drug due to accidental intravenous (IV) infusion of all or part of the therapeutic dose, injection of an excessive amount of drug, or abnormal rates of absorption and biotransformation of the drug. Typically, these reactions demonstrate a combination of cardiovascular, respiratory, and central nervous system side effects that range from mild to severe.
Mild reactions occur when systemic blood levels of LA rise above the usual physiologic levels. Patients may experience dizziness, vertigo, tinnitus, headache, anxiety, tachycardia, hypertension, tachypnea, dysarthria, metallic taste, and nausea.
Moderately severe reactions are manifested by abnormal mental status including somnolence, confusion, and sometimes loss of consciousness. Muscular twitching may progress to generalized motor seizures and usually is accompanied by hypertension and tachycardia that require immediate practitioner action with particular attention to proper ventilation.
Severe toxic reactions from marked overdoses of LA usually are evinced by rapid loss of consciousness with hypotension and brachycardia. Respiratory depression and arrest may accompany other signs of severe central nervous system and cardiovascular depression. If prompt treatment is not instituted, progression to complete respiratory and cardiovascular failure with death may result.
Whenever a systemic toxic reaction is suspected, oxygen administration is justified to reduce the risk of hypoxia. With recurrent seizures, a patent airway must be maintained, including tracheal intubation and artificial ventilation when necessary. Small doses of fast-acting anticonvulsant agents, such as diazepam or lorazepam, can be considered when seizures are recurrent without interictal recovery of consciousness or for continuous seizure activity lasting more than 20 minutes. Cardiovascular monitoring is essential, coupled with appropriate fluids and medication support. Other undesirable systemic reactions to local and regional analgesia include psychogenic reactions, which often are highlighted by fear and anxiety prior to the procedure.
During or after the procedure, patients may experience light-headedness, tinnitus, hyperhidrosis, tachycardia, skin pallor, hypotension, and even syncope. Any adverse reactions should be observed carefully to ensure that symptoms are not due to toxicity or allergy. Management consists of placing the patient into a recumbent position, administering oxygen, and monitoring blood pressure. In some cases, judicious IV infusion of ephedrine may be necessary to alleviate hypotension. Not infrequently, epinephrine in an LA solution can contribute to uncomfortable or adverse side effects, including apprehension, palpitations and tachycardia, dizziness, diaphoresis, and skin pallor. If severe hypertension develops, then treatment with vasodilators or other hypotensive agents is appropriate.
Allergic reactions can occur following repeated exposure to specific LAs and are characterized by urticaria, arthralgia, and edema of eyelids, hands, joints, and larynx. Severe laryngeal edema requires prompt attention to maintain airway patency and may necessitate emergency tracheostomy. Although rare, idiosyncratic reactions may result in sudden and rapid cardiovascular and respiratory collapse leading to death. Treatment includes prompt establishment of an airway, artificial ventilation, oxygen administration, cardiac monitoring, and medication support with vasopressors.
Neurological complications may result from systemic reactions or be due to specific procedures. For example, injuries to peripheral nerves may result from direct trauma including localized hematoma, compression by tourniquet, unintentional neural traction, compression due to positioning, or injection of an excessively high concentration of LA. Complications following subarachnoid or epidural injections can result from direct spinal cord or nerve root trauma, spinal cord compression by hematoma, or spinal cord ischemia.
Direct neural damage is most often reported with brachial plexus blocks. Direct intraneural injection often is attributed to the practitioner's negligence or lack of skill but can occur with highly skilled and experienced interventionists. Needles with a low bevel angle (< 45°) may contribute to a lower incidence of such complications. Postblock neuropathy can occur immediately after the block or within the first 7 days; however, recovery is common over the ensuing 2-3 months.
Accidental injection of LA into the subarachnoid space sometimes complicates paravertebral blocks aimed at addressing somatic or sympathetic neural structures, such as the stellate ganglion. If the level of anesthetic-induced spinal cord dysfunction is as high as C4, respiratory support, including artificial ventilation, may be necessary. Occasionally, withdrawal of 10-15 mL of cerebrospinal fluid (CSF) reduces CSF concentration of the misplaced LA. Hypotension also can result from unintentional extensive subarachnoid or epidural blockade, or in some cases, from paravertebral sympathetic or celiac plexus blockade.
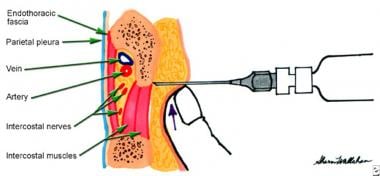
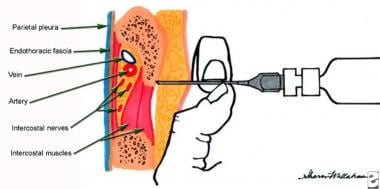
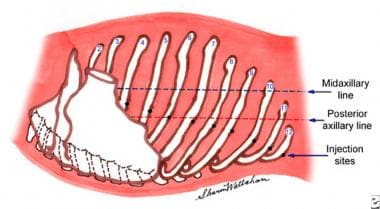
Pneumothorax is a potential complication from thoracic paravertebral, supraclavicular brachial plexus, intracostal, and celiac plexus blocks. Occasionally, trapezius and other apically directed intramuscular injections also might lead to pneumothorax. Symptoms can develop within minutes but more often develop over several hours. Frequently, patients who experience injections that violate the respiratory space complain of tasting the anesthetic followed by hoarseness. Radiographic evaluation is obligatory in cases in which this complication is suspected.
Injection site hematomas are usually minor complications associated with the use of large needles having a dull bevel or hook, except in patients with a bleeding disorder or taking anticoagulant medications. Diagnosis is usually evident by subcutaneous extravasation of blood, and in some cases, neural deficit, which may be slow to resolve. In cases of localized hematoma, initial use of ice and pressure is warranted to slow or stop the bleeding. Occasionally, this complication may require ultrasound or other imaging studies to document the size and location of the hematoma.
Commonly Practiced Neural and Structural Blocks
Several somatic and peripheral neural blockade procedures are useful for therapeutic and diagnostic purposes. Although the opportunity to block specific nerves can be considered limitless in the hands of an experienced interventionist with appropriate radiographic guidance, only some of the available procedures are mentioned below to highlight their usefulness as potential tools for a neurologist involved in the diagnosis and treatment of pain.
Therapeutic injections for extra-axial soft tissue structures
Therapeutic injections frequently are used as a mode of treatment in general or subspecialty practices, especially orthopedics, physiatry, and rheumatology. Many musculoskeletal disorders respond amenably to injections, including intra-articular and extra-articular tissues of many synovial joints, bursae, muscles, and tendons. Pain from extra-axial articular structures often is managed best by the aforementioned subspecialists.
Understanding a few key principles can help the neurologist determine the structural anatomy of an articular pain syndrome and respond efficiently by specialty referral, especially when certain symptoms indicate a potentially serious etiology. In most cases, patients with generalized arthralgia and arthropathy should be referred to a rheumatologist; therefore, this article concentrates primarily on localized pain disorders. In fact, the neurologist often is asked to differentiate whether pain is localized to a joint or periarticular structures or is referred from diseased neural structures.
Pain referral from joints or other soft tissue structures typically does not assume a myotomal or dermatomal pattern. Pain arising from superficial soft tissue structures that can be identified by palpation often permits more precise localization of the causative tissue or structure. However, pain that is referred from extra-axial joint capsules and other periarticular structures, such as ligaments, tendons, bursae, and muscles, may be more difficult to differentiate. Pain from bone and periosteum is usually well localized and rarely radiates; however, this discrepancy between "soft" and "hard" structures remains unexplained.
The manner in which the pain from symptomatic joints responds to biomechanical stressors is often the key to localization and causation. Pain that is worse when the joint is used suggests a mechanical etiology, especially if improved with rest. Pain in bed at night should bring about concern for a serious underlying etiology and almost always requires investigation. Persistent pain that does not fluctuate despite activity or rest is also worthy of diagnostic inquiry. Psychogenic or operant pain frequently is described as continuous and often more intense and disabling with certain activities, eg, worse at work and better with recreation. Pain and stiffness that are present in the early morning or after inactivity may be a harbinger of inflammatory arthropathy in extra-axial and axial joints. Patients with monoarticular deformity, swelling, stiffness, and warmth should be referred to the appropriate musculoskeletal specialist for evaluation.
Many common afflictions of extra-axial soft tissue structures are amenable to management by a neurologist who is skilled in the evaluation and treatment of musculoskeletal disorders. Bursae are fluid-filled sacs that facilitate smooth movement between articulating structures. Subcutaneous bursae, such as the olecranon and prepatellar bursae, form in response to normal external friction. Deep bursae, such as the subacromial bursa, form in response to movement between muscles and bones and may or may not communicate with adjacent joint cavities. "Adventitious" bursae form in response to abnormal shearing stresses (eg, over first metatarsal head) and are not uniformly present.
Acute or subacute bursitis (most often affecting subacromial, subscapular, prepatellar, and trochanteric bursae) frequently presents with severe disabling pain that can be relieved promptly by injection of LA. Depending on the size of the targeted bursa, a dilute solution of bupivacaine (0.25-05%) with epinephrine 5 mg/mL, with 40 mg of methylprednisolone (Depo Medrol) or an equivalent corticosteroid (ie, Celestone), is often dramatic in its effect. If the bursa is swollen and contains fluid, aspiration should be performed prior to injection for laboratory studies including cultures for a possible infectious agent.
Tendons act as functional anatomical bridges between muscle and bone. Tendinitis is also a common cause of outpatient evaluation for moderately severe to severe, often disabling, pain. Among the most frequent syndromes are bicipital tendinitis, lateral epicondylitis (tennis elbow), medial epicondylitis (golfer's elbow), and supraspinatus (rotator cuff) tendinitis. Long-acting LAs, such as bupivacaine, coupled with a long-acting corticosteroid are often effective. Repeated use of corticosteroids may risk toxicity to the soft tissues, and long-term use can result in adverse systemic effects that are associated with Cushing syndrome. Occasionally, patients experience a "steroid flare" and develop increased pain in the injection site over 24-48 hours; however, local beneficial effects usually follow after the flare resolves. Exercise and physical modalities, including ice and heat, are fitting adjuncts. LA infiltration alone without corticosteroids can be repeated until permanent benefit is achieved.
Muscle spasm and myofascial pain (ie, trigger points) and treatment of syndromes considered controversial by some, such as that caused by the piriformis and scalene muscles (thoracic outlet syndrome), are other commonly considered indications for injection treatment. The tenets of managing these syndromes must be emphasized, however; therapeutic injections are considered adjunctive to an overall treatment plan that includes postural correction, ergonomic modification of contributory occupational factors, appropriate strengthening and flexibility exercises, and concomitant use of physical modalities.
Painful scars following injury or surgery also may be associated with pain and hyperesthesia. Infiltration of LA, sometimes accompanied by corticosteroids, has been reported to be beneficial in many cases. Concomitant topical or oral agents may be useful, as well as application of transcutaneous electrical stimulation (TENS).
Neuromata can develop in nerves that are entrapped subsequent to traumatic neurosection or following surgery for amputation. Infiltration with LA is useful not only from a therapeutic standpoint but also diagnostically. LA without epinephrine mixed with a depot corticosteroid can suppress spontaneous ectopic discharges suspected of producing pain and paresthesia. Supplemental treatment with anticonvulsants may improve outcome if relief is incomplete.
Intra-articular injections of a dilute solution of LA, usually in combination with corticosteroids or articular lubricating agents, frequently are advocated for severe pain associated with chronic degenerative arthritis, especially in weight-bearing joints. Intra-articular injection of LAs into spinal facet joints is discussed in a later section of this article; however, injection of extra-axial joints is considered beyond the scope of the primary theme and the audience addressed in this article.
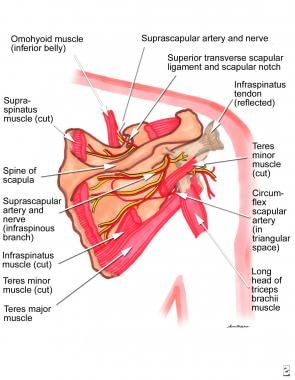
Suprascapular nerve block
The suprascapular nerve branches from the brachial plexus and serves as the primary sensory supply for the shoulder joint. Suprascapular nerve block can be helpful for the management of severe pain caused by bursitis, periarthritis, or arthritis when intra-articular and periarticular injection of LA and steroids are contraindicated, ineffective, or to be avoided.
Suprascapular nerve block provides anesthesia to the shoulder joint, which allows physical therapy to implement improved range of motion caused by adhesive capsulitis or excessive periarticular muscle guarding. Technically the procedure is easy to perform; however, satisfactory blockade is not achieved uniformly in all cases. When blockade is inadequate, concomitant use of radiography or a peripheral nerve stimulator can provide more accurate placement of the needle and improve anesthetic administration.
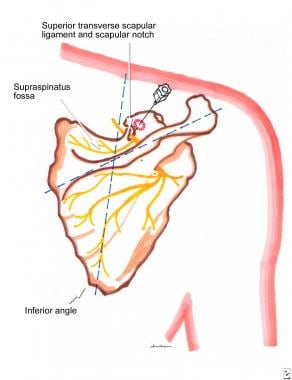
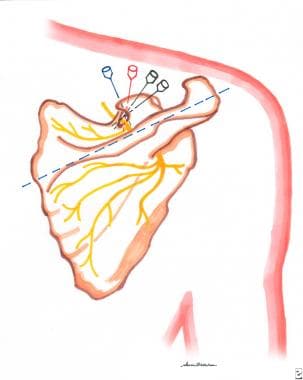
To perform a suprascapular nerve block, the practitioner locates the suprascapular notch by first forming 2 bisecting lines—one extending along the spine of the scapula and another that bisects this line and extends to the inferior angle of the scapula.
Using the technique advocated by Bonica, an 8-cm, 22-gauge needle is introduced through a skin wheal of LA placed in the outer triangle about 1.5 cm from the bisection point. The shaft of the needle is directed anteriorly, caudally, and medially into the supraspinatus fossa just lateral to the suprascapular notch. The needle is withdrawn until its point lies within the subcutaneous tissue and then re-introduced to a point that is approximately 5 mm medial to the first contact. The needle should enter the notch; contact with the nerve is verified if paresthesia is evoked. If no paresthesia is elicited, sequential insertions may be necessary, or location of the nerve can be facilitated by electrical nerve stimulation.
Bupivacaine (3-5 mL) or other long-acting LA, in addition to a short-acting LA, should provide an adequate block for diagnostic purposes, and thereafter, allow appropriate physical therapy intervention.
See the images below.
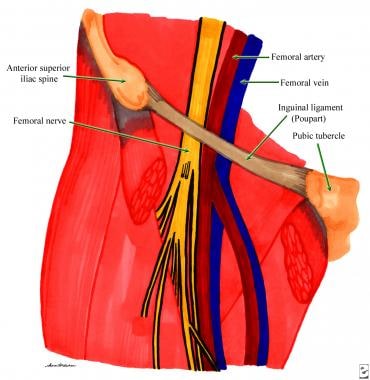
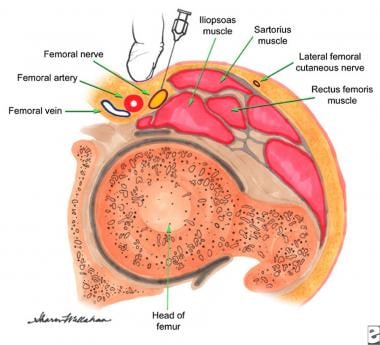
Femoral nerve block
Femoral nerve block just below the inguinal ligament can be used as a diagnostic tool in patients who present with anterior thigh pain or can be combined with a sciatic nerve block to produce sympathetic neural blockade of the lower extremity. Femoral nerve block can alleviate severe pain related to posttraumatic or postoperative causes (eg, fracture of the neck of the femur).
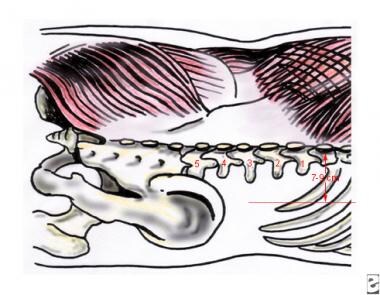
Using the technique described by Bonica, this procedure is performed with the patient in a supine position. The midpoint of a line joining the anterosuperior iliac spine and pubic tubercle usually overlies the femoral artery. A short-acting LA is used to raise a skin wheal approximately 1 cm lateral to the junction of the femoral artery in the inguinal ligament. See the images below.
While palpating the artery under the second finger of the left hand, a 5-cm, 22-gauge or 25-gauge, short-beveled needle is introduced with the right hand through the skin wheal and is perpendicularly advanced through the skin until paresthesia is elicited in the distribution of the femoral nerve, preferably by using an electrical nerve stimulator or ultrasound for guidance. Usually 8-10 mL of 1% lidocaine with epinephrine produces analgesia for 3-4 hours, whereas the same volume of 0.25% bupivacaine with epinephrine produces analgesia for 6-8 hours. If longer analgesia is required, the concentration of bupivacaine can be increased to 0.5% with epinephrine or a continuous block can be applied by placing an infusion catheter at the site.
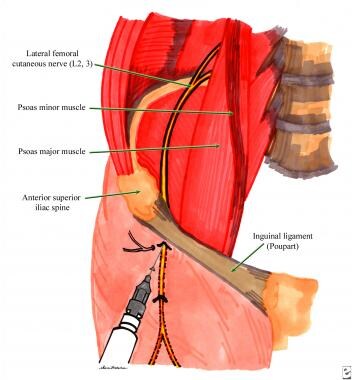
Lateral femoral cutaneous nerve block
A lateral femoral cutaneous nerve block confirms the presumptive diagnosis of lateral femoral cutaneous neuralgia or meralgia paresthetica and may provide symptomatic relief. Using the technique described by Bonica, a 5-cm, 22- or 25-gauge, short-bevel needle is introduced through a skin wheal of 1% lidocaine that is 1.5 cm caudal to the anterosuperior iliac spine just below the inguinal ligament at an angle of approximately 60° to the skin. See the image below.
Usually a volume of 5-8 mL of LA is required; addition of corticosteroids may produce therapeutic relief for meralgia paresthetica. Oral medications (tricyclic antidepressants or anticonvulsants) can be added for improved pain relief.
Sciatic nerve block
The sciatic nerve is derived from the L4, L5, and the S1-S3 nerve roots; these nerve roots become enjoined on the anterior surface of the piriformis muscle. The nerve then travels inferiorly and leaves the pelvis just below the piriformis muscle via the sciatic notch. The sciatic nerve lies anterior to the gluteus maximus muscle and is halfway between the greater trochanter and the ischial tuberosity. The sciatic nerve courses downward past the lesser trochanter to lie posterior and medial to the femur. In the mid thigh, the nerve gives off branches to the hamstring muscles and the adductor magnus muscle. In most patients, the nerve divides to form the tibial and common peroneal nerves in the rostral popliteal fossa.
A posterior sciatic nerve block is useful for evaluation and management of distal lower extremity pain that is thought to be caused by the sciatic nerve. Sciatic nerve block with local anesthetic can be used during differential neural blockade to determine the anatomy of distal lower extremity pain. If destruction of the sciatic nerve is considered, this technique is sometimes useful as a prognostic indicator of the degree of motor and sensory impairment that the patient may hope to experience.
In some cases of acute pain, sciatic nerve block with local anesthesia may be used to provide urgent relief. Examples of this clinical scenario include distal lower distal extremity fractures or trauma. Sciatic nerve block can alleviate pain while waiting for other pharmacologic methods to become effective. Sciatic nerve block combining local anesthetic and corticosteroids is occasionally used to treat persistent distal lower extremity pain that is thought to be secondary to inflammation or when entrapment of sciatic nerve by the piriformis muscle is suspected. Destruction of the sciatic nerve is occasionally indicated for palliation of persistent distal lower extremity pain secondary to malignancies.
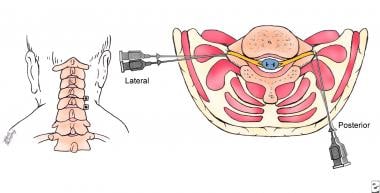
A posterior sciatic nerve block into the subgluteal region is usually performed with the patient in a lateral decubitus position with the top leg flexed. Ultrasonography-guided needle placement enhances safety and provides more accurate needle position. In these cases, the ultrasound transducer is placed in the subgluteal region midway between the greater trochanter and ischial tuberosity. After the sciatic nerve is located, the skin is infiltrated with local anesthetic, a 22-gauge needle that is 10-12 mm long or a 25-gauge, 3.5-inch needle is directed in a perpendicular plane.
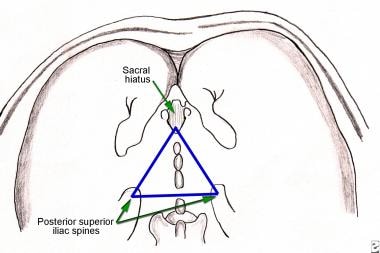
Needle movement can be ultrasound guided or may be gently and slowly advanced until it elicits paresthesia. If bone is encountered prior to paresthesia, the needle is redirected along a line joining the sacral hiatus and the greater trochanter. During redirection, the needle is steered deeper, not to exceed 2 cm.
Once paresthesia is elicited in the distribution of the sciatic nerve, the needle is withdrawn 1 mm, and the patient is observed to rule out any persistent paresthesiae. Further guidance and confirmation of tip placement can be obtained using electrical nerve stimulation. If a nerve stimulator is used, dorsiflexion and plantar flexion of the foot are noted. If paresthesiae resolve and careful aspiration is unrevealing, then 20-25 mL of 1% preservative-free lidocaine can be slowly injected.
If the pain has an inflammatory component, then the local anesthetic can be combined with 80 mg of methylprednisolone that is incrementally injected. Subsequent daily nerve blocks can be carried out in a similar manner substituting 40 mg of methylprednisolone before the initial 80 mg dose. Pressure should be applied to the injection site to decrease the incidence of postblock ecchymoses and hematoma formation.
The primary side effects from sciatic nerve block have been mentioned and include ecchymoses and hematoma. Maintaining pressure at the injection site can usually avoid this complication.
The sciatic nerve can also be blocked anteriorly in patients who cannot assume the Sims or lithotomy position because of lower extremity trauma. This is also a useful technique when the clinician desires performance of a combination of nerve blocks for the lower extremity, perhaps also including the lateral femoral cutaneous, femoral, and obturator nerves, and in some cases, the lumbar plexus.
The anterior approach requires that the patient is positioned in supine with the leg in a neutral position. The greater trochanter and the crease of the groin on the involved side are identified by palpation. An imaginary line is then drawn parallel to the crease of the groin that runs from the greater trochanter to the center of the thigh. This center point is then identified and prepared with antiseptic solution. A 25-gauge, 3.5-inch needle is then slowly advanced perpendicular to skin until it impinges on the femur. Again, nerve stimulation techniques can be used as described for guidance.
When the needle reaches the bony surface of the femur, it is then walked slightly superiorly and medially off the top of the lesser trochanter. When the sciatic nerve is reached, paresthesia is elicited; if a nerve stimulator is used, dorsiflexion and plantar flexion of the foot is elicited. The patient should be warned prior to stimulation or paresthesia so that they respond immediately. Paresthesia is usually elicited at a depth 1 inch beyond initial body contact. Once the needle elicits paresthesia, it is withdrawn about 1 mm. If paresthesia is not persistent and aspiration is negative, then as much as 20 mL of 1 % preservative-free lidocaine can be slowly infused. Methylprednisolone can be added to treat an inflammatory component, similar to that described with the posterior approach.
In some cases, physicians choose to block the tibial and peroneal branches of the sciatic nerve at the popliteal fossa. By definition, the popliteal fossa is defined cephalically by the semi-membranosis and semi-tendinosis muscles medially and the biceps femoris muscle laterally. Its caudal extent defined by the gastrocnemius muscle both medially and laterally. If this quadrilateral is bisected, as shown in the image below, the clinically pertinent area would be the cephalolateral quadrant.
Here, both tibial and common peroneal nerve blockade is possible. The tibial nerve is the larger of the 2 and separates from the common peroneal nerve at the upper limit of the popliteal fossa. The tibial nerve continues the straight course of the sciatic nerve, running lengthwise through the popliteal fossa directly under the popliteal fascia between the heads of the gastrocnemius muscles. With the patient prone, the patient is asked to flex the leg at the knee, which allows more accurate identification of the popliteal fossa.
When identified, it is divided into equal medial and lateral triangles as shown in the image below.
A mark, such as “X,” is placed 5 cm superior to the skin crease of the popliteal fossa and 1 cm lateral to the midline of the triangles. A 22-gauge, 4-cm to 6- cm needle is directed at a 45-60 degree angle to the skin, and then the needle is advanced in an anterior and superior direction. Paresthesia is sought and if obtained 38-48 mL of local anesthetic is injected. Potential problems include vascular obstructions that also occupy the popliteal fossa. Intravascular injections should occur infrequently when proper precautions and technique are used. In these cases ultrasound guidance and nerve stimulation may be helpful.
Occipital nerve blocks
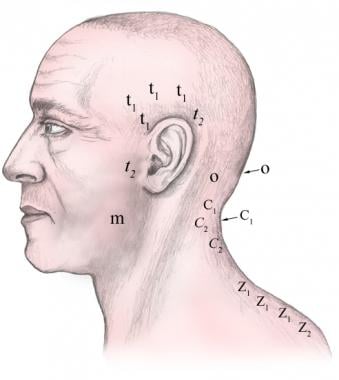
Occipital nerve block can be applied for diagnostic, prognostic, and therapeutic purposes in patients with headache, neuralgia, and other painful conditions of the posterior aspect of the head. Using the technique described by Bonica, the greater occipital nerve is blocked by needle placement just above the superior nuchal line and approximately 2.5-3 cm lateral to the external occipital protuberance. If reaching the nerve and eliciting paresthesia are difficult, then 5 mL of LA can be injected on the medial side of the artery, 2 mm superficial to the skull. Frequently, care must be taken during this block not to allow anesthetic fluid to spread laterally, as it may affect the glossopharyngeal nerve, causing hoarseness and difficulty in swallowing. See the image below.
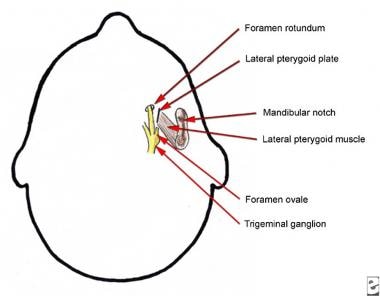
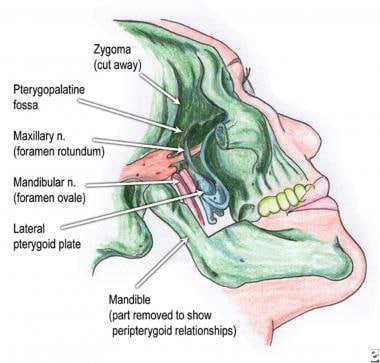
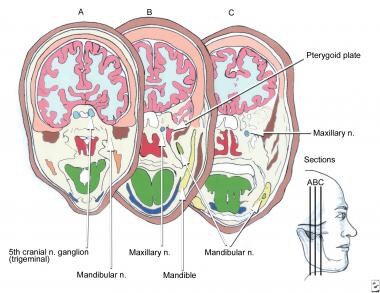
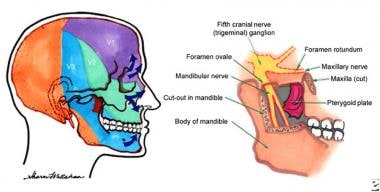 Anatomy of the fifth cranial nerve ganglion (trigeminal) along with innervation and peripterygoid relationship.
Anatomy of the fifth cranial nerve ganglion (trigeminal) along with innervation and peripterygoid relationship.
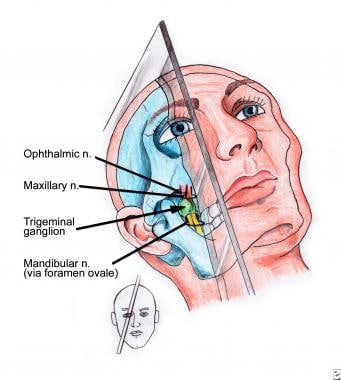
Trigeminal nerve blocks
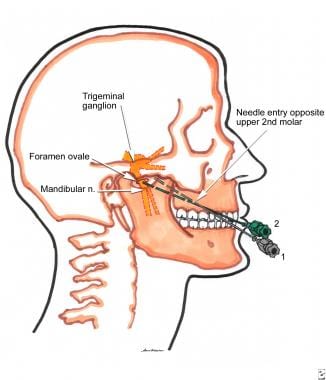
Trigeminal ganglion block commonly is used for diagnostic and prognostic purposes when considering trigeminal neurolysis for patients with trigeminal neuralgia. The trigeminal ganglion is located intracranially, situated lateral to the internal carotid artery and cavernous sinus and posterosuperior to the foramen ovale.
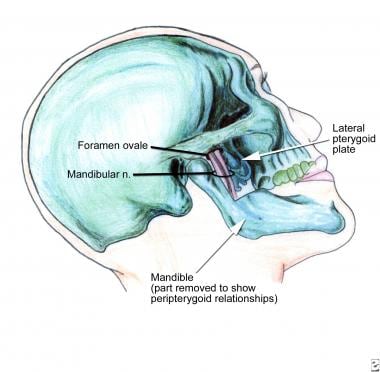
The foramen ovale is approximately 1 cm in diameter and serves as the cranial opening through which the mandibular nerve exits; it lies approximately in the same horizontal plane as the zygoma at the level of the mandibular notch, immediately dorsolateral to the pterygoid process. See the images below.
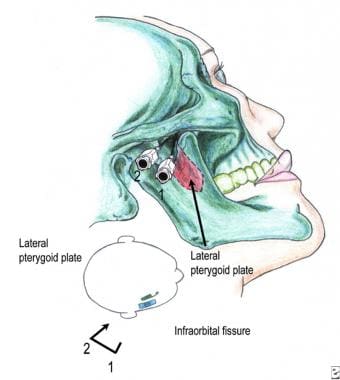
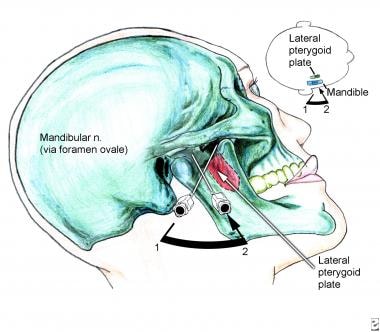
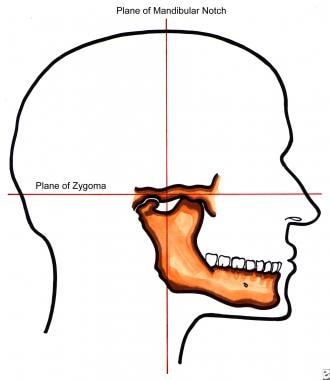 Lateral view of mandibular notch and plane of zygoma. Correlate with cross-sectional view of the fifth cranial nerve (trigeminal) ganglion and foramen ovale.
Lateral view of mandibular notch and plane of zygoma. Correlate with cross-sectional view of the fifth cranial nerve (trigeminal) ganglion and foramen ovale.
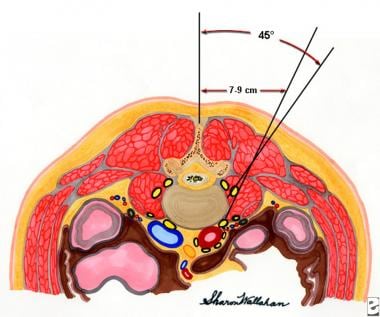
Trigeminal ganglion blockade should be performed only by skilled and experienced interventionists. Using the technique described by Brown, the patient is placed in a supine position. See the images below.
A 22-gauge, 10-cm needle is inserted through a skin wheal approximately 3 cm lateral to the corner of the mouth and medial to the masseter muscle in a direction that bisects the plane formed by the midpoint of the pupil with the patient staring at the ceiling. This allows the needle tip to contact the infratemporal surface of the greater wing of the sphenoid bone, immediately anterior to the foramen ovale at a depth of 4.5-6 cm.
Once the needle is positioned firmly against this bony target, it is withdrawn and redirected in a stepwise manner until it enters the foramen ovale at a depth of about 6-7 cm, approximately 1.5 cm beyond the initial needle length required to contact the bone. As the foramen is entered, paresthesia in the mandibular distribution usually is evoked. Further slight and careful movement of the needle may elicit paresthesia in the distributions of the ophthalmic and maxillary nerves. These additional paresthesiae verify a periganglionic placement of the needle tip.
Aspiration should be performed first to check for CSF because the posterior two thirds of the trigeminal ganglion is enveloped in the reflection of the dura. One milliliter of a short-acting LA then can be injected. If neural blockade is incomplete after 5-10 minutes, an additional 1-2 mL of LA can be injected or the needle can be repositioned to obtain a more complete block. The most concerning complication with this procedure is subarachnoid injection. Moreover, because the needle passes through a highly vascular region, hematoma formation is a possibility.
Maxillary nerve blockade also can be useful for diagnosis and treatment of facial neuralgia. The maxillary nerve is entirely sensory and exits through the foramen rotundum. Using the technique described by Brown, the patient is placed in supine position with the head and neck rotated away from the side to be blocked. See the images below.
A 22-gauge, 8-cm needle is inserted through the mandibular notch and advanced in a medial and cephalad direction until it meets the lateral pterygoid plate at a depth of approximately 5 cm.
The needle is then withdrawn and redirected in a stepwise manner by walking the bevel off the pterygoid plate, to a depth 1 cm beyond initial contact, until it lies within the pterygopalatine fossa. Once the needle rests in a satisfactory position, 5 mL of LA is injected. Because of the maxillary nerve's proximity to the infraorbital fissure, LA may spill into the orbit and affect eye movement or vision. Because the vascularity of this region is rich, hematoma formation is a possible complication; some subjects may develop a black eye following this block, again because of the close proximity of the orbit.
Mandibular nerve block is similarly useful for diagnosis and treatment of facial neuralgia. The mandibular nerve is primarily a sensory nerve and exits the cranium through the foramen ovale, traveling parallel to the posterior margin of the lateral pterygoid plate, then descending inferiorly and laterally toward the mandible. See the images below.
The anterior division of the mandibular nerve is principally motor and supplies the muscles of mastication, whereas the posterior division is principally sensory and supplies the skin and mucous membranes overlying the jaw and skin anteriorly and superior to the ear.
The Brown technique for performing this block begins with the patient in supine position with the head and neck turned away from the side to be blocked. See the image below.
The patient is asked to open and close the mouth gently so that the operator can identify and palpate the mandibular notch. A 22-gauge, 8-cm needle is inserted in the midpoint of the mandibular notch and directed at a slightly cephalad and medial angle through the notch to the lateral pterygoid plate at a depth of approximately 5 cm. The needle is then withdrawn to a subcutaneous position and carefully walked off the posterior border of the pterygoid plate in a horizontal plane. The needle should not be advanced more than 0.5 cm past the depth of the pterygoid plate because the superior constrictor muscle of the pharynx can be pierced easily. When the needle is in appropriate position, 5 mL of LA can be administered. Complications include hematoma formation and subarachnoid injection.
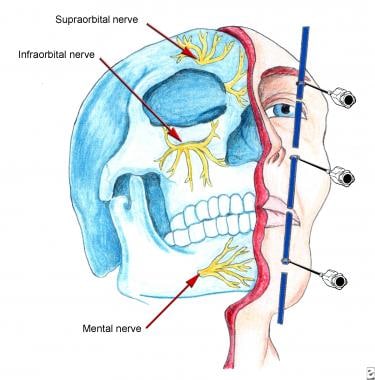
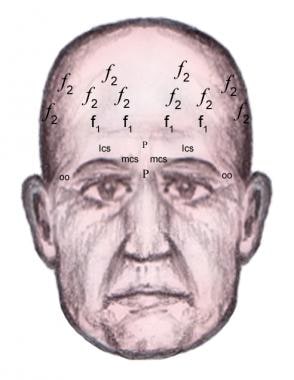
Distal trigeminal blocks can be performed to target specific distal branches of the 3 divisions of the trigeminal nerve, specifically the supraorbital branch of the ophthalmic nerve, infraorbital branch of the maxillary nerve, and mental branch of the mandibular nerve. These blocks are performed with a 25-gauge needle directed at the superficial foraminal site, where approximately 2-3 mL of LA can then be injected. See the image below.
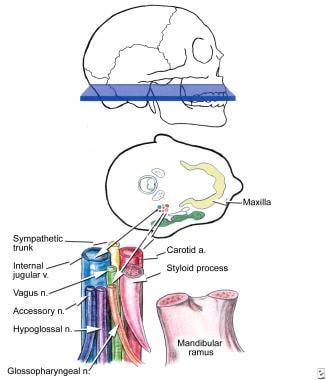
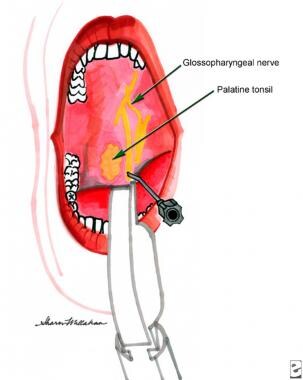
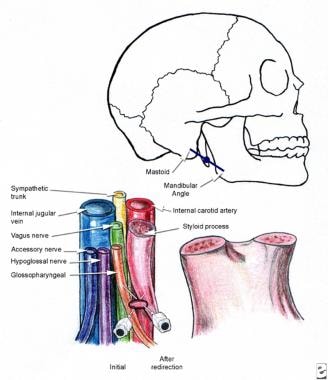
Glossopharyngeal nerve blocks
Glossopharyngeal nerve block is also performed for diagnosis and management of neuralgia. The glossopharyngeal nerve exits the jugular foramen at the base of the skull in close association with structures of the cheek, including the parotid gland and vagus nerve. It then descends into the neck between the internal and external carotid arteries. See the image below.
A glossopharyngeal block can be carried out intra-orally or using a peristyloid technique. If the block is performed intra-orally, the patient must be capable of opening the mouth, and adequate topical anesthesia of the tongue is necessary to allow needle placement at the base of the tonsillar pillar. While using this approach, care must be taken because of the proximity of the glossopharyngeal nerve to the internal carotid artery, which lies immediately lateral to the tip of the correctly positioned needle. See the image below.
The peristyloid approach, also described by Brown, begins with the patient in a supine position with the head neutral. See the image below.
A 22-gauge needle is inserted at the midpoint of a line between the mastoid process and angle of the mandible and advanced until it reaches the styloid process. Palpation of the styloid process should be maintained while the needle is inserted until it reaches this structure. The needle is then pulled back and redirected to slip off the posterior border of the styloid process. Careful aspiration for blood is necessary because of the intimate relationship of both the internal jugular vein and carotid artery to the glossopharyngeal nerve.
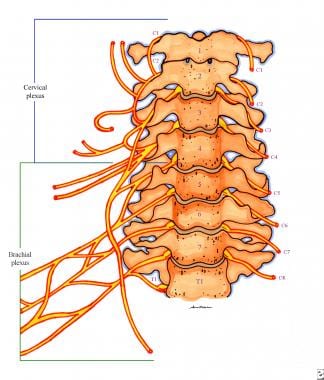
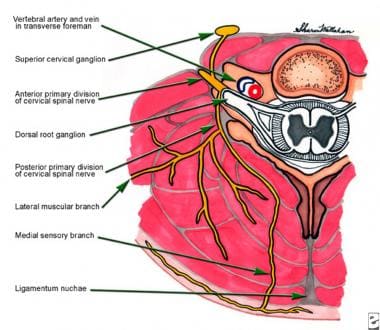
Other blocks, including cervical plexus, superior laryngeal, translaryngeal, and retrobulbar blocks, are usually best performed by anesthesiologists or surgical subspecialists. These blocks are usually performed to achieve regional anesthesia, although a retrobulbar block can be useful diagnostically for determining the etiology of eye pain.
Clinical Application of Spinal Injection Techniques
Pain sensitive spinal structures within the 3 joint complex (composed of the disk and 2 posteriorly situated facet joints) include the nerve roots, dura, posterior longitudinal ligaments, outer annular fibers of the disk, facet joints, joint capsules, and cancellous bone. Intraspinal structures without proven pain innervation include the ligament flavum, inner annulus and nucleus pulposus. Spinal interventional techniques can isolate potential pain generators, and also provide therapeutic relief from pain and associated neurologic symptoms. Identification of a pain–producing structure can be inferred when the patient's characteristic pattern is provoked by radiocontrast agents or saline. Furthermore, diagnostic value can be derived from the patient's response to an injected local anesthetic, and sometimes the use of corticosteroids or neurolysis can provide durable therapeutic value. Safety and accuracy are enhanced when the practitioner performing these procedures is knowledgeableofspinalanatomy,experienced with the use of fluoroscopy, and skilled at steering needles within the soft tissues of the back.
The decision to perform a spinal interventional procedure should be based on sound medical evidence. Evidence-based medicine is a strategic approach to managing cost by managing care. It is the judicious use of the current best evidence for making decisions about the care of individual patients. Therefore, when clinical and research evidence support the benefit of a specific procedure for a particular patient problem, it can be considered and even advocated. If medical evidence suggests that no clear benefit is derived from a procedure for a specific indication, or if the procedure may harm the patient, either directly through adverse events or indirectly by wasting medical resources, then it should be avoided.
A pivotal 2007 evidence-synthesis and review of the literature cites the authors evaluation of the relative strength of the evidence that supports the use of spinal interventional techniques for providing short and long-term relief from chronic spinal pain. Table I outlines their analysis of the benefit from the application of several procedures that are predominantly used for treatment in the lumbar region.
Table 1. Therapeutic Interventional Techniques [15] (Open Table in a new window)
Facet Joint Interventions |
Short-term |
Long-term |
Intra-articular injections |
Moderate |
|
Medial branch blocks |
Strong |
Moderate |
Radiofrequency |
Strong |
Moderate to strong |
Epidural Steroid Injections |
|
|
Interlaminar |
Strong |
Limited |
Caudal |
Strong |
Moderate |
Transforaminal |
Strong |
Moderate |
Adhesiolysis |
|
|
Percutaneous |
Strong |
Strong |
Endoscopic |
Strong |
Moderate |
Intradiscal Therapy |
|
|
IDET |
Strong |
Moderate |
Nucleoplasty |
Limited |
Limited |
When insufficient evidence exists to determine whether the procedure is beneficial, then the operating practitioner can depend on clinical experience and operate within standard of care or conservative guidelines. Manchikanti and colleagues have defined guidelines that classify the strength of experimental evidence that supports decisions as to whether specific interventional pain procedures should be performed. This analysis includes the prevalence of specific spinal pain generators and the efficacy of performing specific procedures for therapeutic or diagnostic purposes. [16]
Epidural corticosteroid injections reportedly were used first in 1952 by Robecchi and Capra, who claimed to provide relief of lumbar and sciatic pain in a woman after periradicular injection of hydrocortisone into the first sacral root. Sacral epidural injection of steroid by the transforaminal route was largely popularized in Italy and involved passing a needle through the first dorsal sacral foramen to gain access to the first sacral nerve roots.
Caudally administered solutions require a substantial volume so that the injectate reaches the lumbar nerve roots, which lie approximately 10 cm or more cephalad to the site of injection. Frequently, a threaded catheter inserted under fluoroscopic guidance provides more precise anatomical application, thereby avoiding the complications associated with injection of a large volume of fluid. Traditionally, clinicians and investigators have used methylprednisolone or triamcinolone, mixed with variable, often large, volumes of LA and isotonic saline or sterile water, for spinal injections.
Corticosteroids may be administered into the lumbar epidural space through either a caudal or lumbar approach, with the latter approach advocated as more target specific and requiring smaller volumes of injectate. For the same reason, many spine specialists advocate transforaminal steroids because this route of administration is placed more precisely at or near the presumed painful nerve root. Once the drug is injected into the epidural space, the operator has no control over dispersal, which is governed by injection volume and pressure and the anatomy of the epidural space.
Normal epidural ligaments or epidural scarring may obstruct passage of injectate to the desired site. To overcome these perceived difficulties, some operators advocate delivering the drugs into the epidural space immediately surrounding the nerve root. Therefore, the target nerve root is approached with the needle under radiographic guidance along an oblique paravertebral approach. Targeting the root, and not the epidural space, is more likely to deliver the corticosteroid solution to the affected nerve root.
The rationale for use of epidural steroids was based on the belief and some supporting literature, including animal studies, that lumbosacral radiculopathies may have an inflammatory component. [17] A study performed by Ryan and Taylor arbitrarily divided 70 patients into 2 groups -- those with "compressive radiculopathy" and those with "irritative radiculopathy." The former group was characterized by sciatica with sensory, motor, and reflex disturbances, while the latter was characterized by sciatica alone. Intrathecal and epidural injections of corticosteroids produced better therapeutic responses in the group with "irritative radiculopathy." Furthermore, responders tended to have higher CSF protein levels and a shorter duration of illness, particularly with sciatica lasting less than 2 weeks. [18]
Therefore, epidural corticosteroids may provide relief in some cases of radiculopathy owing to their anti-inflammatory properties; however, research has demonstrated that methylprednisolone has a direct inhibitory action upon nociceptive input. In summary, many practitioners advocate the use of epidural corticosteroids as treatment for inflammatory-type radicular pain and preclude their use for axial or referred somatic pain. Since nerve root inflammation has not been implicated as the only cause of back pain, no confirming data exist to support the use of epidural steroids for low back pain alone.
Epidural corticosteroids should be used with caution or avoided in some cases of congenital anomaly or prior surgery that has altered the normal anatomy of the epidural space, when corticosteroids may unmask an infection, in patients with coagulopathy, and in patients susceptible to fluid retention and congestive heart failure. Epidural corticosteroids are absorbed systemically, which may cause suppression of adrenal function for up to 2-3 weeks.
Other "red flags" that should warn practitioners considering use of corticosteroids include patients with significant contributing operant and psychosocial factors, clinical presentation suggestive of somatization, nonmechanical back pain, disability related to the lumbosacral syndrome under treatment, normal straight leg raising, and pain that is not decreased by medication of any type. Factors that seem to have no bearing on the decision to use corticosteroids include age, pattern and frequency of pain intensity, results of physical examination, and presence or absence of structural pathology.
Corticosteroids have been advocated using the same techniques and operational procedures as described previously in this article for somatic, transforaminal, and epidural neural blockade. The issues associated with the use of epidural corticosteroids include those attributed to injection technique and local anesthetics. Infection is possible following any injection but is an exceedingly rare complication of epidural corticosteroids and has been documented only in several case reports.
Arterial hypotension has been reported as a complication of epidural steroids unrelated to LA toxicity. Other adverse effects ascribed to corticosteroids have included nausea, vomiting, respiratory insufficiency, insomnia, and facial flushing.
The technical risks of epidural steroid injection include bloody tap, nerve root injury, and dural puncture. Dural puncture usually is associated with postural or low-pressure headaches, which are increased in intensity when the patient is vertical and improve in deliberate fashion when the patient moves to a horizontal position. Bed rest, fluid intake, and caffeinated beverages usually resolve such headaches; however, in some cases, placement of a blood patch is necessary over the presumed site of dural puncture.
Uncontrolled studies on the use of caudal epidural corticosteroids have shown benefit in 33-77% of patients. One study indicated no significant difference in outcome between a group of 24 patients treated with caudal injections of procaine 1% and methylprednisolone 80 mg and another group of 24 patients treated with procaine alone. Two additional studies purported to show that caudally administered LA mixed with corticosteroids yielded a clinical benefit, but comparison data were found to lack statistical significance. Another 3 studies reporting the same results were methodologically flawed. Overall, the published literature supports the therapeutic use of caudal epidural steroids for the treatment of radicular symptoms; however, the scientific evidence is weak.
On assessment, the published medical literature also is favorably disposed toward the use of lumbar epidural LA and corticosteroid combinations for radicular symptoms, although more negative studies have emerged evaluating the lumbar epidural approach than evaluating the caudal approach. Dilke et al studied 100 patients with unilateral sciatica who received either active treatment consisting of lumbar epidural injection of 40 mL of 0.75% lignocaine with 80 mg of methylprednisolone and 25 mg of hydrocortisone, or a control injection of 1 mg of isotonic saline solution into the interspinous ligament. Significantly, more patients receiving the active treatment had their pain "clearly relieved." Three months after treatment, a greater proportion of the active treatment group had no pain, took no analgesics, and had resumed work. However, some of the treatment group had undergone subsequent surgery or other nonsurgical treatments; these latter differences were not statistically significant.
Other randomized controlled studies have shown conflicting results and been attacked as methodologically flawed. Clinical judgment remains the mainstay of support for or against the use of lumbar epidural steroid injections. Some advocate their use in the early management of selected patients with sciatica or radiculopathy; however, benefits are usually temporary.
Diagnostic spinal synovial joint blocks are used to assess whether the pain stems entirely from the zygapophyseal joints. No established clinical or radiographic features are recognized uniformly that enable practitioners to assign the posterior articulations as probable pain generators. Furthermore, degenerative features on CT scan have shown poor specificity and sensitivity in implicating these as causative of pain, and joints that appear normal have been demonstrated to be symptomatic. Aprill et al have mapped typical referral patterns that occur with provocative injections into the synovial zygapophyseal joints.
Cervicogenic headache involving the occiput and posterior portion of the head has been demonstrated as a result of injections into the C2-3 facet and lateral atlantoaxial joint. Provocation at C3-4 tends to span the entire cervical area but not to extend into either occiput or shoulder girdle. Provocation at C4-5 sends pain into the angle formed by the neck and top of the shoulder girdle. Provocation at C5-6 tends to produce pain over the supraspinous fossa to the acromion, and provocation at C6-7 provokes pain that radiates into the ipsilateral scapula. Reproducible pain patterns have been harder to establish in similar injection studies of lumbar spine facets, although provocation of these joints at L4-5 or L5-S1 usually results in pain referred into the low back, gluteal, and posterior thigh regions.
Nevertheless, the facet joints of the lumbar spine have been implicated as a source of low back pain since 1911. Injections of intra-articular anesthetic have provoked and alleviated pain. Although some spine specialists and interventionists advocate facet injections as a treatment method, several studies, including a large prospective study and 3 randomized controlled trials, showed no significant long-term benefit. Intra-articular facet injections, which are costly and invasive, should be considered as an adjunctive method for diagnostic identity of pain generator(s), and if convincing pain relief is obtained from intra-articular anesthetic block, the practitioner should remain open-minded in addressing the zygapophyseal joints as a potential pain source. Estimates for the prevalence of lumbar facet syndromes range widely in the published medical literature from as low as 7% to as high as 75%.
The prevalence of cervical zygapophyseal joint pain has been studied and estimated at 65%. Intra-articular corticosteroids have been used for presumptive zygapophyseal joint pain involving the lumbar and cervical spine. A carefully designed, double-blind study of intra-articular steroids versus saline for lumbar zygapophyseal joint pain revealed no clinically significant differences between groups at 1- or 6-month follow-up. No controlled studies of the value of intra-articular steroids for neck pain have been published. The concept of denervating painful zygapophyseal joints has been explored.
Some investigators have identified modest benefit from medial branch neurolysis with phenol. Percutaneous radiofrequency neurotomy has been advocated for neurolysis of the medial branch or for facet articular denervation as a treatment for both neck and back pain. A recent double-blind, randomized, controlled study comparing percutaneous radiofrequency neurotomy for chronic cervical zygapophyseal joint pain showed approximately 50% improvement in pain for a mean duration greater than 8 months when compared with an identical sham procedure.
A prospective, randomized, double-blind study of injections into diskography-confirmed painful disks showed no significant difference in benefit between corticosteroids and LAs. Other interventions used to disrupt painful epidural adhesions have included hyaluronidase, hypertonic saline, and corticosteroids. Intrathecal morphine and dorsal column stimulation have been proposed as options in specific cases of severe, disabling, and intractable low back pain.
Technical Principles of Spinal Neural Blockade
Cervical spinal nerve blocks
Cervical spinal nerve blocks can alleviate pain caused by segmental neuralgia or by primary spinal lesions (eg, nerve root compression caused by disk protrusion, spondylosis, or neoplasm). In some cases, these blocks provide prognostic information, and. if successful. can be followed by neurolytic or neuroablative interruption of involved pathways, particularly when the pain is caused by cancer. Also, selective nerve root blocks are often used to determine whether a patient will respond to surgical decompression of the targeted spinal nerve.
Cervical nerve roots (C1-C8) pass laterally through their respective foramina within the sulcus of each transverse process and exit at the level above the vertebral segment for which they are numbered. See the image below.
The posterior tubercle of the tip of each transverse process is larger and more superficial, and therefore is easier to palpate than the nearby anterior tubercle. Ventral and dorsal divisions of each cervical nerve root join to form the dorsal root ganglion, which lies just posterior to the ascending vertebral artery.
Just lateral to the dorsal root ganglion, the posterior primary division or dorsal ramus passes posteriorly, dividing into a lateral muscular branch and a medial sensory branch. See the image below.
The anterior primary division or ventral ramus continues its anterolateral course, sending gray ramus communicantes to the nearby sympathetic ganglion situated adjacent to the anterolateral surface of the vertebral body. See the image below.
Cervical selective nerve root blocks
Nerves emanating from the spinal cord can be blocked in the paravertebral region or at certain points along their course. These procedures usually are performed for management of severe acute or chronic pain affecting the trunk or extremities, to relieve painful muscle spasm, or to block sympathetic nervous system dysfunction in affected limbs. Each cervical nerve root can be blocked paravertebrally by approaching the nerve in a lateral or posterior direction as it lies within the shallow sulcus of the transverse process. The posterior approach is technically more difficult but may be necessary in patients with contraindications due to skin infection, carcinoma, or other pathological processes in the lateral structures of the neck. Furthermore, neural blockade of the C8 nerve root can be achieved only from a posterior approach by slowly passing the needle caudally and slightly medially over the transverse process of C7, until the patient reports paresthesia in the C8 distribution. See the image below.
With the patient in the supine or lateral position on the fluoroscopy table, the fluoroscopy beam is rotated from a lateral to oblique position to allow visualization of the affected neural foramina at its largest diameter. Next, the fluoroscopy beam is moved from a cephalad to caudal position, which allows visualization of the affected neural foramen. This maneuver should place the beam parallel to the targeted nerve root in the approximate center of the inferior portion of the foramen.
Next, the skin is prepped with an antiseptic solution, and a skin wheal of local anesthetic is placed at a point overlying the posterior aspect of the foramen over the tip of the superior articular process of the level below the affected neural foramen. A 25-gauge, 2-inch needle is passed through the skin wheal and advanced until it abuts the superior articular process of the level below the targeted foramen. This contact on bone provides the operator with knowledge specifically regarding the depth of the needle tip in relationship to the neural foramen, and feedback that the needle tip is resting safely on bone.
After the needle tip is safely oriented on bone, the needle is withdrawn slightly and then redirected caudally and ventrally toward the target nerve root. The patient should be instructed to notify the operator as soon as he feels a paresthesia, which is elicited when the needle touches the nerve root. The needle should be targeted just dorsal of the uncinate process toward the center of the foramen; a fluoroscopic image confirms placement of the needle tip at or near the margin of the lateral mass adjacent to the targeted nerve, outside of the neural foramen and outside the epidural, subdural, and subarachnoid spaces.
Approximately 0.3 cc of a suitable contrast medium is carefully injected around the target nerve root. The contrast should outline the affected nerve root and produce a neurogram. Injection of 2-4% lidocaine should flow in the same distribution as the previously injected contrast. [19]
Both the contrast and local anesthetic irritate the target nerve root so that the patient experiences a painful response. If the purposed nerve root is the primary pain generator, then the patient experiences pain that is concordant. Concordance implies that provocation reproduces the essential nature of the neck and arm pain symptoms that are under investigation.
Also, as the LA takes effect, this familiar sensory experience, including pain characteristics (eg, intensity, regional pattern, associated symptoms) should diminish. This procedural approach is commonly referred to as provocate and ablate responses, and this approach is widely practiced by clinicians that may vary or determine their opinion based on the procedure's influence as a part of the data used to pursue and locate a spinal pain generator.
Selective nerve root blocks (SNRBs) are often useful diagnostically and prognostically as part of a surgical work-up. Some experts advocate that deposition of a small amount of corticosteroids might produce a therapeutic effect. The therapeutic application of LAs and corticosteroids may provide short-term relief for presurgical reconditioning or as part of a nonoperative treatment plan, to reduce pain while initiating a physical therapy or functional restoration program.
Because selective nerve root blocks are often performed for diagnostic purposes, only small quantities of LA should be used to prevent any confusion that may occur if anesthesia spreads to adjacent nerve roots simultaneously. Nerve roots are identified by eliciting dermatomal paresthesia; radiographic confirmation is useful to ascertain the level and to prevent needle injury to the target nerve root.
Complications of paravertebral block include accidental injection into the subarachnoid, subdural, or epidural space. This is particularly hazardous in the cervical region, where anesthetic may diffuse and cause phrenic nerve and respiratory paralysis. Accidental injection of LA into the vertebral artery may lead to transient loss of function in vital brainstem areas and cause impaired consciousness, coma, and seizures.
This complication requires immediate cardiorespiratory and circulatory support until the LA is redistributed and metabolized. Other possible adverse events include anesthesia or injury to the cervical sympathetic chain (with development of Horner syndrome), the superior or recurrent laryngeal nerve, or the trunk of the vagus nerve. Because of the risks of unintended recurrent laryngeal and phrenic nerve block, limiting the procedure to a unilateral injection at any one treatment setting is advisable.
Inadvertent needle trauma and/or injection into the spinal cord can cause quadriplegia and death. Intravascular placement or injection may cause systemic LA toxicity or inadvertently spread local infectious agents, even creating sepsis. An unintentional breach of the dura may lead to total spinal anesthesia with associated loss of consciousness, hypotension, and apnea. Needle trauma to epidural veins may cause bleeding that results in an epidural hematoma with spinal cord compression and associated neurological deficit. Epidural introduction of infection may lead to an abscess or to widespread infection in immunocompromised patients (eg, AIDS, cancer).
Needle placement for selective cervical nerve root blocks is characteristically targeted just outside the neural foramen so that deposition of the injectate does not enter the epidural, subdural, or subarachnoid space. Furthermore, some experts advocate the deposition of a small amount of corticosteroids provides a therapeutic influence. However, adverse events due to transforaminal placement of LA and corticosteroids can be tragic, with trauma or occlusion of the foraminal radicular artery. Recently, this has been implicated as causative when particulate steroids are used. [19, 20, 21]
Cervical epidural spinal blocks
Some experts advocate cervical epidural blocks (CEBs) with LA, combined with corticosteroids or opioids for acute or palliative pain relief when diagnostic evaluation has not yet identified the cause or nature of the presenting disease or while the patient is awaiting more pertinent therapy, including surgery. Temporary pain management may be indicated for postoperative, posttraumatic, infectious (ie, herpes zoster), or cancer-related pain in patients awaiting treatment that is more definitive, that requires time to exert efficacy, or that reduces suffering when death is the expected outcome.
CEBs have been shown to offer therapeutic value for the treatment of upper extremity vascular insufficiency due to vaso-occlusive or vasospastic disorders and have been shown to improve vascular perfusion in disorders like frostbite and ergotamine toxicity. Some advocate CEBs for pain relief for patients when adjunctive or parallel treatment is underway or if multiple pharmaceutical trials are needed or if prolonged treatment duration through rehabilitation, time for healing, or disease resolution is needed.
Some experts advocate CEBs for cervical spinal degenerative disorders with radiculopathy, spinal stenosis, discogenic pain or spondylosis, failed surgery disorders, refractory cervicogenic headaches, spinal fractures, upper limb amputations, complex regional pain syndromes, acquired neuropathic pain from postherpetic neuralgia, or polyneuropathy from diabetes or chemotherapy. [21]
The transforaminal approach with LAs and corticosteroids, when performed correctly is considered by many physicians to be the most specific for determining the diagnosis and prognosis for the treatment of chronic cervical radicular syndromes due to discal compression, vascular insufficiency, inflammation, noxious biochemical factors, failed surgical disorders, and spondylosis with stenosis; this is especially the case when it is preceded by a selective nerve root block.
Some specialists advocate this approach as being more effective; however, most evidence is moderate for short-term and long-term benefit. Although once considered the treatment of choice for selective cervical radicular pain, a high incidence of major complications suggests more caution when considering CEBs. High cervical and brainstem infarction are presumed to be caused by vertebral artery trauma, vasospasm, and in some cases, to thromboembolic occlusion. Trauma and occlusion of the cervical foraminal radicular artery has been frequently reported as a cause of severe complications of late. The latter complication has been noticed and speculated by some to occur more often with the use of particulate corticosteroids. Other complications of this procedure include high cervical spinal anesthesia, seizures, and death. [19, 20, 21]
Fluoroscopy is recommended to aid in needle placement. With the patient in a supine position on the fluoroscopy table, the patient's head is turned slightly away from the side of the injection so that the fluoroscopy beam is rotated to an anterior oblique position to allow the best visualization of the target neural foramina at its largest diameter. The fluoroscopy beam may need to be moved caudally to allow better visualization of the targeted neural foramina, which occurs when the fluoroscopic beam is parallel with the affected nerve root.
The skin is prepared with antiseptic solution and with a LA to produce a skin wheal. The skin wheal is placed at a point overlying the posterior aspect of the foramen just over the tip of the superior articular process at the level below the affected neural foramen. This point is approximately one third of the distance from the most posterior-inferior aspect of the foramen.
A 25-gauge, 2-inch needle is placed through the previously anesthetized area and advanced until the tip rests against the superior articular process just posterior to the targeted neural foramen. The physician should be concerned with failure to impinge on bone because such a failure may indicate that the needle has passed through the foramen and into the substance of the spinal cord. Of course, correct bony placement should be achieved and identified using AP and lateral fluoroscopic views to verify the needle's position within the neural foramen and not past the midpoint of the posterior column composed of the facet joints.
When satisfactory needle position is confirmed, the needle bevel is medially oriented, and 0.2-0.4 mL of contrast medium is gently injected under active fluoroscopy. Contrast flow into the epidural space and distally along the affected nerve root sheath. The injected contrast should be immediately stopped if the patient complains of pain from the injection. If placement and epidural contrast flow suggests that the needle is properly placed, then injection of 6 mg of betamethasone or a solution of 20-40 mg of methylprednisolone or 20-40 mg of triamcinolone are combined with 0.5-1.5 mL of 2-4% of preservative-free lidocaine is slowly injected; this is terminated if the patient describes pain. [19]
Recently, blunt and flexible catheters with microbore extension tubing, and even radiopaque markers, have been developed to reduce the risk of complications associated with intraforaminal injections; these include TRUCATH™. The blunt flexible catheter is better designed to deflect and reduce penetration of vascular and neural elements. Side injection orifices for injection of contrast and a radiopaque marker on the catheter tip enhance the interventionalist's ability to anatomically determine the location of the needle tip. Although studies have not proven these attributes actually reduce complications, they are welcomed tools because they possess progressive design for technical methodology that will prevent some percentage of devastating vascular and neural complications.
The translaminar or interlaminar approach is considered the safest and most effective technique for cervical epidural placement of local anesthetic, corticosteroids, and sometimes opioids, for various diagnostic, therapeutic, or prognostic purposes. CEBs with LA and/or opioids may be used to dampen acute pain, especially during emergencies while waiting for more definitive or effective treatment through pharmacologic, surgical, and/or antiblastic methods. CEBs may be used to manage pain after trauma or surgery, as well as various other disorders that are hard to manage, even with parenteral opioids, such as acutely painful conditions as herpes zoster, cancer, limb amputation, and acute vascular insufficiency. [19, 20, 21]
Performance of a interlaminar CEB can be performed with the patient sitting or horizontally in a lateral or prone position. Regardless of the operator's experience, this procedure is best performed with fluoroscopic guidance. In most cases, the patient is placed in an optimal flexed cervical spine posture stabilized with enough resistance to prevent movement of the head during the procedure.
The skin is prepared with an antiseptic solution and the operator places the middle and index fingers on each side of the spinous processes at C5-6 or C6-7 spinal levels. The midline of the selected interspace is identified by palpating the spinous processes above and below where midline needle entry is intended. LA, such as lidocaine, may be used, to mark the intended site of skin entry. See image below
As much as 1 mL of a short acting anesthetic (eg, lidocaine) is used to infiltrate the skin and subcutaneous tissues, as well as both the supraspinous, and interspinous ligaments. Physicians are advised to insert a 25-gauge, 2-inch needle exactly into the targeted midline. Some physicians prefer to use a longer, larger, blunter needle, such as a 3.5-inch, 18-gauge or 20-gauge Hustead needle.
After the LA has been given time to anesthetize the area, a right-hand dominant physician holds the needle firmly at the hub with the left thumb and index finger. Then the palm of the left hand is placed firmly against the patient’s neck, so that the left hand acts as a unit to stabilize, protect, and control the needle’s trajectory and its metered ingress from any unexpected patient or physician activity.
The needle is then advanced with the left hand, which is braced against the neck with the needle hub held tightly between the left thumb and forefinger The operator uses the right hand to monitor resistance through a syringe containing air or preservative free normal saline. With constant pressure applied to the plunger of the syringe through light pressure applied by the right thumb, the needle and syringe are advanced in a slow and deliberate manner. As the bevel passes through the ligament flavum and enters the epidural space, a sudden loss of resistance that the operator appreciates; the plunger can then be effortlessly depressed under minimal, if any, pressure through the right thumb.
Needle position within the epidural space can be checked by using fluoroscopic verification and by repeating the loss of resistance maneuver. The cervical epidural space should accept 0.5-1 mL of air or sterile preservative free saline without significant resistance. The force required to depress the plunger should not exceed that which is necessary to overcome the resistance of the needle. Any significant pain or sudden increase in resistance during the injection suggests incorrect needle placement.
The physician should stop the injection and assess the position of the needle using fluoroscopy. If the needle remains satisfactorily placed and loss of resistance within the epidural space is confirmed without additional patient report of pain, gentle aspiration is checked to assure that the needle is not positioned in the subarachnoid space or that it’s not intravascular. If cerebrospinal fluid (CSF) is aspirated, the operator can repeat the block attempt at a different interspace. If aspiration of blood occurs, the needle should be tightly rotated and the aspiration test should be repeated. If the aspiration of blood continues, the procedure should be aborted due to the danger of developing an epidural hematoma and possibly neurological compromise. [19]
If the operator is confident that the needle is correctly placed in the midline of the epidural space, then injection of as much as 5-7 mL of solution can be performed. For diagnostic and prognostic blocks, 1% preservative-free lidocaine is a reasonable choice. For therapeutic blocks, 0.25% preservative-free bupivacaine combined with 40-80 mg of methylprednisolone is commonly recommended.
In some cases, this procedure is repeated on a daily basis or every other day when treating acute painful disorders. Repeat treatments are performed in cases whereby temporary pain reduction is indicated for the management of acute pain Some randomized studies have demonstrated both short-term (< 6 wk) and long-term (≥6 wk) pain relief from CEBs. [22, 23]
When the cervical epidural route is chosen for the administration of opioids, 0.5 mg of preservative-free morphine sulfate is a reasonable initial dose in patients who can tolerate opioids. More lipid-soluble opioids such as fentanyl must be delivered by continuous infusion via cervical epidural catheter.
Cervical epidural injections by interlaminar approach are usually considered safe and effective; however, the patient should undergo this procedure without anesthesia, so that appropriate feedback can be provided to the physician operator.
Complications can include infections; hematogenous spread is facilitated by the Batson plexus. CEBs should not be performed with any suspicion of local or widespread infection. Anticoagulation and coagulopathy are absolute contraindications, and any medication that inhibits platelet adherence or normal coagulation is a contraindication unless these medications are withheld for a reasonable amount of time that is considered safe. The time that is necessary for safety is a property that is individual and specific to the drug in question and its mechanism of action. [19, 20, 21]
Dural puncture is uncommon but, if unrecognized, may cause immediate total spinal anesthesia associated with loss of consciousness, hypotension, and apnea. Epidural doses of opioids accidentally placed into the subarachnoid space can cause profound respiratory and CNS depression. Physician recognition of these complications must be immediate to be effective. Subdural placement of epidural doses of local anesthetics can produce a clinical scenario similar to a massive subarachnoid injection. [19, 20, 21]
Needle trauma to epidural veins may also result in self-limited bleeding; in the best-case scenario, this only leads to postprocedure pain. However, uncontrolled bleeding into the epidural space can result in a hematoma with compression of the spinal cord, resulting in neurologic deficit, including cervical myelopathy. Needle trauma to the spinal cord or nerve roots is usually accompanied by pain.
Principal tenets are common sense. If the clinician encounters significant pain or opposition by the patient, the procedure should be stopped. The procedure should be stopped or completely aborted when a complication is suspected, even when it is not clearly apparent. Avoiding patients who are immunocompromised or otherwise at risk for complications should always be considered to avoid potential adverse events. [19, 20, 21]
Cervical facet blocks
Intra-articular cervical zygapophyseal joint blocks should be performed by a highly skilled interventionist experienced with the use of fluoroscopy for needle placement. They are usually performed as a diagnostic maneuver to prove that a specific facet-joint is in fact the source of pain. Intra-articular cervical facet blocks are primarily used for diagnostic maneuvers (eg, to prove that a specific facet joint is the source of pain). [19]
Facet pathology is commonly presumed to be salient when pursuing localization of a primarily axial neck pain source. Blind injection techniques are no longer considered the standard of care because of the accessibility of fluoroscopy. The C3-4 to C6-7 levels can be approached using either a posterior or lateral approach. Only the lateral approach is in feasible for the C7-T1 joint because of the obligatory steep slope approach. An oblique approach to the C2-3 zygapophyseal level is necessary because the joint tends to slope caudally and medially. [20]
Injection techniques described by Bogduk et al are usually accomplished with the patient in a prone position; however, if necessary, the patient can be in the sitting position. A 22-gauge or 25-gauge needle is directed into the midpoint of the target joint from a posterior paraspinal site, usually 2 or more segments caudally and along an oblique trajectory that coincides with the plane of the joint as viewed by C-arm fluoroscopy. The needle is directed through the skin upward and ventrally through the posterior neck muscles until it touches the posterior aspect of the targeted facet; the needle then can be readjusted until it enters the joint cavity.
Repeated PA and lateral screening by fluoroscopy provides the operator with assurance that the needle maintains its intended course. The bevel of the needle should enter the target joint at its midpoint. [19, 20]
Once the needle is located in the joint, injection of contrast medium should produce an arthrogram and confirm accurate needle placement. Contrast injection may induce a pain response from the awake patient. The practitioner should carefully record whether the contrast-induced pain is concordant (identical to the pain under investigation), partly concordant (similar, but not identical), or non-concordant (a different, new pain experience).
After the patient's pain assessment is recorded, the injection of LA with or without corticosteroids provides further diagnostic and treatment information, including whether or not the pain can be satisfactorily ablated with intra-articular treatment or treatment may provide better relief if aimed at the joint’s innervation by blocking the pertinent medial branches of the dorsal root rami. The medial branch block technique can also be used to determine the symptomatic level, although this may be confounded due to the facet joint’s characteristic innervation, which is received from 2 spinal levels. Each joint receives nociceptive afferents from the dorsal root ramus at the same level and from dorsal root ramus of the vertebral level above. [19, 20, 21]
Although the goals of this procedure are controversial, therapeutic response is the primary goal for the proceduralist. The capacity of the joint can be gauged from the injection of the contrast medium; it is usually less than 1 mL. The capacity of zygapophyseal joints should be considered to prevent rupture of the joint capsule and unwanted spread of the injected agent into surrounding tissues, which may exacerbate the patient's pain syndrome and confound the identification of the joint as a pain generator. Other possible complications include inadvertent trauma and puncture of the deep cervical artery en route, the facet-joint capsule, the vertebral artery or vein, the ventral ramus of the spinal nerve, the epidural space, or in some cases the spinal cord.
The lateral approach to the cervical zygapophyseal joints described by Bogduk et al is performed with the patient in the lateral position. In these cases, the patient may be gently rolled ventrally or dorsally, or the x-ray beam adjusted to tilt along the transverse plane of the target joint. The needle is directed, then advanced, toward the superior or inferior articular process at the midpoint of the target joint. This is done carefully so that the needle does not pass deeper into or through the joint into the epidural space.
When the needle reaches the joint, the operator gently probes and pierces the capsule to enter the joint space, which can be sensed by the operator as a loss of resistance. Only minimal penetration is required. A small amount of contrast medium (0.3 mL) is used to obtain an arthrogram and to record the patient's pain response. The C2-3 zygapophyseal joints are blocked using the lateral approach already described. This level is considered important, and especially pertinent to neurologists, because several studies suggest that this articulation level is the most common source of cervicogenic headache.
Cervical medial branch blocks
Cervical medial branch blocks also can produce anesthesia of cervical facets. These medial branches of the cervical dorsal rami travel across the waist of the articular pillars (a point proximal to the origin of the articular branches). Here, the nerves have a constant relationship to bone and are more easily accessible by either a posterior or lateral approach. See the image below.
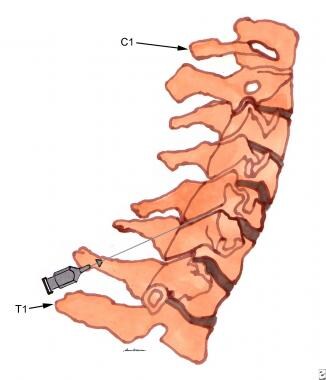 Cervical spine local injection technique into the cavity of the right C5-C6 zygapophyseal joint (lateral view). See text for details.
Cervical spine local injection technique into the cavity of the right C5-C6 zygapophyseal joint (lateral view). See text for details.
Atlantoaxial joint blocks
Atlantoaxial joint blocks should be performed only by highly skilled interventionists. The intra-articular target of this joint is at the midpoint of its radiographic silhouette as seen in posteroanterior views. This procedure is potentially hazardous with little margin for error because of the proximity of the dural sac, spinal cord, and vertebral artery.
Thoracic spinal nerve blocks
Thoracic paravertebral somatic or selective blocks (SNRBs) can alleviate pain involving the thoracic paraspinal regions, chest, and abdomen. SNRBs are helpful in determining the cause of nociception when patients complain of thoracic segmental neuralgia caused by nerve root impingement or inflammation due to vertebral column or foraminal pathology. Thoracic paravertebral blocks can also be used to quell the pain due to acute and chronic herpes zoster and other neuropathic pain syndromes, postthoracotomy, skeletal muscle spasm, and fractures or other structural complications associated with osteoporosis, surgery, and traumatic injuries to the chest wall or upper abdomen.
The thoracic paravertebral nerves exit their respective intervertebral foramina just beneath the transverse process of the vertebra. After exiting the intervertebral foramen, the thoracic paravertebral nerve provides a recurrent branch that loops back through the foramen to provide innervation to the spinal ligaments, meninges, and its respective vertebra. The thoracic paravertebral nerve interfaces with the thoracic sympathetic chain and then divides into an anterior and posterior primary division. The posterior innervates the facets, paraspinal muscles, and the skin of the back. The anterior division moves laterally into the subcostal groove and then under its respective rib to become an intercostal nerve.
Thoracic paravertebral somatic nerve blocks can be performed with the patient prone using C-arm fluoroscopic guidance. This technique is also described by Waldman. [19] The spinous of process of the vertebra just above the nerve to be blocked is palpated. Bonica and Waldman advocate the insertion of a 3.5-inch or 8-cm, 22-gauge, short-beveled needle through a skin wheal located approximately 4-5 cm (or 1.5 in) lateral and perpendicular to a location that originates just below the spinous process.
A skin wheal is raised using lidocaine, and then the area is prepped with an antiseptic agent. The needle is then directed anteriorly and medially at an angle of 45° to the midsagittal plane. Waldman suggests attaching a 12-cc syringe. The needle is then carefully advanced until it strikes the appropriate transverse process.
The needle should impinge on bone after being advanced approximately 1.5 inches. After bony contact is made, the needle is withdrawn into the subcutaneous tissues, redirected inferiorly, and walked off the inferior margin of the transverse process. As soon as bony contact is lost, the needle is slowly advanced approximately three quarters of an inch deeper until a paresthesia in the distribution of the thoracic paravertebral nerve to be blocked is elicited.
Furthermore, if paresthesia cannot be elicited, then electrical nerve stimulation and lateral fluoroscopy can be used for confirmation of safe and appropriate anatomic placement. If careful aspiration reveals no blood or CSF, then 5 mL of 1%, preservative-free lidocaine can be safely injected. If an inflammatory component to the pain is noted, the local anesthetic is combined with 80 mg of methylprednisolone and is injected in incremental doses.
Subsequent daily nerve blocks can be carried out in a similar manner, substituting 40 mg of methylprednisolone for the initial 80-mg dose. Because of overlapping innervation of the posterior elements from the medial branch of the posterior division from adjacent vertebrae, the paravertebral nerves above and below the nerve suspected of subserving the painful condition must be blocked. [19, 20]
Thoracic epidural nerve blocks
Using the transforaminal approach, epidural spinal block with local anesthetics can also be used to acquire diagnostic information when performing differential neural blockade to determine the anatomic basis of thoracic, chest wall, and abdominal pain. If procedural disruption of the thoracic nerve roots is considered, this technique is useful as a prognostic indicator of the degree of motor and sensory impairment that the patient may experience. Although the interlaminar approach is more commonly used for routine therapeutic thoracic epidural injections, some interventional pain treatment specialists believe that the transforaminal approach is more effective for the treatment of painful conditions involving a single radicular pain syndromes; however, the risk of complications is significantly higher, especially for thoracic radiculopathy caused by neural foraminal stenosis and/or perineural fibrosis. [19, 20, 21]
Transforaminal thoracic corticosteroid epidural injections are performed using the prone paravertebral. Although some experienced pain practitioners perform this technique described above using fluoroscopic guidance to aid in accurate needle placement and to reduce the risk of injury due to needle placement. It is also requisite for documenting the validity of therapeutic or diagnostic injections. With the patient in the prone position on the fluoroscopy table, the end plates of the affected vertebra are aligned or squared up on fluoroscopy. The fluoroscopy beam is rotated to a more ipsilateral oblique position to bring the images of the spinous process and head of the ribs medially.
A "magic box" consisting of the superior end plate, the inferior end plate, the lamina or lateral pedicle lines, and the rib head are visualized. This "magic box" represents the target for needle placement. A skin wheal of local anesthetic, antiseptically prepared, is placed at a point overlying the above mentioned box that corresponds to the inferior aspect of the foramen. A 25-gauge or 22-gauge, 3.5-inch spinal needle is placed through the previously anesthetized area and advanced until the tip is near the level of the posterior elements.
Care is taken to ensure that the needle tip does not stray laterally (pleura) or medially (spinal cord). Lateral fluoroscopy is used to view and advance the needle tip into the foramen. AP fluoroscopy is used for guidance of the needle tip to pass just medial to the lateral laminar border. Insertion of the needle past the foramen produces entry into the intervertebral disc.
After satisfactory needle position is confirmed, 0.2-0.4 mL of contrast medium suitable for subarachnoid use is gently injected under active fluoroscopy. The contrast may be seen to flow into the epidural space, with some flow distal along the nerve root sheath. On the lateral view, the foramen can be seen to be filled with contrast and a cross section of the nerve root is identified. The injection of contrast should be immediately stopped if the patient complains of significant pain upon injection.
After a satisfactory pattern is observed, and no evidence of subdural, subarachnoid, or intravascular spread of contrast is observed, 3-6 mg of betamethasone solution or 20-40 mg of methylprednisolone or triamcinolone 20-40mg suspension with 0.5-1.5 mL of 2-4%, preservative-free lidocaine is slowly injected. Injection of the local anesthetic and/or steroid should be discontinued if the patient complains of any significant pain on injection, although transient pressure paresthesia is often appreciated.
After satisfactory injection of the local anesthetic and/or steroid, the needle is removed and pressure is placed on the injection site. This technique may be repeated at additional levels as a diagnostic and/or therapeutic maneuver.
Procedural risks relate to the proximity of the needle tip to the posterior border of the lung; If the needle penetrates the intervertebral foramen, puncture of the dura and spinal cord are possible. To circumvent the risks of this procedure, Bonica developed a paralaminar technique with the patient positioned horizontally and laterally. A 5-cm to 8-cm, 22-gauge, short-bevel needle is inserted through a skin wheal of short-acting LA and advanced to the lateral edge of the lamina.
After contact with the lateral edge of the lamina, the needle is withdrawn until its point is subcutaneous and the skin is moved laterally, approximately 0.5 cm. The needle is then readvanced until it reaches a point just lateral to the upper edge of the lamina engaging the uppermost part of the superior costotransverse ligament just below the adjacent transverse process. A 2-mL glass syringe filled with saline solution is then attached to the needle. As long as the tip of the needle is within the ligament, the operator can perceive some resistance to injection. [19, 20, 21]
The paramedian approach to the epidural space is primarily used for blockade of the middle thoracic vertebral interspaces in which the acute downward angulation of the spinous processes make the midline approach to the thoracic epidural space unsatisfactory. Mid-thoracic epidural block has a limited number of applications for thoracic surgical anesthesia. Mid-thoracic epidural nerve block with local anesthetic can be used as a diagnostic tool when performing differential neural blockade on an anatomic basis in the evaluation of chest wall and thoracic pain. If destruction of the mid-thoracic nerve roots is being considered, this technique is useful as a prognostic indicator of the degree of motor and sensory impairment that the patient may experience.
Thoracic epidural spinal blocks with local anesthetics and/or opioids may be used to palliate acute pain emergencies while waiting for pharmacologic, surgical, and/or antiblastic methods to become effective. This technique is useful in the management of postoperative pain as well as pain secondary to trauma. The pain of acute herpes zoster, acute pancreatitis, and cancer-related pain are also amenable to treatment with epidurally administered local anesthetics, steroids, and/or opioids. The administration of local anesthetics and/or steroids via the thoracic approach to the epidural space is useful in the treatment of various chronic benign pain syndromes, including thoracic radiculopathy, thoracic postlaminectomy syndrome, vertebral compression fractures, chronic pancreatitis, diabetic polyneuropathy, chemotherapy-related peripheral neuropathy, postherpetic neuralgia, and reflex sympathetic dystrophy of the chest wall.
The mid-thoracic epidural administration of local anesthetics in combination with steroids and/or opioids is also useful in the palliation of cancer-related pain of the chest wall and intrathoracic organs. This technique has been especially successful in the relief of pain secondary to metastatic disease of the spine. The long-term epidural administration of opioids has become a mainstay in the palliation of many cancer-related pain disorders. [20]
Mid-thoracic paramedian epidural spinal blocks may be carried out in the sitting, lateral, or prone position, with the sitting position being favored for simplicity of patient positioning when compared with lateral position. [19] The prone position should be avoided because it makes patient monitoring more difficult. After the patient is placed in optimal sitting position with the thoracic spine flexed and forehead placed on a padded bedside table, the skin is prepared with an antiseptic solution. See image below.
By exerting constant pressure on the plunger of the syringe with the right hand, the needle is slowly advanced with the left hand until lack of resistance is discerned. When this occurs, the needle has passed through the costotransverse ligament into the paravertebral region and the needle tip is likely to be in near proximity to the targeted nerve root. If paresthesia is not elicited, a peripheral nerve stimulator can be used to ensure that the bevel of the needle is positioned adjacent to the nerve. For diagnostic purposes, 3 mL of 1% lidocaine or 0.25% bupivacaine can be injected.
For treatment of acute severe pain, 5 mL of 0.375-0.5% bupivacaine with epinephrine is commonly used. Production of a prolonged continuous block covering multiple levels involves a larger injectate of 10-15 mL of 0.375-0.5% bupivacaine with epinephrine through a fixed catheter. Possible complications include accidental subarachnoid or epidural injection, intravascular injection, and pneumothorax. [19, 20, 21]
Intercostal nerve blocks
Intercostal nerve block is a useful procedure for defining potential source of pain in the chest and abdominal wall. Intracostal neural blockade at the posterior axillary line relieves pain of somatic origin but does not relieve pain arising in the thoracic or abdominal viscera, which are supplied by nociceptive fibers that follow sympathetic pathways located near the vertebral column. Intercostal nerve blocks can also offer relief of severe posttraumatic, postoperative, or postinfectious pain in the thoracic or abdominal wall.
Other indications include severe pain involving rib fractures or dislocation of the costochondral joints at the sternum, chest pain associated with pleurisy, pain associated with herpes zoster or intracostal nerve entrapment in the abdominis rectus sheath, and postoperative pain from thoracotomy, sternotomy, and after renal surgery through flank incisions. Caution should be used when performing bilateral intracostal blocks because ventilation may be impaired. The intercostal nerves are the ventral rami of T1-T11; however, the twelfth ventral ramus becomes the subcostal nerve and travels between the transversus abdominis and internal oblique muscles of the abdomen. See the image below.
The intracostal nerve provides preganglionic sympathetic fibers to the sympathetic chain via the white rami communicantes and receives postganglionic neurons from the sympathetic chain through the gray rami communicantes. These gray rami join the spinal nerves near their exit from the intervertebral foramina.
A short distance beyond the intervertebral foramina, the nerve root divides into the posterior and anterior primary divisions. The posterior primary division carries sensory and motor fibers to posterior cutaneous and muscular tissues, which are paravertebral. The primary anterior division that becomes the intercostal nerve gives rise to the lateral cutaneous branch just anterior to the midaxillary line, which sends subcutaneous fibers anteriorly and posteriorly. The intercostal nerve continues to the anterior trunk where it terminates as the anterior cutaneous branch.
The posterior intercostal block, as described by Bonica, is carried out easily at the angle of the rib, where it is the most superficial and easiest to palpate. The patient is placed in the lateral position with the target side up if performing a unilateral block or in prone position if performing bilateral blocks. A 3-cm, 25-gauge, short-beveled needle is inserted through a skin wheal at the lower edge of the posterior angle of the rib. The second finger of the left hand is placed over the intercostal space and the skin is pushed gently cephalad so that the lower edge of the rib above can be palpated simultaneously. This technique protects the intercostal space, thus reducing the risk of passing the needle into the lung. See the images below.
The needle is advanced until the lower part of the lateral aspect of the rib is reached. After reaching the rib, the needle is grasped with the thumb and index finger of the left hand about 3-5 mm above the skin surface. The skin is moved caudally with the left index finger to allow the needle to slip just below the lower border of the rib and then the needle is advanced until the left thumb and finger grasping the needle become flush with the skin. Aspiration is attempted; if negative, 3-4 mL of LA solution is injected. This LA solution diffuses several centimeters distally and proximally to involve the sympathetic chain, which may also block visceral nociceptive pathways, thus helping to relieve pain, which arises from painful viscera as well. Injection of larger volumes will result in both paravertebral and epidural spread of the drug, which may cause arterial hypotension if many segments are involved.
The lateral intercostal block technique described by Bonica is performed 3-4 cm posterior to the midaxillary line where the lateral cutaneous nerve pierces the intracostal muscles and divides into anterior and posterior branches. The anterior branch supplies skin and subcutaneous tissues of the anterolateral chest and abdominal wall as far as 7 cm from the midline; the posterior branch supplies tissues as far as 7-10 cm from the spine. A block at this site is unlikely to diffuse to the paravertebral region and therefore is preferable to differentiate thoracic and abdominal visceral pain from somatic pain caused by disorders of the chest and abdominal wall. See the image below.
Intercostal block at this site produces less ventilatory impairment than blocks at other sites; therefore, it is often considered preferable for patients with pulmonary disorders. Because a block at this site does not relieve postoperative pain from the viscera, however, supplementary pharmacologic analgesia may be necessary.
Anterolateral intercostal block is performed in the anterior axillary line proximal to the takeoff of the anterior cutaneous branches of the thoracic intercostal nerves and is useful for alleviating the pain of sternotomy, fracture of the sternum, and dislocation of costicartilage articulations. See the image below.
This technique also can be used to block the cephalad 3 or 4 abdominal intercostal nerves just proximal to the costochondral articulation to provide analgesia in the upper abdominal wall. Like the lateral intracostal block, this procedure does not interrupt visceral nociceptive pathways.
Thoracic zygapophyseal joint blocks have received little attention in the literature. The orientation of these facet joints does not lend them to the posterolateral approaches used for intra-articular injections as in the cervical or lumbar spine. Furthermore, the exact course of the medial branches of the thoracic dorsal rami and the pattern of innervation of these joints has not been researched adequately.
Lumbar spinal nerve blocks
Lumbar selective nerve root blocks(SNRBs) can provide diagnostic information and also temporary pain relief associated with a known cause for painful nerve root compression (eg, due to structural vertebral bony and/or intervertebral disk pathology). SNRBs provide information regarding patients who have minimal or no definitive imaging findings; patients with multiple imaging abnormalities when a more accurate determination of surgical treatment levels need definition; preoperative or postoperative patients with unexplainable or complex recurrent pain; and patients with equivocal neurological examinations. These blocks can be used to reduce reflex spasm of the hip adductor muscles in patients with spasticity or paraplegia.
The technique described by Bonica begins with the patient in a prone position. The C-arm (image intensifier of patient) is rotated in a ipsilateral oblique angle with respect to the targeted nerve root, thereby bringing the "Scotty dog" appearance to view. Rotation of the C-arm or patient is continued until the ventral aspect of the superior articulating process (ear of the Scotty dog) has the same vertebral number as the nerve root to be blocked. The nerve root to be injected should be located between the anterior and posterior aspects of the vertebral body superior end plate. See image below.
The superior end plates should appear superimposed on fluoroscopy, thereby providing a bony limit to the depth of needle penetration. The nerve root normally passes a few millimeters inferior to the pedicle (eye of the Scotty dog) and 1-2 mm superficial to vertebral body. The lower thoracic and upper lumbar SNRBs should be blocked slightly more inferolaterally. The artery of Adamkiewicz is the main supply of arterial blood to the lowe rtwo thirds of the spinal canal and enters the canal anywhere from T7-L4.
The L5 nerve root is set up fluoroscopically in a similar fashion. However, standard positioning may cause the iliac crest to obstruct the proceduralist's approach. In this situation the needle is passed through an upside down triangular window formed by the inferior margin of the transverse process of L5, the superior articulating process of S1, and the iliac crest. The vertebral body limits the depth of needle penetration as it does in more cephalad SNRBs of the lumbar spine.
When performing a SNRB of the S1 sacral nerve root, the C-arm can be placed in a straight and the projection, unless an additional 5-10° of ipsilateral angulation allows better visualization of the S1 foramen, which cares as a circular lucency. There is no bony back trauma and to limit needle penetration, therefore, repeated visualization of the needle in AP and lateral planes using fluoroscopy must be performed more frequently.
Technically, when performing lumbar SNRBs a skin wheal is placed 1.5 cm lateral to the upper portion of the spinous process. A 5-cm, 25-gauge needle is directed vertically downward, while tissues along the way are infiltrated with 5-7 cc of a dilute LA solution (eg, 0.5% lidocaine or 0.125% bupivacaine) until the needle impinges upon the lamina of the vertebra. An 8-cm, 22-gauge needle is inserted perpendicular to the skin in the parasagittal plane through the anesthetized area, until the second needle reaches the uppermost part of the lateral edge of the lamina.
After contact with the lamina, the needle is marked 1.5 cm above the skin. The needle is then withdrawn until it is subcutaneous in location, then moved laterally approximately 1.5 cm and advanced past the lamina to a depth of 1.5 cm, where it should make contact with the nerve, eliciting paresthesia.
Needle placement can be verified by radiography, eliciting paresthesia, or using a nerve stimulator. See the images below.
For diagnostic or prognostic purposes, 2 cc of a potent LA solution (eg, 0.5% bupivacaine with epinephrine) is typically injected after radiographic verification of the position of the needle bevel. This volume is sufficient to block the nerve as it exits from the intervertebral foramen, provided the needle tip is within 1-2 mm of the nerve. For therapeutic purposes, 5 mL of solution can be used to prolong analgesia but this is likely to spread to one or more adjacent segments. Multiple nerve roots can be addressed by injecting 25-30 cc of LA solution into the psoas compartment, which contains the lumbar plexus. This spreads sufficiently to block sympathetic nerves, the lumbar plexus, and lumbosacral trunks.
Transforaminal epidural corticosteroid injections are advocated by many interventionalists for their capacity to provide diagnostic information often coupled with a therapeutic benefit. The approach to the prone patient using C-arm fluoroscopy to image the oblique "Scotty dog" is easy and usually safe in the competent and well-trained hands of a fulltime interventionalist. The 6 o’clock mark on the Scotty dog’s chin is the junction of the “dog’s ventral nose and the beginning of his neck is the target.”
The 22-gauge, 3.5-inch needle is walked off this bony landmark after it is withdrawn and then directed inferiorly. An AP fluoroscopic view is used to verify that the needle is not directed too far medially from the 6 o’clock mark on the pedicle, thereby avoiding a deep placement with its risk of entry into the dural sleeve or spinal canal. Correct needle placement is next verified by a lateral view with injection of 0.2-0.4 mL of a suitable contrast medium.
Contrast flow should flow proximally around the pedicle into the epidural space. Injections should be immediately stopped if a patient complains of pain upon injection. If epidural placement and satisfactory flow of contrast is observed, then 6 mg of betamethasone/solution or 20-40 mg of methylprednisolone or triamcinolone suspension with 0.5-2 mL of 2-4% preservative-free lidocaine or 0.5-0.75% bupivacaine is slowly injected in a total volume of 1-3 mL. Transient mild pressure and paresthesia are commonly noted.
Any bleeding tendencies, especially anticoagulation or coagulopathy, represent absolute contraindications for lumbar epidural spinal injections. Any evidence of local or systemic infection should call to question the relative need versus risk of the procedure due to the potential for hematogenous spread via the Batson plexus. Although infrequent, unintentional dural puncture occurs slightly more often using the transforaminal approach. This complication must be immediately recognized to prevent tragic consequences due to total spinal anesthesia, loss of consciousness, hypotension, and apnea. Complications seen with this approach at other anatomic levels have already been outlined at length. [19]
Lumbar paramedian epidural blocks
Lumbar paramedian epidural spinal blocks may be carried out in the sitting, lateral, or prone position, with the sitting position being favored for simplicity of patient positioning when compared with lateral position. [19] The patient is placed in the optimal sitting position with the lumbar spine flexed, and forearms placed on a padded bedside table. The skin is prepared with an antiseptic solution, usually at the L3-L4 inner space. The operator’s middle and index fingers are place to the side of the respective spinous processes. The position of the inner space is confirmed with palpation using a rocking motion in the superior and inferior planes. The midline of the selected inner space is identified by palpating the spine this processes above and below the interspace using the lateral rocking motion to ensure the needle entry site is exactly in the midline. See image below.
Approximately 1 mL of local anesthetic is used to infiltrate the skin and subcutaneous tissues, as well as the supraspinous and interspinous ligaments. A 25-gauge, 2-inch to 2.5-inch needle or an 18-gauge or 20-gauge, 3.5-inch needle is inserted exactly in the midline through the previously anesthetized area. The needle stylet is removed and a loss-of-resistance glass syringe filled with air or preservative-free normal saline is attached.
Alternatively, the physician can use a 12-cc plastic syringe filled with the intended injectate for also following loss the of resistance maneuver. By exerting constant pressure on the plunger of the syringe with the right hand, the right-handed physician advances the needle slowly with the left hand until lack of resistance is discerned. The operator uses the right hand to monitor resistance through a syringe containing air or preservative-free normal saline. With constant light pressure applied to the plunger of the syringe by the right thumb, the needle and syringe are advanced in a slow and deliberate manner. As the bevel passes through the ligament flavum and enters the epidural space, a sudden loss of resistance is noted.
If the operator appreciates it, the plunger can be depressed effortlessly under minimal, if any, pressure detected through the right thumb. Needle position within the epidural space can also be checked using fluoroscopic verification and by repeating the “loss of resistance” maneuver. The lumbar epidural space should accept 0.5-1 mL of air or sterile preservative-free saline without significant resistance. The force required to depress the plunger should not exceed that which is necessary to overcome the resistance of the needle.
Any significant pain or sudden increase in resistance during the injection suggests incorrect needle placement. The physician should immediately stop the injection and assess the position of the needle using fluoroscopy. If the needle remains satisfactorily placed and loss of resistance within the epidural space is confirmed without additional patient report of pain, gentle aspiration is checked to assure that the needle is not positioned in the subarachnoid space or that it is not intravascular. If CSF is aspirated, the operator can repeat the block attempt at a different interspace. If aspiration of blood occurs, the needle should be rotated tightly and the aspiration test repeated. If the aspiration of blood continues, the procedure should be aborted due to the danger of developing an epidural hematoma, and possibly neurological compromise. [19]
If the operator is confident that his needle is correctly placed in the midline of the intended epidural space, then injection of up to 5 to 7 mL of solution can be performed. For diagnostic and prognostic blocks, 1% preservative-free lidocaine provides adequate information. For therapeutic blocks, 0.25% preservative-free bupivacaine combined with 40-80 mg of methylprednisolone is commonly injected. In some cases. this procedure is repeated on a daily basis or every other day for the treatment of acute painful disorders that require pain reduction, even if only temporary. [19]
Lumbar facet block
Intra-articular lumbar zygapophyseal joint blocks, as described by Bogduk et al, are performed with the patient lying prone. Upper lumbar facet joints originate in the sagittal plane; therefore, the joint space is usually evident on posteroanterior fluoroscopy with the patient prone. The lower lumbosacral zygapophyseal joints are oriented obliquely at an angle of approximately 45° to the sagittal plane.
To permit visualization of the joint space, the patient has to be rotated appropriately and supported in an oblique prone position or a C-arm fluoroscopy unit capable of tilting the x-ray beam. A 22-gauge or 25-gauge, 9-cm spinal needle is the most practical for accessing the target joint cavity. Finer needles enter the joint space more easily but are apt to stray during penetration of the back muscles. If this difficulty is encountered, then a double needle technique can be used, in which a large gauge needle is introduced to the target joint and a finer needle is passed through the larger needle to penetrate the joint capsule.
The operator relies on feel to determine when the needle enters the joint and limits penetration of the joint no farther than its center. Correct placement of the needle inside the midpoint of the joint is confirmed by injection of a small quantity of contrast medium (less than 0.3 mL) using a small syringe (2-5 mL) to minimize injection pressure. If the needle is inside the joint, the arthrogram smoothly outlines the smooth perimeter of the joint space. At this point in the procedure, the patient should be questioned in detail whether the character of pain that is perceived as a result of the dye injection is concordant to the pain for which treatment is being sought. Once intra-articular placement has been verified, LA can be used to ablate the pain and provide additional diagnostic verification. Addition of corticosteroids has been reported to provide therapeutic benefit; however, no more than a total of 1 mL of any solution combination should be injected.
Lumbar medial branch blocks
Lumbar medial branch blocks, the technique of which also has been described by Bogduk et al, are performed under fluoroscopic guidance. The needle target for medial branch blocks of L1-L4 is on the dorsal surface of the transverse process, where it joins the superior articular process. The medial branch of each of these lumbar segments crosses the transverse process of the segment below; for example, the L4 medial branch crosses the L5 transverse process and so on. A 22- or 25-gauge, 9-cm spinal needle typically is used to perform the block. Larger needles are easier to maneuver through the back muscles, while finer needles are averted more easily from their intended course.
When using C-arm fluoroscopy, with the patient in a prone position, the image intensifier or the patient is rotated in a ipsilateral oblique angle with respect to the targeted nerve root, thereby bringing the “Scotty dog” appearance of the vertebral segment to view. Rotation of the C-arm or patient is continued until the ventral aspect of the superior articulating process (earof the Scotty dog) has the same vertebral number as the nerve root to be blocked. The anatomic site of the medial branch (at each targeted level) is located on the image of the Scotty dog in a groove formed by the transverse process (nose of the dog) where it joins the superior articular process (ear of the dog) with aim directed over the superior-lateral margin of the pedicle (eye of the dog), which is also approximately the 1 or 2 o’clock position of the eye for this obliquity. See image below.
Injections of the medial branch are primarily performed to determine whether or not a neurolytic procedure, which denervates the targeted posterior articulations, might provide long-term pain relief. [24]
Sacroiliac joint blocks
Sacroiliac joint blocks are challenging because the joint cavity lies deep to the corrugated interosseous surfaces of the sacrum and ilium and is joined by the dense interosseous sacroiliac ligament. Entry into the joint is most practical below the interosseous ligament deep to the gluteus maximus muscle along the upper margin of the greater sciatic notch. Using the technique described by Bogduk et al, the patient is placed in the prone position and a 25-gauge spinal needle is inserted through a skin wheal into the gluteus maximus and advanced until it engages the posterior aspect of the sacrum.
The operator must be cautious to avoid the greater sciatic foramen and redirect the needle toward the lower end of the joint space. Once the needle enters this slitlike opening, it is wedged between the sacrum and ilium and should be in the correct position. Penetration should be just deep enough to engage the slit; further penetration may cause the needle to emerge from the ventral surface of the joint. Contrast medium is then injected to verify placement and pain concordance. LA with or without supplementary agents may be injected for diagnostic and therapeutic purposes.
Caudal lumbar epidural spinal blocks
Caudal lumbar epidural spinal blocks have become more popular as a method of inducing epidural anesthesia and for catheter entry to locate specific spinal pain generators and to provide meaningful relief. To perform caudal blockade using the technique described by Brown, the patient is placed in a lateral decubitus or prone position. The prone position is more amenable to accurate identification of midline anatomical targets in adults. A pillow placed beneath the lower abdomen produces slight flexion of the lumbar spine. Mild sedation improves patient comfort. Relaxation of the gluteal muscles is induced in the prone patient by a 20° hip adduction and the feet pointed inward by internal rotation of the hips. A 25-gauge or 22-gauge needle varying in length from 1.5-3.5 inches is recommended for adult patients, and some needles allow introduction of a catheter, if desired, which can be directed under fluoroscopy using a steering wire. See the images below.
After the sacral hiatus is identified, the index and middle fingers of the palpating hand are placed on the sacral cornu and the caudal needle is inserted at an angle approximately 45° to the sacrum. As the needle is advanced, the operator can sense a reduction in resistance when the needle enters the caudal canal. The needle is advanced until bone is contacted on the dorsal aspect of the ventral plate of the sacrum. The needle is then withdrawn slightly and redirected at an angle more parallel to the skin surface. In male subjects this angle is usually about parallel to the tabletop, whereas in female patients a slightly steeper angle is often necessary. After the needle is redirected, it should be advanced approximately 1-1.5 cm into the caudal canal. Further needle advancement should be avoided to prevent unintentional intravascular cannulation or dural puncture. At this point in the procedure, a catheter can be threaded and directed by fluoroscopy to the desired spinal level and structures.
Caudal anesthesia and neural blockade are fraught with the same complications that can accompany lumbar epidural anesthesia; however, the incidence of subarachnoid puncture is much lower with the caudal technique. The dural sac ends approximately at the level of S2; therefore, unless the needle is inserted deeply within the caudal canal, subarachnoid puncture is unlikely. The most commonly encountered problem with caudal anesthesia is ineffective neural blockade.
Sympathetic Nervous System Blockade
Complex regional pain syndromes (CRPS) develop as an exceedingly disproportionate consequence relative to the causative trauma affecting the limbs. Causalgia (CRPS 2) is a painful disorder that results from traumatic nerve injuries, most commonly when such damage is partial. Causalgia is a syndrome of sustained, diffuse, burning pain; allodynia (pain produced by non-noxious stimuli) with hyperpathia (painful overreaction to stimuli); and vasomotor and sudomotor disturbances.
When advanced, CRPS 2 is associated with trophic changes of the affected tissues. Treatment of CPRS 1 and 2 entails sympathetic denervation of the entire limb, thus LA volume and concentration with diffusion must be sufficient to block the entire portion of the sympathetic chain that supplies the affected extremity. Following sympathetic interruption, patients should be questioned and urged to keep a diary as to the extent and duration of relief from burning pain, hyperpathia, allodynia, and sudomotor changes.
Three "critical sites" can be used to interrupt the peripheral sympathetic nervous system: the cervicothoracic (stellate) ganglion, celiac plexus, and lumbar sympathetic plexus. Usually, injection of 15-20 mL of an LA solution into the proper fascial plane near the stellate ganglion allows for sufficient spread to block the sympathetic chain from the superior cervical ganglion to the T5 ganglion, thereby inducing interruption of sympathetic innervation to the head and neck, upper extremities, heart, and most of the esophagus and lungs. Likewise, sufficient spread of 15-25 mL of an LA injectate near the celiac plexus should interrupt all sympathetic (and vagal), efferent, and afferent fibers serving the viscera in the upper abdomen. Injection of 15-20 mL at the anterolateral surface of the L2 or L3 vertebral body interrupts sympathetic innervation to the ipsilateral lower extremity and pelvis.
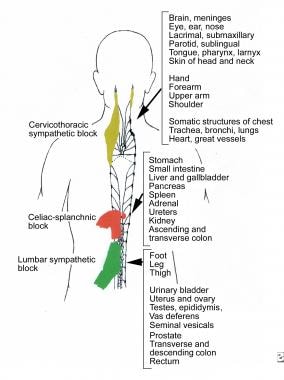 Three important sites that can be used to interrupt the peripheral sympathetic nervous system. The colored areas represent patterns of diffusion of local anesthetic solutions for the following techniques: cervicothoracic sympathetic block, celiac-splanchnic block, and lumbar sympathetic block.
Three important sites that can be used to interrupt the peripheral sympathetic nervous system. The colored areas represent patterns of diffusion of local anesthetic solutions for the following techniques: cervicothoracic sympathetic block, celiac-splanchnic block, and lumbar sympathetic block.
Sympathetic blockade is often useful for other pain disorders, including postamputation pain syndromes and peripheral vascular disease, such as acute or chronic occlusive arterial disease and vasospastic disorders. Blockade of sympathetic nerves to the thoracic or abdominal viscera often alleviates severe visceral pain that is not amenable to other therapies. Thoracic visceral pain, such as that of acute myocardial infarction and angina pectoris, may activate reflex coronary vasoconstriction by segmentally induced sympathetic stimulation, which conversely further aggravates cardiac ischemia.
In these cases, cervicothoracic sympathetic blockade and, if necessary, neurolytic sympathectomy may be considered useful as adjunctive treatments. Celiac plexus block or continuous segmental T5-T10 block can be used to interrupt nociceptive afferents associated with pancreatitis, biliary and ureteral colic, and adynamic ileus, as well as painful visceral conditions caused by malignancy. Sympathetic blockade at the appropriate segmental level also has been prescribed in cases of acute herpes zoster and postherpetic neuralgia.
Cervicothoracic sympathetic block is also referred to as "stellate ganglion block;" and it usually is performed by an experienced anesthesiologist for the indications previously outlined. Using the technique described by Brown, the patient is placed in supine position with the neck in slight extension. The operator then identifies the sixth cervical vertebral tubercle by locating the cricoid cartilage and moving the fingers laterally until they reach this easily palpable structure. The anesthesiologist then places the index and third fingers between the carotid artery laterally and the trachea medially at the level of C6. A short 22- or 25-gauge needle is inserted until it contacts the transverse process of C6. The needle is then withdrawn approximately 1-2 mm and 5-10 mL of LA injected. Care must be taken not to perform intravascular injection or LA blockade of the recurrent laryngeal and phrenic nerves.
Blockade of the thoracic sympathetic chain is a useful diagnostic and therapeutic procedure for identifying segmental nociceptive pathways, which may be causing pain due to inflammatory, infectious (herpes zoster), or structural pathology. Celiac plexus block should be performed by a skilled anesthesiologist for relieving severe pain caused by an acute visceral disease. Using the technique described by Brown, the patient is placed in prone position over a pillow placed beneath the abdomen to reduce lumbar lordosis.
The lumbar and twelfth thoracic vertebral spines are identified and marked, and parallel lines to the vertical axis of the spine are drawn 7-8 cm from the axial midline. Then the tip of the twelfth rib is palpated and marked. Another mark is placed in the midline between the twelfth thoracic and first lumbar vertebral spines. Connecting lines between these 3 marks produce a flat isosceles triangle. Skin wheals are placed over the marks immediately below the twelfth rib, and a 12-15 cm, 20-gauge needle (without the syringe) is inserted.
The needle is inserted between the T12 and L1 vertebral spines in a plane that is 45° to the horizontal table. This placement allows contact with the L1 vertebral body at a depth of 7-9 cm. More superficial bony contact is usually caused by needle impingement upon a vertebral transverse process. C-arm fluoroscopy is helpful for guiding the direction and depth of the needle. After the vertebral body is identified clearly, the needle is withdrawn to subcutaneous level and the angle changed to allow the tip to slip past the lateral border of the vertebral body.
After the needle tip passes by the vertebral body, it should be inserted an additional 1.5-2 cm or until it approaches the aortic wall, which can be recognized by transmission of pulsations from this vascular structure through the needle. On the right, the needle insertion can be placed deeper, approximately 2-3 cm beyond the vertebral body. Aspiration after needle placement is critical prior to the injection of LA or a neurolytic agent. Besides blood, faulty needle puncture may yield urine or CSF.
Lumbar sympathetic blockade also should be performed by an experienced anesthesiologist, preferably using C-arm fluoroscopic guidance. Using the technique described by Brown, the patient is placed in prone position. The second or third lumbar vertebral spines are identified, and a mark is placed on the skin 7-9 cm lateral to the midline. A skin wheal is raised using a 15-cm, 20- or 22-gauge needle, which then is inserted through the skin at an angle of 30-45° from the vertical plane ascribed to the patient's midline. The needle is advanced until it contacts the lateral aspect of the L2 vertebral body.
Superficial contact usually is caused by encroachment upon the transverse process. The needle is repositioned and redirected in a cephalad or caudal manner to avoid the transverse process. The target position for the needle is the anterolateral surface of L2. When the needle is in position, and after aspiration, 15-20 mL of LA solution, usually 0.5% lidocaine or 0.125-0.25% bupivacaine, is injected.
Complications are rare but can occur, including accidental injection into the inferior vena cava on the right or the aorta on the left, damage to lumbar vessels, and unintentional needle penetration or anesthesia to neighboring somatic nerves. Sympathetic nervous system monitoring (which has not been discussed in detail) determines the presence and extent of sympathetic blockade.
Intravenous regional sympathetic blockade entails injection of an antiadrenergic agent into the venous system of a limb with CRPS after the circulation is occluded temporarily with a tourniquet. An experienced interventionist, preferably an anesthesiologist, should perform this procedure. This procedure was originally developed using guanethidine, which can induce a prolonged, unselective sympathetic blockade by displacing NE from presynaptic vesicles and preventing NE uptake.
Guanethidine causes an initial release of NE, followed by NE depletion, which results in long-lasting interruption of adrenergic activity. Blockade may last for hours, days, and occasionally, weeks because of the high affinity of guanethidine for binding to sympathetic nerve endings, and also because guanethidine is eliminated slowly. Unfortunately, parenteral guanethidine is no longer available, since the drug is no longer used for the treatment of hypertension by the IV route.
Other possible candidates for alpha-adrenergic blockade include reserpine, which causes NE storage vesicle depletion and blocks NE reuptake; however, this drug has proved relatively ineffective and produces many adverse effects. Blockade of presynaptic (alpha2) and postsynaptic (alpha1) receptors can be performed with phentolamine, which is reversible, usually with duration of effect of less than 24 hours.
Blockade of postsynaptic (alpha1) receptors can be induced by prazosin; however, a parenteral form of this drug has not yet been approved, and investigation for this indication is insufficient to date. IV sympathetic blockade is particularly useful for patients in need of sympathetic blockade who are taking anticoagulant medications. Patients who are sensitive or experience excessive toxic systemic reactions to LA may be candidates for IV blockade.
Problems with the use of guanethidine include the initial effect of the drug, which causes an increase in NE and consequent cutaneous vasoconstriction, piloerection, and burning dysesthesia. Some of the guanethidine that escapes occlusion of the circulation by tourniquet may produce side effects including tachycardia and dizziness, as well as other signs and symptoms of sympathetic blockade. Cardiac, blood pressure, and other vital signs should be monitored closely, and appropriate resuscitative measures and equipment should be available at the bedside.
Patient anxiety may increase with the transient rise in NE levels secondary to the guanethidine effect. Prior to the procedure, 100 mg of thiopental, 5-10 mg of IV diazepam, or 3-5 mg of IV morphine should be considered to minimize the pain and discomfort inherent to the procedure. Pain resolution associated with regional infusion of guanethidine can be considered sympathetically mediated from a diagnostic standpoint. Repeating this procedure on an outpatient basis may be necessary; patients with severe CRPS may require re-treatment every 3 days, whereas patients with milder CRPS may require therapeutic intervention only at 3-week intervals. Usually, treatment is limited to 2-3 sessions.
IV neural blockade is performed using a technique similar to that described for IV sympathetic blockade. The patient is prepared for IV infusion in the affected limb. The limb is elevated, and the tourniquet is inflated to a pressure above the patient's systolic blood pressure. Using a 50-mL disposable syringe, 30-40 mL of 0.5% lidocaine or procaine, without epinephrine or other vasoconstrictors, is injected slowly. The skin often becomes mottled as the injection proceeds, and analgesia develops rapidly. Adequate analgesia often develops within 5-10 minutes.
Tourniquet discomfort may require adjunctive systemic injections of sedatives or narcotics; however, concomitant opioid use can confound diagnostic interpretations. Usual indications for this procedure include CRPS syndromes, neuralgia, and deafferentation pain. IV lidocaine in doses of 1-1.5 mg per kilogram of body weight, or in a 0.1% solution administered over 35 minutes to 200 mg, are alternative technical approaches for this procedure.
Successful neural blockade by continuous infusion may allow the pain medicine specialist to consider oral lidocainelike derivatives such as mexiletine. To this point, neural blockade and therapeutic procedures that have been described entail the use of LAs. However, LA blockade of certain painful conditions may lead treating practitioners to consider a neurolytic agent for more permanent pain relief.
Neurolytic blockade is an important tool because it offers the potential for long-term relief from severe pain caused by conditions such as advanced cancer, certain neuralgias, and incurable conditions such as occlusive vascular disease. Neurolytic cranial nerve blocks, subarachnoid block, celiac plexus block, and lumbar sympathetic block, when properly executed, result in a high degree of success with acceptably low instances of adverse effects in patients who have not obtained satisfactory relief by other methods.
Practitioners with extensive experience, skill, and knowledge of the pharmacology and application of neurolytic agents should perform these procedures. Informed consent including potential outcomes and adverse effects should be expressed clearly through practitioner-patient communication.
Examples of neurolytic agents include alcohol in concentrations of 35-100%. Alcohol produces nerve fiber destruction, which results in wallerian axonal degeneration. If cell bodies at the level of the dorsal root ganglia are destroyed, no regeneration takes place, whereas if they are destroyed only partially, regeneration may occur.
Phenol often is used to induce prolonged sympathetic, somatic nerve, subarachnoid, and epidural blockade. Phenol is similar to alcohol in regards to its potency and nonselective damage to the nervous system. Injection concentrations of phenol usually vary between 5% and 8%. Concentrations above 5%, when applied to peripheral nerve, cause protein coagulation and necrosis with axonal degeneration and subsequent wallerian degeneration.
Injection of glycerol into the trigeminal ganglion has been popularized for the treatment of neuralgia because of its capacity to relieve pain without causing significant sensory deficits. Topical application of a 50% glycerol solution to nerves causes localized subperineurial damage, whereas intraneural injection is more damaging and causes axinolysis.
Cryotherapy, laser, and radiofrequency lesions are currently under investigation and are advocated as being effective for neurolytic procedures when performed by trained and experienced interventionists. Further clinical research is needed to develop methods that preferentially block nociceptive pathways (ie, strict neurolytic blockade that spares large myelinated sensory fibers).
Neuraxial neurolytic blocks are advocated to alleviate severe intractable pain caused primarily by advanced terminal cancer. The use of these techniques for chronic, nonmalignant pain should be discouraged. Agents used for this purpose include ethyl alcohol, phenol in glycerin, chlorocresol in glycerin, aqueous phenol, hypertonic saline solution, and ammonium compounds.
Subarachnoid neurolytic block is used to relieve severe pain resulting from continuous nociceptive impulses from skin, subcutaneous tissue, deep somatic structures, and viscera. Neurolytic agents are aimed by positioning the patient depending on whether the destructive agent is hyperbaric or hypobaric, so that the axons of the posterior rootlets are destroyed upon contact, thereby affecting neural input from the dorsal root ganglion to the spinal cord.
Subarachnoid neurolysis also can be used effectively for managing patients with spasticity. Intrathecal neurolysis is not associated with significant pain and causes few serious complications; therefore, it can be performed on patients who are in poor physical condition and on elderly patients. Only a brief hospital stay may be necessary; therefore, it is more available to patients than other techniques because it requires no special costly or highly sophisticated equipment or facilities. Neurolytic injections can be repeated or extended if pain spreads or persists. Subarachnoid neurolytic block can delay or avoid neurosurgical procedures, and the duration of pain relief is usually sufficient to afford adequate comfort for patients with terminal cancer.
Intrathecal neurolysis for the management of cancer pain is not, however, devoid of problems and disadvantages. Inadequate pain relief may result from failure of the injection to interrupt all nociceptive pathways completely or from spread of the pain beyond the anesthetized region following the injection. Although the block initially may interrupt nerves to the painful region and afford relief of the pain, aggressive neoplasms often spread beyond the confines of induced analgesia to cause additional symptoms. Fortunately, the block can be repeated several times without further taxing the patient's already overburdened physiological status.
Complications may occur during or following the procedure, such as muscle weakness affecting the limbs or rectal and bladder sphincters. Contraindications for subarachnoid neurolysis include pain that is diffuse or poorly localized; tumor infiltration with involvement of the spinal cord or vertebral column at the level of injection; and inadequate pain relief despite repeated LA test blocks. Epidural and subdural neurolytic blockade also can be used with similar techniques as mentioned above and for similar indications.
Subarachnoid and epidural spinal blockade
Subarachnoid block, also termed spinal anesthesia (SA), can be achieved with small amounts of LA (eg, 100-150 mg procaine, 50-100 mg lidocaine, 5-15 mg bupivacaine) placed into the subarachnoid space where it readily mixes with the CSF. SA produces a rapid onset of analgesia because the drug comes into direct contact with neural structures, especially nerve axons, without first traversing the epineurium and perineurium. Furthermore, SA is a relatively simple procedure when administered by experienced hands and allows better control of the degree and duration of neural blockade. LA solution can be made hyperbaric (ie, specific gravity CSF), which allows the spinal level of the block to be controlled by changing the position of the patient.
Notwithstanding, these advantages of SA have limited value when managing patients with acute pain, and SA is rarely indicated as a therapeutic tool for patients with chronic pain. SA is frequently useful as a prognostic block prior to a subarachnoid injection of a neurolytic agent or for diagnostic purposes.
Differential subarachnoid block can be used as a diagnostic procedure in differentiating pain caused by somatic nociceptive sensory nerves, sympathetic hyperactivity, and pain from a primarily central source, including that of psychogenic etiology. Classically, this is performed by an anesthesiologist who inserts a microcatheter into the subarachnoid space. Bonica described a technique using a 32-gauge polyamide catheter, 91 cm long, which can be inserted through a 25-gauge or 26-spinal gauge spinal needle. During the procedure, cardiorespiratory monitoring, as well as sympathetic, sensory, and motor neural assessment, should be ongoing. After insertion of the catheter, 8-10 mL of saline solution are infused as control. Some anesthesiologists have advocated aspiration of 8 mL of CSF and then CSF re-injection because of the controversial belief that isotonic saline solution may induce a change in sensation.
The operator then injects 8-10 mL of 0.25% procaine, which should produce a sympathetic neural blockade; sympathetic neural functions are monitored, as well as any reported changes in the patient's pain. Subsequently, 8-10 mL of 0.5% procaine is injected to produce a sensory block, which can be assessed by pinprick, touch, and pinch. Finally 8-10 mL of 1% procaine is injected to produce a motor blockade. During each stage of the procedure, the patient's pain intensity, spinal level of the sensory block, and neurophysiological and behavioral changes, as well as the quality of the analgesic effect, are monitored.
Pain that responds to isotonic saline or "placebo" is presumed to have a non-nociceptive origin; therefore, possible contributing psychogenic factors should be evaluated. If a sympathetic blockade accompanied by objective evidence of sympathetic interruption alleviates the pain, sympathetic hyperactivity may account for a component of the pain. Elimination of the pain with 0.5-1% procaine should indicate that the pain has a somatic origin. Failure of any solution to block the pain also implies a central or psychogenic etiology.
Extradural or epidural blockade can be varied to suit the spinal segmental level of the patient's symptoms. Blockade can be achieved with a single injection of LA through a needle placed at the appropriate segmental level or by introduction of a catheter through a thin-walled 18- or 17-gauge needle placed at the spinal level, which is considered clinically to be the optimum site for injection. Injections into the lumbar epidural space can be accomplished through either a caudal or lumbar approach.
The lumbar approach involves passing the needle through the intralaminar space along the midline through the interspinous ligament or slightly to the side of the ligament, then penetrating through ligamentum flavum to enter the epidural space. Perceived advantages of the lumbar route are (1) the needle is directed more closely to the assumed site of pathology, (2) the drug to be injected can be delivered directly to its target (ie, more target specific), and (3) lesser volumes of the injected solution can be used.
Continuous epidural block often is used to eliminate chronic persistent pain secondary to somatic, visceral, or sympathetic etiologies. This procedure can be used for relieving the severe pain associated with pancreatitis, biliary colic, renal or ureteral colic, multiple fractures of the ribs, and severe posttraumatic pain. Postoperative pain of the thorax, abdomen, pelvis, and/or lower limbs is also a common indication. In all these acute conditions, blockade provides not only analgesia by interruption of nociceptive pathways from somatic structures and viscera, but also blocks reflex muscle spasm, sympathetically induced ileus, and neural endocrine responses that may codevelop with acute injury and disease. Continuous epidural anesthesia also can be achieved using minute doses of soluble opioids.
Chemodenervation with Botulinum Toxin for Pain Treatment
Botulinum toxin (BTX) is a potent neurotoxin produced by the gram-positive, spore-forming, anaerobic bacterium Clostridium botulinum. The 7 immunologically distinct serotypes of BTX are as follows: types A, B, C1, D, E, F, and G. Only types A and B have been developed for commercial use in routine clinical practice. Three type A (BTX-A) preparations have been developed: onabotulinumtoxinA (BOTOX®; Allergan, Inc; Irvine, CA), incobotulinumtoxinA (Xeomin; Merz Pharmaceuticals, LLC; Greensboro, NC) and abobotulinumtoxinA (Dysport; Medicis Pharmaceutical Inc; Scottsdale, AZ). Type B is currently commercially available as Myobloc in the United States.
Each of these neurotoxins are proteins and vary with respect to molecular weight, mechanism of action, duration of effect, and adverse effects. Each toxin is initially synthesized by the bacteria as a single chain polypeptide. Bacterial proteases then "nick" both type A and type B proteins, resulting in a dichain structure consisting of 1 heavy and 1 light chain. Type A is nicked more than type B, and the homology between the toxins is less than 50%. [25]
The mechanism by which acetylcholine release is blocked by BTX is presently better understood than other antinociceptive mechanisms by which these neurotoxins exert their analgesic effects. The toxin first binds to a receptor on the motor nerve terminal at the neuromuscular junction. Each BTX serotype specifically and irreversibly binds to its own receptor, and each neither binds to nor inhibits the other serotypes' receptors. [26, 27]
The binding domain of the toxin appears to be the heavy chain. BTX is then internalized by acceptor-mediated endocytosis into the cholinergic synaptic terminal. After the toxin is bound, an endosome is formed that carries the toxin into the axon terminal. The final step involves cleavage of one of the known synaptic proteins that are required for acetylcholine to be released by the axon. BTXs A, E, and C cleave synaptosome-associated protein-25 (SNAP-25). BTXs B, D, F, and G cleave synaptobrevin, also known as vesicle-associated membrane protein. BTX type C also cleaves syntaxin. [25] The specific manner in which each toxin type may cleave the synaptic protein as well the specific differences in effect on inhibiting acetylcholine release is beyond the scope of this clinical summary. How these differences translate into various observed beneficial and adverse effects is unclear.
In December 1989, BTX-A (BOTOX®) was approved by the United States Food and Drug Administration (FDA) for use in the United States for the treatment of strabismus, blepharospasm, and hemifacial spasm in patients aged 12 years and older. In December 2000, BOTOX® was subsequently approved for the treatment of cervical dystonia in adults to reduce the severity of abnormal head posture and pain associated with cervical dystonia. In April 2002, BOTOX® was approved for the treatment of glabellar wrinkles. In July 2004, BOTOX® was approved by the FDA for primary axillary hyperhidrosis that is inadequately managed by available topical agents. In March 2010, BOTOX® was FDA approved for the treatment of upper extremity spasticity, which is often painful. In October 2010, BOTOX® was approved for the prophylaxis of headaches in adult patients with chronic migraine (≥15 d/mo with headaches lasting ≥4 h/d).
BTX type B (BTX-B) is currently FDA-approved for the treatment of cervical dystonia. [28] Despite the fact that neither FDA-approved BTX is approved specifically as an analgesic, the analgesic effects of these agents has been observed (eg, the ability for these toxins to reduce the pain associated with cervical dystonia). In fact, the analgesic effect of the neurotoxins appeared to have a greater duration of action than other more direct neuromuscular effects. [29]
Following injection of the toxin into muscle, a "BTX-effect" (eg, weakness) occurs within a few days, usually peaks within 2 weeks, and then gradually returns to baseline. This recovery of strength is associated with new axonal growth or "sprouting" at the affected neural site and the return of cholinergic synaptic activity to the original nerve terminals. Regeneration of the cleaved synaptic protein is required for recovery to occur. The duration of the clinical effect of the currently available neurotoxins appears to be approximately 3-5 months in humans but may vary.{{Rerf198} [30, 31] Additionally, the possible differences in duration of action of these toxins for different clinical conditions (eg, cervical dystonia, migraine headache, chronic low back pain) may be due to this variation, at least in part.
Therefore, the toxins' primary mechanism of action has been linked to their ability to inhibit the release of acetylcholine from cholinergic nerve terminals; however, most experts acknowledge that this effect appears inadequate to explain the entirety of the neurotoxin's apparent analgesic activity exhibited by these toxins. [32] Consequently, research has demonstrated other mechanisms of action that might also explain the analgesic effects of BTX. These mechanisms are multiple and have been demonstrated in animal studies; therefore, their clinical effect in humans, if any, can only be estimated.
Some of these neurophysiologic actions on pain are inhibition of glutamate; release of substance P and calcitonin-gene related peptide; reduced afferent influence on the central nervous system through the toxin's effects on muscle spindles; and other possible effects on pain transmission. [33, 34, 35] In addition to reduced glutamate release in the peripheral nervous system, compared with animal controls, BTX-inhibition of the expression of C-fos in the dorsal spinal cord in treated animals was observed. Two reviews were published that elucidated and summarized the multiple noncholinergic mechanisms of BTX, which may explain its analgesic effect. [36, 37]
Of particular note, Cui and colleagues performed a placebo-controlled study on rats who received subcutaneous (SC) injections of BTX-A into their paws before being exposed to the formalin model of inflammatory pain. [38] The BTX-treated rats experienced a significant dose-dependent inhibition of both the acute and secondary pain responses. [39, 38]
Aoki later studied whether the action of SC BTX-A to inhibit inflammatory pain in the rat formalin model was due to a direct action on sensory neurons. [40] Using microdialysis, Aoki discovered that BTX-A significantly inhibited formalin-induced glutamate release and reduced the number of formalin-induced C-fos-like immunoreactive cells in the dorsal horn of the spinal cord. Also, BTX-A significantly inhibited excitatory activity of wide dynamic range neurons in the dorsal horn characteristic of phase II of the formalin response. Inhibition of neurotransmitter release from primary sensory neurons was shown in this study and may act as the primary mechanism for BTX-A's inhibition of peripheral sensitization, which may also indirectly reduce central sensitization.
BTX for the management of musculoskeletal pain
Multiple studies have looked at the neurotoxin's potential for treatment of painful musculoskeletal conditions, including chronic myofascial and spinal pain syndromes.
Musculoskeletal pain is often attributed to myofascial pain syndrome (MPS). Of patients with pain presenting to various specialists, the prevalence of MPS has been reported to vary from 30-90%, depending on the subspecialty practice and setting. MPS is characterized by painful muscles with increased tone and stiffness containing trigger points, which are tender, firm nodules, or taut bands, usually 3-6 mm in diameter. Palpation produces aching pain in localized reference zones.
Mechanical stimulation of the taut band by needling or brisk transverse pressure produces a localized muscle twitch. Trigger point palpation often elicits a "jump sign"—an involuntary reflexlike recoil or flinching from the pain—that is disproportionate to the pressure applied. Multiple treatments, including trigger point injections, have long been advocated; however, reports conflict as to whether any therapeutic substance injected into a muscle provides more benefit than dry needling alone.
The pathogenesis of myofascial trigger points is unknown; however, Simons postulates that abnormally increased motor endplate activity caused by excessive release of acetylcholine at the neuromuscular junction results in spontaneous electrical activity and extrafusal muscle contraction in the immediate vicinity of the extrafusal muscle end plates, thus forming the taut band and trigger point. [41]
Numerous studies have examined the role of BTX for treating chronic cervical-thoracic pain associated with myofascial pain and dysfunction. In a randomized, controlled, crossover study, Cheshire et al injected myofascial trigger points in the cervical and shoulder region in 6 patients with either BTX-A (50 U spread out over 2-3 areas) or normal saline (NS). [42] Crossover occurred at 8 weeks. Four of the 6 patients reported at least 30% pain reduction, as measured by visual analogue scales (VAS), with BTX-A, but not saline injections.
In a randomized, double-blind, prospective, placebo-controlled study by Wheeler et al, 33 patients with a single cervical myofascial trigger point were injected with either 50 U or 100 U of BTX-A or normal saline. [43] All 3 groups showed significant treatment effects as measured by VAS, psychometric testing, and pressure algometry. Group differences were apparent only when the authors considered the number of patients who were asymptomatic from the injections, but no clear statistically significant benefit of BTX-A over placebo was demonstrated over 4 months.
However, a striking difference in treatment response was noted between the participants in the 2 BTX-A treated groups compared with those in the initial placebo group who elected to receive a second, unblinded BTX-A 100 U injection into the same trigger point. Using the same measurement criteria, this second study arm showed a beneficial effect from BTX-A, but the small number of participants precluded meaningful statistical analysis. [44]
In a follow-up open-label study, Wheeler and Goolkasian examined a 44 patient-cohort with refractory cervical-thoracic (73%) or lumbosacral (9%) muscular pain (or both) who received BTX-A treatment in a private outpatient clinic combined with physical therapy. [43] BTX-A treatment was directed at painful muscles with spasm or trigger points. BTX-A dosages were tailored to meet individual patient needs and varied between 50-200 U. Eighty percent of all patients reported significantly reduced pain after their initial treatment session. Forty-one percent of patients who only underwent one treatment session and an additional 27% who required a second injection session still reported "adequate pain relief" when contacted 2 years later.
However, in a third follow-up study, Wheeler and colleagues were unable to detect any statistically significant differences in pain reduction between BTXA and placebo-treated patients with painful cervical-thoracic paraspinal and trapezius muscles using higher total doses of BTX-A (eg, 200-300 U/session), similar to treatment doses commonly used for cervical dystonia.
In the studies described so far, physicians have used similar injection methodology by placing the neurotoxin into symptomatic trigger points, a practice consistent with the treatment techniques originally described by Simons et al. [45]
However, some advocate placement of BTX into the muscle's motor point (eg, into standardized sites in the mid-belly of affected muscles). [46] Using a BTX treatment technique that involved injecting the muscle in it's motor point pattern with doses of BTXA ranging from 20-600 U, Lang studied the treatment of 72 patients who received 95 injection session treatments. [46] Sixty percent of patients experienced good-to-excellent results at 22-60 days following injection.
In a 12-week randomized, double-blind, placebo-controlled study, 132 patients with cervicothoracic myofascial pain were treated with BTX-A or saline by Ferrante et al. [47] No significant differences in outcome were seen between groups. Patients receiving BTX-A were treated with a total of 50-250 U of toxin divided among 5 injection sites.
Porta, in a single blinded study, evaluated the difference between lidocaine/methylprednisolone injections compared with BTX-A injections into symptomatic myofascial trigger points in the psoas, piriformis, or scalenus anterior muscles; [48] 80-150 U of toxin were used. Each group received benefit, but the toxin-treated patients experienced a greater duration of relief.
Opida presented 31 patients with posttraumatic neck pain who he treated with BTX-B injections in an open-label study. [49] Seventy-one percent of his patients reported significant reductions in headache pain frequency and severity. In 2 separate open-label studies, Taqi and colleagues showed that either type of BTX may be effective in the treatment of myofascial pain. [50, 51] Several case reports using BTX-B injections in the management of chronic myofascial pain have suggested overall beneficial results. [52, 53, 54]
Several publications, including a case report and an open-label study involving 77 patients, have emphasized the benefit of BTX in the management of chronic myofascial pain. [55, 56, 57] One published review of BTX-A treatment for chronic musculoskeletal pain found no clinical evidence of its beneficial efficacy, despite scientific evidence of BTX analgesic qualities. [58]
Reports of the use of BTX for treatment of piriformis muscle syndrome included a randomized, controlled, crossover study of 9 patients who were treated with 100 U of either BTX-A or placebo using EMG and fluoroscopic guidance for injection placement. Childers and colleagues reported a trend toward greater pain relief for patients receiving toxin as opposed to placebo. [59] Fanucci and associates reported that 26 of 30 patients with piriformis syndrome who were injected with BTX-A under computerized axial tomographic guidance obtained relief of their symptoms within 5-7 days. [60]
Fishman et al performed 2 studies looking at BTX use for patients with piriformis syndrome. In one noncontrolled study, the authors concluded that BTX-A injections may be a useful adjunctive measure to physical therapy in the management of this syndrome. [52] In a follow-up dose-ranging study with BTX-B for piriformis syndrome using EMG guidance, Fishman reported that patients experienced notable symptom improvement. [61]
A double-blind, randomized, controlled study of BTX-A use for chronic myofascial pain compared 30 patients with trigger points in the infraspinatus muscle. Subjects were divided into a treatment group who received 50 U/0.25 mL saline or a placebo group who just received 0.25 mL of isotonic saline. Outcome measures included localized and referred pain, pain detection and tolerance thresholds to mechanical pressure (electronic algometer), and shoulder movement assessed at 3 and 28 days after injection. EMG interference patterns were evaluated at baseline and at 28 days following BTX-A injections. BTX-A significantly reduced motor endplate activity and EMG interference patterns; however, no significant differences were found in any of the outcome measures between groups.
BTX-A has antinociceptive and muscle-spasmolytic properties that may be hypothesized to alleviate signs and symptoms of myofascial pain syndromes (MPS). A prospective, double-blind 12-week, multicenter, randomized controlled trial by Gobel et al found that patients with upper-back MPS who received injections of 400 Ipsen units of BTX-A (Dysport) to 10 individual trigger points demonstrated significantly improved pain levels at 4-6 weeks after treatment without adverse side effects. [62]
Lew et al enrolled 29 study participants from 45 screened patients in a double-blind, randomized controlled trial to determine the efficacy of BTX-A in treating neck and upper-back pain of myofascial origin. [63] Study subjects received a one-time injection of either BTX-A or NS. Outcome measures included the VAS for pain, the Neck Disability Index (NDI), and the 36-item Short-Form Health Survey (SF-36).
Participants were evaluated at 2 weeks and at 1, 2, 3, 4, and 6 months. Improvements in the VAS and NDI scores were seen in both groups, but differences were not statistically significant between the treatment and comparison groups. However, statistically significant improvements were seen in the SF-36 bodily pain (at 2 mo and 4 mo) and mental health (at 1 mo) scales in the BTX-A treated group. Therefore, the authors could only surmise that trends towards improvement in the VAS and NDI scores did not show a BTX-A effect that could be differentiated from placebo effect; however, a larger study using the same or similar psychometric measures is warranted. No serious adverse events were reported.
BTX for the treatment of neck pain due to whiplash associated disorders
Padberg et al conducted a randomized controlled trial in 40 patients who experienced chronic pain due to whiplash-associated disorders (WAD). [64] Study participants were randomly assigned to receive BTX-A (maximum 100 U) or placebo (NS) into muscles that were felt to be symptomatic by demonstration of increased tenderness. No significant differences could be determined between groups at 4, 8, and 12 weeks as measured by neck pain intensity using VAS, mean number of neck pain days or pain hours per day, days requiring treatment for symptoms, number of analgesics taken per day, and cervical range of motion. No significant improvement was noted after 4, 8, and 12 weeks. This study did not show any beneficial treatment effect when tender muscles, presumed to be due to WAD, were injected with BTX-A.
Similar findings were noted by Carroll et al in a prospective, double-blind, randomized controlled trial. [65] In this study, 37 patients with symptomatic WAD lasting longer than 2 months were randomized to receive either 250 U BTX-A (Dysport) or NS. Each received 4 trigger-point injections of 0.625 mL. Tenderness to palpation, VAS scores, the Vernon-Mior Index, and cervical range of motion were assessed at baseline, at 4 week,s and at 3 months after treatment. The findings of this study were consistent with most previous studies in showing a tendency towards improvement in all measures in both groups. However, changes in the Vernon-Mior Index, which measures pain and disability, were both statistically and clinically significant in the BTX-A group. Group comparisons did not meet statistical significance. The authors were optimistic in suggesting that BTX-A may have a beneficial role in the treatment of WAD, but larger studies are necessary to determine any such use at present.
Tender points due to WAD, rather than trigger points, were injected by Braker et al in 20 patients diagnosed with cervical MPS, 2-48 weeks after injury. [66] Patients were randomly assigned to receive either 200 U of BTX-A or placebo at 4 tender points, and progress was measured at 3, 6, 9, 12, and 24 weeks following the injection session. Outcome measures included VAS intensity scores, 5-point Verbal Rating Scale (VRS), quality of life assessed by the SF-36 questionnaire, global assessment scores by both physician and patient, tenderness from mechanical pressure, and cervical range of motion. These data are confounding because some patients, who were acute or subacute, were likely to improve based on natural history. The authors' observations of a time-dependent improvement in all the parameters is suspect as a study result.
Consistent with prior cervical studies, improvement was demonstrated in both groups, and although improvement was larger in the BTX-A group, the difference was not statistically significant. Systemic adverse effects were more common in the BTX-A group (40% vs 0%, P=0.07). The authors joined suit in recommending the need for a larger well-designed clinical study.
To investigate the efficacy and tolerability of BTX-A in patients with refractory neck pain, 47 subjects were enrolled in a prospective, double-blind, randomized controlled trial. [67] Participants received a total of 150-300 units of BTX-A injected into the neck and shoulder muscles based on pain localization and the area involved. Subjects completed the VAS (pain intensity), Pain Frequency Questionnaire, and the Modified Oswestry Pain Questionnaire (MOPQ) at baseline and 3 and 8 weeks after the treatment. Primary outcomes consisted of (1) 50% or more improvement on the VAS and (2) 30% or more reduction in pain day frequency. Secondary outcome was improvement of activities of daily living in the MOPQ. Excellent responders (ERs) were those who met all 3 outcomes.
At 2 months, a significant reduction in the mean VAS was noted in the BTX-A group compared with placebo; 6 ERs were found in the BTX-A group compared with 1 ER in the placebo group. Administration of BTX-A into the neck and shoulder muscles for treatment of chronic refractory neck pain met only 1 of the 2 primary outcomes (reduction in pain intensity).
BTX for low back pain
The use of BTX in the management of chronic low back pain remains controversial but has been investigated. In a randomized, controlled study involving 31 patients with chronic low back pain, Foster and colleagues studied the effect of 200 U of BTX-A (5 sites in the paravertebral levels L1-L5 or L2-S1, 40 U per site) compared with placebo injections. [68] Pain and extent of disability were noted at baseline and at 3 and 8 weeks using a VAS and the Oswestry Low Back Pain and Disability Questionnaire. At both 3 and 8 weeks, more patients who had received BTX injections (73.3% and 60%, respectively) experienced 50% or more pain relief compared with the placebo treated group (25% and 12.5%, respectively). At 8 weeks, less disability was noted in the BTX-treated group compared with the placebo-treated group.
Knusel and colleagues treated patients with low back pain associated and painful muscle spasm with different doses of BTXA and noted that only those treated with the highest doses (240 U) experienced significantly greater relief than placebo-treated patients. [69]
Two randomized, prospective studies, one double-blind and one open label, were performed to evaluate the long-term efficacy and safety of BTX-A in 31 and 75 patients with chronic low back pain, respectively. Both studies used a novel injection technique, with placement of 40-50 U of BTX-A by injection into the erector spinae muscles at each of 5 levels from L1-L5. [70] Jabbari reported significant (p < 0.05) reduction of pain intensity and improvement in performance of activities of daily living in 60% and 53% of the patients, respectively. A second study also demonstrated safety with repeated injection sessions over 14 months. The author suggests that BTX-A should be considered when treatment of low back pain fails other more standard management approaches.
A prospective study by Jabbari et al was also performed to study the short-term and long-term effects of BTX-A on refractory chronic low back pain. [71] Seventy-five patients received BTX-A injections into paraspinal muscles at 4-5 levels between L1-S1 unilaterally or bilaterally. Dose per site ranged from 40-50 U, whereas the total dose per session ranged from 200-500 U. Reinjection of BTX-A was performed at 4 months if pain returned over the study duration of 14 months. Outcome data collection included VAS scores, pain frequency (eg, number of pain days), and self-perceived functional status using the Oswestry Disability Questionnaire (ODQ).
Participants were assessed at baseline, 3 weeks, and then at 2, 4, 6, 8, 10, 12, and 14 months. Forty patients at 3 weeks (53%) and 39 patients at 2 months (52%) reported significant pain relief. Changes in VAS, ODQ scores, and pain frequency were consistent with patient improvements and were statistically significant when the 2-month data were compared with baseline at 2 months and then after each injection period (p < 0.005). Among initial responders, 91% continued to show improvement over the length of the study. Three patients (4%) experienced a probable adverse event consisting of a mild flulike reaction that lasted 2-5 days following an initial injection session. The number of responders and durations of chronicity is unclear. Any associated therapies were not noted. Therefore, agreeing with the authors when they suggest that a favorable initial response to BTX-A predicts subsequent responsiveness is difficult.
The same authors performed an open label prospective study on 60 patients with chronic low back pain. [72] Patients received 40-50 U per paraspinal level with multiple levels injected. A maximum dose was 500 units of BTX-A per an injection session. Study participants with a beneficial clinical response received a second treatment at 4 months. Pain and clinical status were assessed by VAS, modified OLBPQ, and a CLBPQ at baseline, 3 weeks, 2 months, 4 months, and 6 months after the first treatment. Participants included 18 women and 42 men, aged 21-79 years (mean, 46.6 y), with chronic low back pain over a mean duration of 9.1 years.
Significant improvement in back and radicular pain occurred at 3 weeks in 60% and at 2 months in 58% of the cohort. Again, the authors found that a beneficial clinical response to the first injection predicted the benefit of a second reinjection response, which was indeed measured determined to be 94%. A significant minority of patients had a sustained beneficial effect from the first injection at 4 months (16.6%) and 6 months (8.3%). Two patients experienced an adverse event described as a transient flulike reaction after the initial treatment. Ney et al concluded that BTX-A is a reasonable therapy for seeking improvement in patients with refractory chronic low back pain.
A beneficial clinical response can be predicted within the first 2 months following treatment. An early positive response from BTX-A treatment also predicts the high likelihood that the benefit is sustained with a second treatment. Furthermore, BTX-A demonstrates a low incidence of mild and transient side effects.
BTX in the management of neuropathic pain
BTX is effective in the management of neuropathic pain, which is caused by damage or dysfunction within the central or peripheral nervous system. Conditions such as postherpetic neuralgia (PHN), spinal radiculopathy, complex regional pain syndrome (CRPS), spinal cord injury, and brachial plexus injury are examples of neuropathic pain syndromes. [73] BTX-A has demonstrated relief of pain in conditions associated with muscular overactivity, but may also be effective in the treatment of neuropathic pain. Multiple neurochemical and neurophysiological mechanisms have been cited that could explain potential actions of BTX-A as a therapeutic agent for neuropathic pain.
Freund and Schwartz reported reduced pain in 7 patients with trigeminal, thoracic, or lumbar PHN of more than 6 months who were treated with subdermal BTX-A injections at a concentration of 5 U per 0.1 cc preservative-free normal saline into every 9 cm3. [74] In another report, 2 patients with cervical spinal cord lesions experienced hyperesthesia, allodynia and burning pain in a segmental dermatomal distribution. [75] Patients were treated with multiple point subcutaneous injections of BTX-A in the involved dermatome. Definite analgesia was obtained and then maintained by repeating injection treatments every 4-6 months. Injections in one patient were discontinued at 3 years and in the second patient after 2 years, when neuropathic pain symptoms subsided.
A series of 3 case reports included treatment of chronic refractory neuropathic pain in 2 patients with PHN and another with an S1 radiculopathy. [73]
A physician with PHN of the left V-1 region was treated with BTX-A and rapidly experienced complete pain relief except for an area of pruritus with intermittent paroxysmal pains in the medial canthus area. This area was reinjected with 5 U of BTX-A, and paroxysmal pain resolved. At 2 years and over 5 years following his initial injection session, the patient reported occasional mild pruritus in the left V1 area when "overheated or stressed."
The second patient had right lateral foot pain and allodynia in an S1 pattern due to PHN. He chose to try BTX-A following multiple oral and topical medication therapies. The patient received incomplete relief in the anterior two-thirds of the affected area, but minimal relief in the posterior third of the affected area despite reinjection. At 4 months follow-up pain recurred, and he chose not to repeat BTX-A treatment.
The third case was a male attorney with an 8-year history of right S1 radicular burning, with pain and allodynia affecting the right lateral foot. Extensive diagnostic workup was negative and pharmacological/nonpharmacological therapies were ineffective. Selective nerve root blocks demonstrated a painful S1 radiculopathy without any structural cause amenable to surgical therapy. Subsequently, BTX-A injections caused complete resolution of S1 burning pain and allodynia, which had continued beyond 18 months and now beyond 10 years follow-up.
Injection techniques for these patients were similarly from a technical standpoint to those with hyperhidrosis. The affected sensory area was outlined, then divided into grids between 1.25 – 1.50 cm squares or diameter circles. BTX-A dosage and dilution was determined by the thickness and resistance of the skin region to be injected and grid-size.
Long-lasting analgesia of neuropathic pain was demonstrated in 2 experimental studies using rats with either alloxan or streptozotocin-induced diabetic peripheral neuropathy. A single subcutaneous injection of BTX-A produced a prolonged antinociceptive effect as measured by mechanical sensitivity/ [76, 77]
An abstract by Relja and Militec presents a prospective study of BTX-A treatment of painful diabetic neuropathy, whereby 41 symptomatic patients were randomized into a BTX-A 100 U treatment or placebo group. [78] Injection methodology was not discussed in the published abstract. All patients completed the study. Significant improvements were noted in all outcome measures, including the endpoint mean pain score, VAS, global assessments, and the SF–36 Questionnaire.
BTX for osteoarticular pain
The rationale for the use of BTX injections into painful joints followed research findings that implicated intra-articular injections of substance P and calcitonin gene-related peptide (CGRP) as causative of joint pain and inflammation. BTX was found to produce significant pain relief when injected into painful joints due to either inflammatory or noninflammatory disorders. This rationale presumes that the neurotoxin is capable of binding to nocicepter C-fibers, undergoing endocytosis, and blocking the vesicular release of substance P, CGRP, and glutamate, which are all pain mediators capable of producing neural transmission of noxious stimuli with subsequent nocicepter sensitization.
Mahowald et al reviewed their clinical experience with 11 patients (15 joints) who were treated for refractory joint pain with intra-articular injections of BTX-A over 12 months. [79] None were considered to be surgical candidates, and all had failed multiple oral and intra-articular medication treatments. Fifteen joints were managed by intra-articular injections of BTX-A. Six lower extremity joints (3 knees, 3 ankles) received 25-50 U, and 9 shoulders were treated with 50-100 U. Maximum relief of pain, maximum improvement in function, and the time to perform sit-to-stand 10 times (the timed stands test [TST]) were used as outcome measures for the lower extremity joints.
Five patients had osteoarthritis (OA), 5 had rheumatoid arthritis (RA), and 1 had psoriatic arthritis. A clinically and statistically significant improvement was noted after IA-BTX-A injections. The mean maximum decrease in lower extremity joint pain was 55%, and a 36% improvement in the TST was noted at 4-10 weeks after injection. A 71 % mean maximum reduction in shoulder pain severity was noted. Active range of motion increased 67% in flexion and 42% in abduction. No significant adverse effects related to BTX-A were noted. Duration of pain relief ranged from 3-12 months. Although this study was small and uncontrolled, the results suggest that IA-BTX-A injections are an effective and safe treatment for chronic joint pain.
Singh et al performed a randomized, double-blind, randomized controlled trial to determine the safety and efficacy of intra-articular BTX-A injections in 43 patients with chronic refractory, moderate-to-severe shoulder joint pain presumed to be due to arthritis. [80] Patients were randomized to receive either 100 U of BTX-A with lidocaine or saline and lidocaine. Primary outcomes were reduced pain severity on VAS at 1 month (0-10 cm). Secondary outcomes were improvements as measured by the Shoulder Pain and Disability Index (SPADI) disability subscale, quality of life on short-form (SF)-36 subscales, percent of patients who achieved at least a 30% decrease or a 2-point reduction in VAS pain (clinically meaningful pain relief), and safety.
Both BTX-A (n = 21) and placebo (n = 22) groups were comparable at baseline. At one month postinjection, pain reduction by VAS, SF-36 subscale scores, and the SPADI disability subscale improvement were significantly greater in the BTX-A group than in the placebo group. Clinically meaningful pain relief occurred in 61% of the BTX-A treatment group versus 36% of placebo patients (P = 0.22). The total number of adverse events was similar, which included 50 events in the BTX-A group versus 46 events in the placebo group. Therefore, a single injection of BTX-A produced statistically significant and clinically meaningful pain relief and improvement in quality of life in patients with chronic refractory moderate/severe shoulder arthritis pain at 1 month. These data provided evidence to support the need for a larger multicenter, randomized trial.
The effect of BTX-A on pain and functional impairment caused by refractory plantar fasciitis was investigated using a randomized, double-blind, placebo-controlled study of 27 patients (43 feet) with plantar fasciitis. [81] In patients with comparable bilateral severity, BTX-A was injected in one foot and saline in the other. BTX-A at 70 U was divided into 2 sites per foot. Placebo was the same volume of normal saline. Main outcome measures included pain VAS, Maryland Foot Score, pain relief VAS, and pressure algometry response. Patients were assessed at baseline, 3 weeks, and 8 weeks. Compared with placebo injections, the BTX-A group improved in all measures.
BTX for shoulder pain following stroke
BTX has been studied for use in shoulder pain following stroke. A small, double-blind, 2-parallel group, randomized controlled trial showed a beneficial effect on shoulder pain following injection of BTX-A into the subscapularis muscle in patients who had experienced a stroke and who had spastic hemiplegia. [82]
To assess the effects of BTX-A on hemiplegic shoulder pain associated with spasticity, a double-blind, randomized controlled trial looked at a one-time injection of BTX-A (500 Speywood U) into the pectoralis major and biceps brachii on the hemiplegic side. [83] VAS of shoulder pain, shoulder adductor and elbow flexor tone using the Ashworth scale, and passive range of shoulder abduction were assessed as outcomes. Only 17 patients were enrolled, 8 in the BTX-A group and 9 in the placebo group. Negative findings in this study include the small sample size and the presence of causes of shoulder pain not related to spasticity, which could have confounded outcome.
A double-blind, randomized controlled trial was performed to determine the efficacy of BTX-A for treatment of shoulder pain in patients with spasticity after stroke. [84] Two cases dropped out (6.5%) of 31 patients enrolled from an acute-care hospital in Spain. Fourteen subjects were treated with infiltration of 500 U of BTX-A compared with 15 who received placebo in the pectoralis major muscle of the paretic side. Patients were assessed using a VAS for pain. A significant reduction in pain was considered when the VAS score was below 33.3 mm or less than half the initial score. At 6 months, patients treated with BTX-A showed significantly greater improvement in pain than placebo from the first week postinfiltration. Patients with shoulder pain from spasticity treated with BTX-A infiltration into the pectoralis major muscle on the paretic side had a higher likelihood of pain relief, ranging between 2.43-3.11-fold.
A randomized, double-blind, placebo-controlled study of the effect of BTX-A injections into the subscapular muscle was performed in 22 stroke patients with spastic hemiplegia, substantial shoulder pain, and reduced external rotation of the humerus. [85] Twenty-one of twenty-two patients completed the study. No significant changes in pain or external rotation were noted as a result of BTX-A administration. Therefore, application of BTX-A into the subscapular muscle for reduction of shoulder pain and improvement of humeral external rotation in spastic hemiplegia did not appear to be clinically efficacious.
A prospective, double-blind, randomized controlled trial was conducted to compare the effects of BTX-A and triamcinolone acetonide (TA) on shoulder pain and arm function in 29 patients who had experienced hemiplegic stroke with pain duration of 24 months or less and numeric rating scale of 6 out of 10 or more. [86] Patients were randomized into 2 groups: a group that received intramuscular injections of BTX-A 100 U (total) during one session to the infraspinatus, pectoralis, and subscapularis muscles in conjunction with intra-articular injections of NS into the painful joint and a comparison group that received an intra-articular injection of TA (40 mg) and an intramuscular injection of NS to the same muscles. Results from this study suggest that injection of BTX-A into selected muscles of the shoulder girdle might provide more pain relief and range of motion improvement than intra-articular TA in patients with hemiplegic shoulder pain.
A Cochrane systematic review was performed to determine the efficacy and safety of BTX compared with placebo or other treatment options for shoulder pain. [87] Using well-known standard search strategies, 6 randomized controlled trials comparing BTX with placebo or active treatment in 164 patients with shoulder pain were evaluated. Participants in 5 of the trials with poststroke shoulder pain received a single intramuscular injection of BTX that significantly reduced pain at 3-6 months postinjection when compared with placebo; shoulder external rotation was increased following one month, but not at 3-6 months.
Shoulder abduction, external rotation and spasticity did not differ between groups, nor did the number of adverse events. Only one trial with arthritis-related shoulder pain showed that BTX reduced shoulder pain severity and disability with a reduction in the Shoulder Pain and Disability Index score compared with placebo. The authors suggest that the results of their review should be interpreted with caution due to the small number of studies, small sample sizes, and the outcome targeted ranges of motion when compared with placebo in patients with shoulder pain due to spastic hemiplegia or arthritis. Pain relief in poststroke study patients primarily relates to study limitations and interpretation, rather than to any research-proven clinical phenomenon.
BTX for muscle spasticity
BTX-A has been demonstrated to reduce pain in muscle spasticity and has been applied to treat more common painful disorders such as headache, neck pain, and back pain. The beneficial effect attributed to BTX is thought to be due to in part to its capacity to reduce painful muscle contraction or spasm; therefore, research continues determine whether it can be used as an effective intervention for myofascial pain disorders, which has been studied extensively, but remains controversial and poorly understood.
Wissel et al investigated the effects of BTXA injections in 60 patients with pain due to acute and chronic spasticity in a prospective multicenter study. [88] Baseline and follow-up (mean 5.9 wk) measures included a patient self-assessment of pain and function using a 5-level scale, a physician evaluation of function, and a global rating of response. Fifty-four of sixty patients experienced improvement in pain without subjective functional improvement. The effects were comparable in acute (n = 17) and chronic (n = 43) spasticity. No serious adverse event was observed.
BTX for urological pain
Zermann et al reported pain relief in 11 patients with chronic prostatic pain who were treated with BTX-A (200 U) by transurethral perisphinteric injection. [89]
Giannantoni et al looked prospectively at the 2-year efficacy and tolerability of intravesical BTX-A injections in patients with painful bladder syndrome (PBS) associated with increased urinary frequency refractory to conventional treatments. [90] Preliminary assessment of the 13 participants, who were all women, included voiding diary, urodynamics, urinary tract ultrasonography, and VAS assessment of pain intensity. All patients received multiple injections of 200 U of commercially available BTX-A diluted in 20 mL NS under cystoscopic guidance.
Clinical evaluation, urodynamic studies, urinary tract ultrasonography, and VAS assessment were repeated at least twice per year during follow-up. A total of 58 injections were administered, with a mean of 4.8 ± 0.8 injections per patient. The mean interval between 2 consecutive injections was 5.25 ± 0.75 months. At 1-month and 4-month follow-ups, 10 patients reported subjective improvement. Three nonresponders to initial BTX-A intravesical treatment underwent a repeat session 3 months later with satisfactory response.
At the 1 year and 2 year follow-ups, the beneficial effect from intravesical BTX-A persisted in all patients. The authors did not observe any adverse systemic side effects during the study period. They concluded that intravesical injections of BT-XA are effective and safe, at least for medium-term management of patients with PBS. As the beneficial BTX effect gradually decreased over several months after previous treatment sessions, repeat injections of the neurotoxin were provided when needed over time.
Liu et al reported their observations regarding the level of nerve growth factor (NGF) mRNA in bladder tissue and the effect of BTX-A treatment in patients with interstitial cystitis (IC). [91] Nineteen patients with IC underwent intravesical injections of 100 U or 200 U of BTX-A, followed by cystoscopic hydrodistension 2 weeks later. The bladder mucosa was biopsied before BTX-A injections and immediately after hydrodistension in study participants and in 12 control subjects. The NGF mRNA and protein levels in bladder tissues were assessed by real-time polymerase chain reaction and immunohistochemistry studies to determine differences in NGF expression between patients with IC before and after BTX-A treatment and compared with controls.
At 3 months, 14 patients had symptomatic improvement (responders) and 5 did not (nonresponders). At baseline, the NGF mRNA levels in the overall IC patient group were significantly greater than controls. At 2 weeks after BT-XA treatment, the NGF mRNA levels were found to be decreased and were not significantly different from the NGF mRNA levels in controls. The NGF mRNA levels decreased significantly in responders and were significantly decreased after BTX-A in 11 patients who reported a reduction in pain of 2 or more as measured by VAS.
Immunoreactivity studies of bladder tissue from patients with IC showed greater NGF density at baseline compared with controls, but the difference was no longer significant after successful BTX-A treatment. The authors suggest that intravesical BTX-A injections plus hydrodistension reduce bladder pain in patients with IC. The NGF levels in bladder tissues were significantly increased in patients with IC and dropped to normal levels after treatment in responders.
The use of ureteral stents for ureteral obstruction and after ureteroscopy can result in substantially reduced patient quality of life due to pain, frequency and urgency. Gupta et al tested their theory that numerous stent-related symptoms may be caused by detrusor muscle spasm in and around the intramural ureter by evaluating the effect of BTX-A in patients with indwelling stents after ureteroscopy. [92] Fifty-one patients were enrolled in a prospective, randomized, single-blind study comparing BTX-A injections into 3 locations around the ureteral orifice (30 patients) compared with no injection after unilateral ureteral stent insertion (21 patients).
Pain and urinary symptoms after stent placement were evaluated using the Ureteral Stent Symptom Questionnaire, which was completed on postoperative day 7. In addition, patients were required to maintain a log of opioid analgesic use between stent placement and its removal. No complications or adverse events occurred during this study. A significant reduction was reported in the postoperative pain score between the patients treated with BTX-A and the control group (eg, 3.4 vs 6 [p = 0.02]). Postoperative opioid use was less in the BTX-A treatment group, who averaged 7.7 pills over 2.7 days compared with 24.7 pills averaged over 7 days in control patients (p = 0.03).
With respect to postoperative lower urinary tract symptoms, no significant difference was noted between cohorts using the individual index scores within the Ureteral Stent Symptom Questionnaire. Periureteral BTX-A injections appear to improve ureteral stent tolerability as referenced by patient report of reduced postoperative pain intensity and decreased opioid intake over a shorter period of time following stent placement.
BTX for pain associated with rectal disorders
Other miscellaneous painful disorders have responded to BTX-A treatment as evidenced by a randomized, controlled study that suggests BTX-A can be effective in reducing pain after hemorrhoidectomy. [93] . Another published review suggests that BTX may be effective in the management of severe anorectal pain. [94]
The maximum resting pressure in the anal canal is markedly increased after hemorrhoidectomy, most likely due to postoperative pain, which is the most difficult early management problem after hemorrhoidectomy.
Patti et al compared the effects of intrasphincter BTX-A injections with application of glyceryl trinitrate ointment after hemorrhoidectomy for improving wound healing and reducing postoperative pain at rest or during defecation. [95] Thirty patients with hemorrhoids were randomized into 2 groups. One group received an injection containing 20 U of BTX-A, whereas the other group received application of 300 mg of 0.2% glyceryl trinitrate ointment 3 times daily for 30 days. Anorectal manometry was performed preoperatively and then at 5 days and 40 days following hemorrhoidectomy.
Five days after hemorrhoidectomy, maximum resting pressure was significantly reduced compared with baseline values in both groups; however, postoperative pain at rest showed a significant reduction in the BTX-A group compared with the glyceryl trinitrate group; pain during defecation and time of healing were similar. Adverse effects, such as headaches, were observed only in the glyceryl trinitrate group. At 40 days posthemorrhoidectomy, the maximum resting pressure values in the glyceryl trinitrate group were similar to those obtained preoperatively. However, the maximum resting pressure values remained decreased in the BT-XA group. These findings support the application of a single intrasphincter injection of BTX-A for more effective reduction of early postoperative pain at rest, although not necessarily during defecation. BTX-A is safer and has less side effects than repeated applications of glyceryl trinitrate.
However, Singh et al looked at 32 patients undergoing haemorrhoidectomy in a prospective randomized controlled trial. [96] Routine postoperative care included metronidazole and bupivacaine. Patients were also randomized and given an intersphincteric injection of either placebo or BTX-A (150 U). A linear analogue score (VAS) was used to assess postoperative pain. The primary endpoint was reduction in postoperative pain. No significant effect on overall or maximal pain scores was noted. Median time for return to normal activities did not differ significantly between groups. BTX-A reduced anal spasm but failed to demonstrate any significant effect on postoperative pain.
Thrombosed external hemorrhoids are a frequent anorectal emergency. They are associated with swelling and intense pain. Patti et al randomized 30 patients with thrombosed external hemorrhoids who refused surgical operation into 2 groups. [97] Patients received an intrasphincteric injection of either 0.6 mL saline or 0.6 mL of a solution containing 30 U of BTX-A. Anorectal manometry was performed before treatment and 5 days afterwards. After 5 days of treatment, the maximum resting pressure fell in both groups but was significantly lower in the BTX group (P = 0.004). Pain intensity was significantly reduced within 24 hours of BTX-A treatment (P < 0.001) but only after 1 week in the placebo group (P = 0.019). A single injection of BTX into the anal sphincter seems to be effective in rapidly controlling the pain associated with thrombosed external hemorrhoids and could represent an effective conservative treatment for this condition.
BTX for pelvic pain
Chronic pelvic pain occurs in about 15% of women and has various causes that require accurate diagnosis and appropriate treatment if pain reduction is to be effected. Superficial conditions such as provoked vestibulodynia and deeper pelvic issues such as pelvic floor myalgia were traditionally difficult to diagnose and adequately treat. [98]
To determine whether BTX-A is more effective than placebo for reducing pain and pelvic floor pressure in women with chronic pelvic pain and pelvic floor muscle spasm, Abbott et al enrolled 60 women with chronic pelvic pain lasting 2 years or longer who demonstrated evidence of pelvic floor muscle spasm. [99] The methodology was a double-blind, randomized controlled trial, wherein 30 women received 80 U of BTX-A by injection into the pelvic floor muscles, and 30 women received injections of NS. The severity of dysmenorrhea, dyspareunia, dyschezia, and nonmenstrual pelvic pain were assessed by VAS at baseline and then monthly for 6 months. Pelvic floor pressures were measured by vaginal manometry.
A significant change from baseline in the BTX-A group was noted for dyspareunia and nonmenstrual pelvic pain. In the placebo group, only dyspareunia was significantly reduced from baseline. A significant reduction in pelvic floor pressure (cm of H2 0) was noted in the BTX-A group from baseline; the placebo group also had lower pelvic floor muscle pressures. The authors found an objective reduction of pelvic floor muscle spasm, which reduces some types of pelvic pain. BTX-A reduced pressure in the pelvic floor muscles more than placebo; therefore, BTX-A may be a useful agent in women with pelvic floor muscle spasm and chronic pelvic pain who do not respond to conservative treatment, including physical therapy.
Abbott has studied and reviewed the gynecological use of BTX for the treatment of chronic pelvic pain in women. [100] In a review, he advocated the use of BTX for inflammatory conditions and in areas where muscle spasm is thought to contribute to pain. He acknowledged the limited data that support or specify the use of BTX for gynecological indications. Support for use in the vulva consists of case reports and small series, which indicate that BTX-A, when used in the vulva, may provide benefit for 3-6 months after injection of 20-40 U of BTX-A for women with provoked vestibulodynia. Retreatment is reportedly successful, and side effects are limited. Controlled studies are essential to further explore this indication.
For pelvic floor muscle spasm, a greater number of women have been studied and a double-blind, randomized controlled study reported a significant reduction in pelvic floor pressures, with significant pain reduction for some types of pelvic pain compared with baseline. No differences in pain were noted when compared with the control group who had physical therapy as an intervention. Physical therapy can be used as a first line treatment or adjunctively with BTX-A injections in cases of refractory pain and muscle spasm.
In a review by Rao and Abbott, they cited pain symptoms caused by pelvic floor muscle spasm, daily pelvic pain, and dyspareunia are the most likely to be improved by BTX-A. [101] Limited data supporting the use of BTX for provoked vestibulodynia indicate an improvement in pain scores. In the lower GI tract, BTX injection into puborectalis has demonstrated objective improvement in intravaginal pressures, although no randomized controlled trials (class I studies) have validated its use in this setting. Class I studies demonstrate a role for BTX-A in the management of idiopathic detrusor overactivity, although long-term follow-up data are lacking.
Potential problems with BTX-A use include reactions to the toxin and urinary and fecal incontinence. A single class I study supports the use of BTX-A for refractory pelvic floor spasm; however, further adequately powered class I studies for this indication and for provoked vestibulodynia are warranted.
For pelvic floor myalgia, 1 class-I study and 3 class-II to -III studies have indicated efficacy of BTX-A. In the only double-blind, randomized controlled trial, significant reduction in pelvic floor pressures with significant pain reduction for some types of pelvic pain were reported compared with baseline. No differences in pain occurred compared with the control group who had physical therapy as an intervention. Physical therapy should be used as first-line treatment and then adjunctively with BTX-A injections for those who remain refractory to treatment.
BTX in other miscellaneous pain disorders
Neck dissection surgery and radiation therapy for the treatment of carcinoma of the head and neck often results in chronic pain. Four of 6 volunteers with muscular neck pain and spasm after radiotherapy for treatment of carcinoma of the head and neck who received BTX-A injections into affected sternocleidomastoid muscle in 1 or 2 locations achieved pain relief. [102]
A prospective, open-label study of 16 patients with chronic neck pain after dissection received 80-320 U of BTX-A (Dysport) injected into muscular trigger points. Outcome measures included chronic and shooting pain using VAS and quality of life improvement measures before and 4 weeks after treatment. All patients showed a significant reduction in chronic pain (4.5 before to 3.3 after treatment, p =.005) and shooting pain (6.1 before to 4.7 after treatment, p =.005), including a trend toward improvement in measures of global quality of life and function. [103]
In another study, 23 patients with chronic neuropathic pain after neck dissection were selected for an open, prospective phase II trial. [104] One group of patients received BTX-A SC in a low-dose concentration of 10 U/0.1 mL saline (n=13) compared with a high-dose-group (n=10) of 20 U/0.1 mL saline. Pain and quality of life measures were assessed at day 0 and day 28. The low-dose BTX-A group showed significant pain reduction by VAS of 4.3 at day 0 to 3 at day 28 (P< .05); however, the mean pain VAS values did not significantly improve in the high-dose group. Trends toward improvement in quality of life were only in the low-dose BTX-A group.
BTX for the treatment of primary headache disorders
In 2004, the International Headache Society (IHS) published the second edition of the International Classification of Headache Disorders (ICHD), which divides headaches into primary and secondary disorders. Primary headache disorders are defined as those which occur as the result of a primary neurological process, whereas secondary headaches are attributed to an identifiable underlying cause or condition of the nervous system. Primary headache disorders include migraine, tension-type headaches and cluster headaches, among others.
Migraine is defined as a headache with at least moderate intensity that is frequently unilateral, throbbing, and usually accompanied by nausea, photophobia and phonophobia. Tension-type headache is characterized as a bandlike tightness without migraine-associated symptoms. In 1994, a revision of the established IHS criteria was proposed using the eponym "chronic daily headache" to describe a condition that occurs 15 or more days per month, with an average untreated duration of more than 4 h/h. [105]
BTX is an appropriate consideration for treatment of refractory headache, especially chronic daily headache, when standard pharmacology is ineffective or fraught by adverse side effects. BTXs are an enticing alternative to many standard preventive medications that interfere with alertness or cognitive efficiency in people who provide complex intellectual services or operate industrial equipment, including aircraft or other vehicular machinery. Therapeutic benefits may occur due to elimination of localized myalgia, muscular triggers, or painful muscle tension that accompany a headache; however, the aforementioned theorized CNS antinociceptive effects may be more salient. [73]
Dr. William Binder, a plastic surgeon, serendipitously observed that many of his patients who had undergone BTX-A injections for the treatment of cosmetically undesirable hyperfunctional facial lines reported improvement in their headaches with reduced frequency and duration that paralleled its adverse effect on experimentally discovered neural mechanisms.
As a result of this observation, he coordinated a multicenter, open-label trial of BTX-A in patients with migraine. [106] Thirty-six of seventy-seven patients (51%) with IHS-defined migraine noted complete relief of their headaches, with a mean duration effect of 4.1 months. Twenty-seven of seventy-seven patients (38%) reported a partial response. The site of injections varied from patient to patient, but most often included the frontalis, temporalis, corrugator, procerus muscles, and, in a few patients, the suboccipital muscles. The dose of BTX-A also varied between patients. Eyebrow ptosis was the only significant adverse effect experienced by some of the study participants.
Silberstein and colleagues reported the results of a multicenter, randomized, controlled study of BTXA involving 123 patients with IHS-defined migraine who experienced 2-8 severe migraine headaches each month. [107] Patients were randomized to 1 of 3 groups: placebo and 25 or 75 U of BTX-A. Eleven standard injection sites were used, including bilateral frontalis, temporalis, corrugator, and the procerus muscles. Compared with placebo, the patients receiving 25 U of BTX-A experienced significantly fewer and less severe migraine headaches, reduced acute headache medication usage, and decreased emesis. These differences were not significant when comparing the groups receiving 75 U of BTX-A versus those receiving placebo. Adverse events included 2 cases of diplopia and 13 cases of ptosis.
In a separate randomized, placebo-controlled, multicenter study, Brin and colleagues studied the efficacy of BTX-A for migraine prophylaxis. [108] Patients received BTX-A injections in the frontal and temporal regions, BTX-A frontal injections with placebo-temporal region injections, BTX-A temporal region injections with placebo-frontal injections, or placebo-frontal and temporal region injections. Only patients who received BTX-A injections into both temporal and frontal regions experienced significantly greater headache relief than the placebo-only group.
More recently, several important studies were reported as abstracts and cited interesting and potentially pertinent observations. In one study, 30 patients who were experiencing between 2-8 IHS-defined migraine attacks each month, were randomized to receive either 50 U of BTX-A or placebo injections. Fifteen injection sites were used, including the temporalis, frontalis, corrugator, procerus, trapezius, and splenius capitis muscles bilaterally. [109] Patient responses were followed for 90 days. Compared with placebo-treated patients, who did not experience any significant change in their headache frequency or severity, those who received BTX-A injections had a significant reduction in headache frequency and severity (at 90 d, 2.5 vs. 5.8; p< .01). No significant adverse effects were noted.
In an open-label study evaluating the effects of BTX-A on patients with episodic and chronic migraine, treatment with 25 U of BTX-A (frontalis, temporalis, and corrugator muscles) demonstrated decreased migraine-associated disability in 58% of patients. [110] Two retrospective studies have emphasized the potential benefit of BTX-A as a "disease modifying" treatment for chronic migraine. [111, 112]
One open-label study involving the use of BTX-B for the treatment of chronic migraine was reported. Forty-seven patients with at least 4 migraine headaches within a 4-week period were treated with a total of 5000 U of BTX-B placed into at least 3 sites. [49] Injection sites were chosen on the basis of pain distribution and included trigger points and glabellar lines. Thirty patients (64%) reported diminished headache intensity and severity. One adverse effect unique to BTX-B versus-A treatment was dry mouth.
Several reports suggest that benefit increases from repeated treatments with BTX-A in patients with chronic migraine. Although not strictly derived from randomized and controlled studies, many injectors consider that these clinical observations are important to consider if the maximal benefit is to be realized from BTX injections. Other retrospective reviews found support for a beneficial role using BTX-A as a prophylactic treatment for migraine. [113, 114, 112, 115, 116] However, these studies were limited by faulty methodology, low numbers of study patients, poorly defined end points, and heterogeneous patient populations, often including other IHS-described types of chronic daily headache. [117]
However, evidence of benefit from BTX was not as clearly demonstrated in 3 double-blind, randomized, placebo-controlled studies. Relja et al randomized patients with episodic migraine occurring between 3-15 days per month after a single-blind, 30-day, placebo run-in. [118] Patients were randomized within placebo responder or nonresponder strata into placebo and 3 BTX-A treatment groups of 225 U, 150 U, or 75 U. A fixed-site, fixed-dose injection methodology was used for 3 treatment sessions at 90-day intervals. The primary efficacy measure was a mean change from baseline of episodic migraine frequency between day 150 and day 180 in the placebo nonresponder strata.
Four hundred and ninety-five patients (322 placebo nonresponders) were randomized into 1 of the 3 BTX-A treatment groups or placebo. All placebo and BTX-A treated groups showed substantial reductions in episodic migraine frequency; however, no statistically significant differences were seen among treatment groups. Results may have been confounded by study participants who overused acute rescue and abortive medications.
Saper et al performed a randomized, double-blind, placebo-controlled study of 232 patients with 4-8 moderate to severe episodic migraine headaches per month. [119] Patients were randomized into placebo or 1 of 4 BTX-A treatment groups. Three BTX-A groups consisted of patients receiving a single injection in the frontal, temporal, or glabellar regions; a fourth group received therapeutic injections into all 3 areas. For 3 months following a single injection session, patients recorded pertinent evaluation variables and periodically completed quality of life questionnaires. All BTX-A groups and the placebo group showed a comparable reduction in the frequency of episodic migraine from baseline, but no significant between-group differences were observed for any of the multiple efficacy measures for treatment. Again, study results were likely confounded by excessive patient use of concomitant prophylactic and acute headache medications.
In a third randomized, placebo-controlled study by Elkind et al, patients with 4-8 moderate to severe episodic migraines per month were randomized into placebo or into one of 3 BTX-A treatment groups receiving 7.5 U, 25 U, or 50 U. [120] Injections were placed into predetermined fixed sites in the frontal, glabellar, and temporal muscles. Patients were subjected to 3 injection cycles, 4 months apart. Patients receiving placebo or 7.5 U were then randomized into a second study to receive a masked higher dose of 25 U or 50 U. Patients in the initial 25 U and 50 U groups received 2 masked treatment sessions of their previously assigned dose. Patients completing the second study arm were next randomized into another 3 treatment groups: BTX-A 25 U, 50 U, or placebo.
In the first randomized study-arm, all groups showed a comparable reduction in frequency of episodic migraine at all time points; however, the BTX-A groups demonstrated statistically significant improvement over the placebo group for global assessment at 4 months. Improvements in all groups observed in the first study were sustained through both the second and third arms of the study. Therefore, this study failed to show a significant reduction in frequency of migraine compared with placebo, which the investigators determined was the primary reason for prescribing a prophylactic migraine therapy. However, result validity was again questioned due to excessive patient use of prophylactic and acute headache medications.
A study by Jakubowski et al explored whether specific neurological markers could be identified that might predict the benefit from BTX-A treatment. [121] Researchers used 100 U of BTX-A spread over 21 standard cranial and cervical muscular sites. A prospective study (n=27) identified BTX-A responders between 4-12 weeks after the injection session. Responders were defined as subjects who had 80% or higher reduction in the mean number of days that they experienced migraine per month (attack frequency X attack duration). Nonresponders were defined as patients who dropped 33% or below migraine days per month.
Among multiple migraine-associated symptoms, the pertinent marker was identified as patient-perceived directionality of head pain. Ninety-two percent of nonresponders characterized their headaches as a build up of pressure from inside the head, termed by the authors as "exploding," whereas 74% of responders described an "imploding headache," a perception that the head was being crushed or assaulted by external forces. All subjects were responders in a smaller third group (n=5) who reported pain as pressure localized behind the eye, hence the classification "ocular headaches."
The results from the prospective study were replicated in a retrospective analysis of 36 patients, thereby suggesting reliability. However, directionality of head pain is a subjective symptom report that would benefit from further study with a standardized and validated psychometric instrument. Any deduction that this study provides specific insight into the pathophysiology of migraine or analgesic mechanisms of BTX-A for headache is speculative at this time.
Tension-type headache as an entity was addressed by numerous published observations and studies to determine whether or not BTX treatment was a potentially effective treatment. Evolution of episodic tension headaches into a chronic pain disorder has been postulated to occur when myofascial driven peripheral nociception compels mechanisms that lead to central sensitization.
A study by Zwart et al refuted the notion that BTX might be useful as a treatment for tension headache when BTX-A induced paralysis of the temporalis muscles did not show pain reduction, thereby rejecting theories proposing that increased muscle tension was a significant or primary cause of tension-type headaches. [122] However, two subsequent small, open-label studies using BTX-A for the treatment of tension-type headaches did show reduced headache duration, pain intensity, and muscle tenderness. [118, 123]
Additional case reports and open label studies suggested that BTX-A was an effective therapy for chronic tension-type headache syndromes. [124, 125, 126, 127] Porta compared treatment responses between BTX-A and methylprednisolone injections in patients with tension-type headaches. [128] Although both groups improved, patients treated with BTX experienced improvement for a greater duration of time (>60 d) compared with the methylprednisolone group.
In a randomized, controlled study of 37 patients with tension-type headache, participants received either 100 U of BTX-A or placebo into 6 injection sites (2 in the temporalis muscles and 4 in cervical sites). [129] At 3 months postinjection, the treatment group showed a statistically significant reduction in headache severity compared with the placebo group. Similarly, 3 subsequent double-blind, placebo-controlled studies demonstrated significant benefit from BTX-A treatment of chronic tension headaches. [130, 131, 132]
Cluster headache was the subject of several reports to determine any benefit from treatment with BTX. Case reports by Ginies and Fraimount, BTXA appeared to end cluster headache periods in 3 of 5 patients. [133] Freund and Schwartz reported that BTX-A ended a cluster period in 2 patients. [134] Within 9 days of treatment, the headaches abated for both patients. In an open-label study, Robbins reported his observations of 7 patients with chronic cluster headache who were treated with BTX-A or type B. [135]
Treatment was at least moderately effective in 4 of the 7 patients and not effective in 3. He also treated 3 patients with episodic cluster headache with BTX, and 2 of the 3 patients had at least moderate improvement. A report by Smuts and Barnard cited positive responses to BTX treatment in 2 of 4 cluster headache patients. [127]
Chronic daily headache is estimated to effect 4% of the US population. [136, 137] This phenomenon was originally conceived and described as a disorder that developed in individuals with a long history of episodic migraines or tension-type headaches. [138] Transformed or chronic migraine was a concept introduced by Mathew et al to describe a clinical syndrome which evolves gradually from typical migraine events in patients who usually have onset of symptoms in their early twenties and who characteristically develop increasing frequency and reduced intensity of headaches. [115]
In contrast and by definition, chronic tension-type headache characteristically develops in patients with a history of headaches that are not associated with distinct migraine features such as nausea, photophobia, and phonophobia. Although most transformations occur slowly, sudden conversion may occur in 20% of cases, and often follows trauma, illness, or surgery. [139]
In an open-label study by Klapper and Klapper, 4 of 5 treated patients with chronic daily headache benefited from BTX-A injections. [140] In a follow-up randomized study, 56 patients with chronic daily headache were divided into 4 groups, depending on whether they received forehead and/or suboccipital BTX-A injections. Only the patients who received BTX-A injections into both regions experienced a significant benefit. Argoff reported 3 patients with chronic daily headache who were all treated successfully using a total dose of 5000 U of BTX-B injected into the frontalis, temporalis, corrugator, splenius capitis, splenius cervicis, levator scapular, and trapezius muscles. [141]
A randomized, double-blind, placebo-controlled, parallel design study looked at the use of BTX-A for treating chronic daily headache in patients who were experiencing either or both chronic migraine or tension-type headache. [142] Sixty patients satisfying criteria for this disorder were randomized to receive either placebo or 200 U of BTX-A using the "follow the pain" injection paradigm. If the patient consented, a second open-label BTX-A injection treatment was provided at 12 weeks. After the first injection session, patients treated with BTX-A had significantly fewer headache days during weeks 8-12 compared with the subjects who received just placebo. Twenty-four patients who received 2 BTX-A treatment sessions had significantly fewer headache days over the 12-week study period than those who received BTX-A injections only once.
Mathew et al performed a randomized, double-blind, placebo-controlled trial of 355 patients with chronic daily headaches due to chronic migraine or tension-type headache. [143] Again, findings showed a dramatic benefit with treated patients having an average of approximately 7 more headache-free days per month compared with baseline. In addition, a statistically significant percentage of patients in the treatment group experienced a 50% or greater reduction in the frequency of headache days. Both studies reported a small number of transient mild to moderate adverse events.
Another double-blind, placebo-controlled trial using BTX-A enrolled 702 patients. [144] The overall study duration was 11 months and included a 30-day screening period followed by a 30-day placebo run-in. Subjects determined as placebo responders and nonresponders were randomized into placebo or BTX-A treatment groups of 225 U, 150 U, or 75 U. Patients received additional masked treatments at 90 days and 180 days. Participants were assessed every 30 days for 9 months. The primary efficacy endpoint was a mean change from their baseline frequency of headache-free days at day 180 compared with the placebo nonresponder group. This primary efficacy endpoint was not met; all groups responded to treatment. However, the 225 U and 150 U groups experienced a greater reduction in headache frequency than the placebo group at day 240.
Five randomized, double-blind, placebo-controlled studies all demonstrated clinically significant reduction in the frequency of chronic recurrent migraine headaches using BTX-A. [145, 146, 147, 148, 149, 119] In some studies, BTX-A was the only prophylactic therapy. Other promising findings included reduction of acute medication use, reduced frequency of long duration headaches, and increased headache-free days.
A randomized, double-blind, placebo-controlled, exploratory study by Saper et al demonstrated that prophylactic treatment with BTX-A reduced the frequency of headaches in migraineurs with chronic daily headache who were overusing acute headache pain medications. [119] These findings may indicate that chronic migraine or BTX might be promising as a treatment for patients with medication overuse headache.
In general, several reviews aimed at the use of BTX-A for the management of headache disorders were favorable, and all reviewers suggested additional research was necessary to confirm clinical observations that have been made to date. [150, 117, 112, 151] Two reviews, using an evidence-based analysis, concluded that the evidence supporting BTX treatment for migraine was insufficient to date; nevertheless, the same authors acknowledged the probability that certain subgroups of migraine headache patients were likely shown to be responsive to BTX treatment. [151, 150]
BTX for the treatment of secondary headache disorders
BTX for the treatment of secondary headache disorders (eg, headache attributed to neck trauma) is usually characterized by pain, which emanates from the neck and shoulders to or through the occipital region of the head. Primary suboccipital pain and other pericranial structures may contribute to both tension and migraine-type headaches.
Hobson and Gladish reported benefit from BTXA treatment of cervicogenic headache from cervical whiplash injuries. [152]
Freund and Schwartz performed a double-blind placebo-controlled study of 26 patients more than 2 years postinjury with more than 6 months of musculoskeletal pain who failed conventional therapy. [126] Injection sites were selected by identifying the 5 most sensitive trigger points by palpation in the cervical region, including the splenius capitis, erectus capitis, semispinalis capitis, and trapezius muscles. Each trigger point site was injected with saline or 100 U of BTX-A.
Of the 26 patients who completed the study, the 14 patients treated with BTX-A showed significantly greater improvement from baseline using a VAS for self-assessing headache pain. They also showed improvement in cervical range of motion. No patient reported unsatisfactory or significant adverse side effects that were greater than expected following prior informed consent. Patients who experienced weakness of the shoulder girdle or neck muscles described it as minimal, acceptable, and consistent with informed consent.
A single-center, randomized, double-blind, active placebo-controlled trial of neck pain treatment for cervicogenic headache failed to show any significant differences between patients receiving physical therapy following a local anesthetic injection versus BTX-A into symptomatic trigger points. [153] However, faulty methodology and documentation was evidenced due to the authors' failure to outline the number of subjects, medication dosages, or number of sites injected. Furthermore, outcome measures were nonspecific and subjective. The information supplied in the abstract does not support any conclusion regarding the use of BTX-A for neck pain or headache.
Patients with cervical dystonia frequently report pain. Multiple studies have demonstrated that BTX is clinically effective in reducing painful muscle spasm and the abnormal head posture of cervical dystonia, as well as eliciting a dramatic reduction in the degree of pain, which is appreciated throughout the duration of the neurotoxin's expected effect.
BTX-A has also been demonstrated to reduce the pain that results from muscle spasticity. More recently BTX has been applied to treat more common painful disorders such as headache, neck pain, and back pain. The beneficial effect attributed to BTX is thought to be due to its capacity to reduce painful muscle contracture or spasm; therefore, research is underway to determine whether it can be used effectively as an intervention for MPS, which has been studied extensively throughout the literature but remains controversial and poorly understood.
Headache due to craniocervical dystonia is cited as an accepted cause of headache in the 2004 ICHD. A retrospective data analysis looked at 70 patients with craniocervical dystonia or facial (blepharospasm or oromandibular) dystonia who were treated for headaches with BTX-A. [154] Headaches with craniocervical dystonia were usually localized to the occipital (61%) or upper cervical (71%) regions. BTX-A treatment of dystonic muscles resulted in reduced craniofacial pain (eg, headache) in as many as 75% of patients. Reported adverse events were mild.
TMJDs are described as conditions that affect the temporomandibular joint (TMJ), masticatory muscles, and adjacent structures. Typical symptoms, in addition to jaw pain and TMJ dysfunction, include headache and facial pain. A BTX treatment-effect was evaluated in an open-label, prospective study of 46 patients who were predominately female and had symptomatic facial pain and TMJD due to myofascial and/or joint dysfunction for a median duration of 8 years. [155] Subjects received Botox® 50 U in each masseter and 25 U/5 sites in each temporalis muscle. Improvements in subjective and objective measures of pain and jaw function were demonstrated in most patients (87% and 96%, respectively). Investigators postulated that both peripheral neuromuscular and central neuromodulatory effects were responsible for BTX-induced pain relief.
A randomized, placebo-controlled study examining BTX-A treatment of chronic facial pain associated with masticatory hyperactivity showed a statistically significant improvement of pain in compared with placebo. [156] In contrast, Nixdorf and colleagues completed a double-blind, placebo-controlled crossover trial of BTX-A treatment of chronic moderate-to-severe orofacial pain of myogenic origin. [157] Using the same dosing paradigm as Freund and Schwartz, 25 U of BTX-A were placed into each temporalis muscle, and 50 U were injected into each masseter muscle. Crossover occurred at 16 weeks. The primary outcome variable used was the change in pain unpleasantness and intensity. No significant difference were demonstrated between placebo versus active treatment; however, only 15 patients entered the study, and only 10 patients completed it. These small participant numbers made statistical analysis difficult. Investigators postulated thatbothperipheralneuromuscularandcentralneuromodulatoryeffectswereresponsible for BTX-induced pain relief. [126]
The effect of BTX of prolonged experimental jaw clenching capable of producing pain and muscle fatigue in the human masseter muscle was evaluated. BTX was injected in 19 subjects, and isotonic saline was injected in 16 subjects. [158] Electromyographic activity at maximum voluntary contraction, pressure pain threshold before and after a 70% maximum voluntary contraction, clench sustained to pain tolerance, and the median frequency of the electromyographic power spectrum were measured.
After BTX injection, the BTX-treated group had a reduced maximum voluntary contraction lasting 3 mos and smaller decreases in pressure pain threshold from before to after the sustained clench. Also, the change in median frequency from before to after the sustained clench did not significantly differ during the postinjection sessions. However, postinjection, preclench median frequency was lower in the group injected with BTX. The authors interpret the reduced change in pressure pain threshold with BTX as a clinically modest but statistically significant analgesic effect on this model of acute muscle pain.
Occipital neuralgia can present as a paroxysmal or persistent neuropathic pain disorder. It is usually accompanied by shooting or radiating pain and paresthesiae involving the occipital and parietal regions of the scalp within the distribution of the greater and/or lesser occipital nerves. It frequently generates secondary headaches. Common causes of occipital neuralgia include irritation, injury as seen in WAD, and sometimes focal entrapment of the nerves by regional muscle spasm or MPS.
A pilot study looked at the efficacy of occipital nerve blocks for providing prolonged and significant pain relief in study participants with chronic occipital neuralgia who were treated with BTX-A reconstituted into 3 cc of NS. [159] Subjects were instructed to report their daily pain level (on a VAS), their ability to perform daily activities (on several quality of life instruments) and their daily pain medication usage (based on a self-reported log). Psychometric/outcome measures were compared between baseline prior to injection and then at 12 weeks after chemodenervation.
Pain characterized as dull/aching, or as having associated paresthesia did not show statistically significant improvement during the study. Sharp/shooting type pain showed improvement during most of the trial period. Quality of life measures specific to headache showed significant improvement by 6 weeks, which continued through week 12. General health-related and depression-related measures showed no statistical improvement. No significant reduction in pain medication usage was demonstrated.
A retrospective case series of 6 patients with severe refractory occipital neuralgia associated with severe headaches were treated with BTX-A following failure of response of multiple trials of conventional oral, injectable, and/or surgical treatments. [160] Each patient underwent bilateral occipital nerve blocks using BTX-A (50 U for each block, 100 U if bilateral). Significant reduction in pain scores as measured by a visual analog scale and improvement in the Pain Disability Index (PDI) were observed at 4 weeks in 5 of the 6 patients after receiving the BTX-A blocks. When the authors compared these same psychometrics in all 6 patients who received a injection of 0.5% bupivacaine prior to receiving BTX-A, the authors concluded that this small group of patients demonstrated a longer duration of meaningful pain relief and improved PDI scores with occipital nerve blocks using BTX-A.
Technical considerations and injection strategies for chronic migraine
In October 2010, BOTOX® was approved for the prophylaxis of headaches in adult patients with chronic migraine, defined as headaches occurring 15 or more days per month with the duration of untreated headaches lasting 4 hours or more per day. A differential diagnosis was considered as including chronic tension type headaches, new daily persistent headache, and hemicrania continua. [161]
BTX is an appropriate consideration for treatment of refractory headache, especially chronic daily headache, and when standard oral pharmacology is ineffective or fraught by adverse side effects. The transformation of migraine and tension-type headache to chronic daily headache may result from peripheral and central sensitization involving vascular and muscular tissues innervated by trigeminal and pericranial (including upper cervical) nerves.
Also, BTX prophylaxis is an enticing alternative to many standard preventive medications that interfere with alertness or cognitive efficiency in people who provide complex intellectual services or operate industrial equipment, including aircraft or other vehicular machinery. Therapeutic benefits may occur due to elimination of localized myalgia, muscular triggers, or painful muscle tension that accompany a headache; however, theorized BTX CNS antinociceptive effects may prove to be more salient.
Clinical practice and research have led to 2 basic BTX injection paradigms for headache. The "fixed-site" method targets standard craniofacial and cervical sites with a range of predetermined BTX doses. [162] This method is frequently implemented for treatment of migraine, and bilateral application is apropos, even when migraine is exclusively unilateral.
Symmetrical placement of neurotoxin reduces any tendency for the headaches to recur on the uninjected side and improves the likelihood of a favorable cosmetic outcome. The "follow the pain" approach is often used for treatment of chronic tension-type headaches, but can be used for migraine by distributing injections into areas that demonstrate tenderness or cover the headache location. Frequently, the author targets craniofacial, pericranial and cervical musculotendinous sites that act as migraine triggers or as pain generators during the headache. Palpation of these actively involved muscles may reveal spasm and tenderness. Some clinicians advocate subdermal injections or toxin placement adjacent to emerging branches of the trigeminal nerve (eg, supraorbital and supratrochlear nerves).
Therapeutic BTX dosages and injection techniques vary between individuals and between clinical disorders that affect the same muscle groups, as exemplified by hemifacial spasm, dystonia, and cosmetically undesirable hyperkinetic facial lines. The number of injection sites and total BTX dosages vary among clinicians, but should be individualized for each patient. Factors that may effect dosing include injection methodology, headache type or severity, treatment of adjacent or regional areas of involvement, and the subject's body habitus.
Standardized criteria for BTX treatment of headache have been published but are not yet established. [113, 163] Sample injection sites and dosages are outlined in the table below. Although many physicians, including the author, prefer more concentrated BTX-A solutions, such as 100 U/1-2 cc NS, many injectors advocate a higher dilution of 100 U into 2-4 cc of vehicle. [162] Many characteristic injection sites contain small, nodular, tender trigger points in distribution patterns similar to those described by Simons and Travell. [45]
Table 2. Guidelines for Headache Treatment: Botox Dosing of Specific Muscles (Open Table in a new window)
Common Injection Sites |
Botox Dose (U) |
Botox Dose(U) |
Number of Injection |
|
Muscle |
Abbreviation |
Per site |
Per muscle (each side) |
Sites per side |
Fixed site method. Characteristic injection sites. |
||||
Procerus |
P |
2.5 |
2.5-10 |
1-2 (midline vertical or horizontal relationship) |
Corrugator supercilii |
|
|
|
|
Medial |
mcs |
2.5 |
2.5 |
1 |
Lateral |
lcs |
2.5 |
2.5 |
1 |
Frontalis |
f1,f2 |
2 |
20 |
2-6 |
Temporalis |
t1,t2 |
2.5 |
30 |
4-6 |
Occipitalis |
o |
10 |
20 |
1-2 |
Follow the pain method. Common injection sites. |
||||
Splenius capitis |
c2 |
5-7.5 |
5-15 |
1-2 |
Cervical paraspinal |
c1 |
5-7.5 |
5-15 |
1-2 |
Masseter |
m |
10-50 |
10-50 |
1-2 |
Trapezius |
z1,z2 |
5-10 |
15-50 |
3-4 |
Note: Regular text denotes characteristic "fixed-site" method dosages and injection sites. Italic text denotes "follow-the-pain" location choices, doses, and number of sites. |
||||
Suggested dosing considerations for BOTOX® are as follows:
-
Currently, only BOTOX® is FDA-approved for the treatment of chronic migraine, and Allergan approves of a specific FDA-approved injection procedure that will be discussed in detail below. However, before FDA approval, injection techniques varied, and many injectors used the "follow the pain" paradigm, and dosed the neurotoxin variably, as outlined above.
-
Significant side effects are uncommon. Pain, especially in the neck; muscle weakness; and rarely flulike symptoms have been reported. Spread of the toxin with weakness involving muscles that were not directly injected, even distal from the injection sites have been noted. Anticholinergic side effects are stronger and more commonly seen with type B toxin.
-
Contraindications to treatment with BTX include pregnancy (category C); the concurrent use of any drug that adversely effects neuromuscular transmission e.g., aminoglycoside antibiotics; myasthenia gravis and Eaton-Lambert syndrome, or any disease that impairs transmission across the neuromuscular junction; or known sensitivity to the neurotoxins.
-
Treating more frequently than the recommended interval of 12 weeks may lead to the development of antibodies to the neurotoxin, which may be associated with the development of clinical resistance.
-
There is no valid or reliable method available at present for consistent and accurate conversion of a specific dose of type A toxin to a specific dose of type B toxin. Nor are their specific methods available at present for accurate conversions between commercially available type A toxins.
-
The use of BTX for pain management is part of a comprehensive treatment program that has been developed based on an accurate diagnosis.
-
Be aware of current storage and handling recommendations for each of the neurotoxins.
-
Whenever possible, use an injection technique, including needle size, that is the least likely to cause additional pain.
-
Guidance techniques such as EMG, CT, or fluoroscopy should be used at the discretion of the injector.
-
Prolonged observation following the injections is generally not necessary or warranted.
-
Follow-up should be arranged for 4-6 weeks following injections.
-
More than one series of injections, >12 weeks apart, may be required to achieve maximal analgesic response
Most advocate precise placement of neurotoxin injections into pertinent sites with minimal unwanted diffusion. Areas to avoid include the inferior-lateral frontalis where weakness may cause brow ptosis. Injections into the middle and lower face must be carefully placed and dosed to avoid asymmetry of the mouth or dysphagia. Unwanted diffusion of the neurotoxin behind the orbit causing diplopia or eyelid ptosis is best avoided by performing periorbital injections with the patient sitting, so that the head and neck are vertical.
Following craniofacial and some cervical injections, patients are instructed to remain in a vertical posture and to avoid touching or manipulating the injected areas for as long as 3 hours. Increased headache pain with muscle spasm at the injection sites can occur in about 20% of patients and is maximal during the 2-10 days following treatment. This adverse side effect is often alleviated by manual physiotherapy and/or safely-placed injections of a local anesthetic agent. Refractory symptoms of postprocedure muscle spasm with pain may benefit most from a repeat BTX session with adjunctive physiotherapy.
The desired degree of paresis induced by chemodenervation is determined by the muscle's role in headache production and its function. Most people can compensate for dense paresis of the emotive glabellar and frontalis muscles by the facility of the eyes to express feelings. Conversely, the temporalis and masseter muscles work synergistically to perform mouth closure necessary for mastication. The degree of weakness desired in these muscles is determined by the extent that they influence facial pain or headache. Therefore, BTX dosages must be calculated to maintain masticatory function with sufficient therapeutic dosing to reduce pain.
Furthermore, dosing for pain relief should produce or preserve a balance of strength between the temporalis muscle and its synergistic partner, the masseter. EMG needle guidance to assure correct needle placement into the masseter is useful, but usually unnecessary. The needle is guided into the body of the muscle, specifically into symptomatic spasm or trigger points, by grasping the painful muscle between the thumb externally to the needle insertion site on the skin and then placing the second and third fingers intraorally.
Needle depth and placement into the target area is monitored, and any penetration of the needle intraorally should be readily discovered. BTX should never be injected until the needle has reached the intended target site and the operator is confident that placement is correct. If the needle enters the oral cavity BTX injection should be aborted. The needle must be withdrawn and placed through a new site, with EMG guidance if necessary, into a site that will not allow BTX diffusion through a prior mucosal puncture site. A safer approach would entail delaying the procedure for 6-8 weeks, if the patient did not experience any adverse effects, such as hoarseness or dysphagia. BTX injected into the oral cavity, especially if swallowed, may cause a serious, potentially lethal, paresis of pharyngeal musculature.
The upper cervical and occipital muscles, especially the occipitalis, splenius capitis and cervical paraspinal muscles, may cause headache and trigger migraine. Often, these muscles contribute to pain and headache by irritation of the adjacent greater occipital nerve, causing concomitant neuropathic pain or symptoms of neuralgia. Frequently, the trapezius or symptomatic parathoracic muscles can trigger headache. Injections into this region may induce unwanted weakness of the supraspinatus and infraspinatus muscles, which form part of the rotator cuff, causing the humeral head to rise. Injection of trapezius and levator scapulae muscles may cause the acromion to shift anteriorly and sag inferiorly. This can result in a painful shoulder impingement syndrome, which usually manifests 7-10 days following BTX treatment.
Onset of a BTXA clinical effect usually occurs at 7-10 days and plateaus at 3 weeks. The neuromuscular blocking action of BTX-A lasts 3-4 months; however, the duration of reduced pain can be substantially longer, and a mitigation effect more specific for migraine may continue to develop beyond 2-3 months after the injection session. Headache improvement can be identified through the use of a diary and other self-reporting measures. Other salient measures include reduction of oral prophylactic medications, improved response from abortive therapies, as well as reduced frequency, intensity and severity of headache symptoms.
However, to conduct a large multicenter study, rules that governed injection technique and dosing were necessary to adopt to give the study a reasonable opportunity of using successful injectors, thereby providing the best chance for a successful outcome. Patients were recruited if they satisfied the definition of chronic migraine.
After written informed consent, injection sites and dosing are preplanned so that the procedure is performed efficiently. Sometimes, a patient may blame BTX therapy for a preexisting cosmetic flaw; therefore, preinjection photographs are advisable. By avoiding needle contact with the periosteum, using small volumes of concentrated injectate (1-2 cc of preservative-free normal saline per 100 U) and using a 30-gauge, 0.5-inch needle coupled with deliberate rapid injection techniques, topical anesthesia is usually unnecessary.
In heavily muscled or obese patients, a longer needle, as long as 1.5 inches, may be required to reach symptomatic muscles in the cervical-thoracic paraspinal and trapezius regions. Some injectors advocate a higher dilution of BOTOX® 100 U into 2-4 cc of vehicle. [162]
An FDA-approved treatment protocol for chronic migraine includes very precise, standardized methods for reconstitution of BOTOX® and structured injection techniques. Allergan advocates 100 U of BOTOX® diluted in 2 cc of preservative-free normal saline, which results in a concentration of 5 U/per 0.1 mL.
Reconstitution is performed using a vial of BOTOX®, which must remain upright. A 21-gauge, 2-inch needle is attached to a 5 mm syringe. Dilution of 100 unit vial of BOTOX® is accomplished using 2 mL of preservative-free 0.9% sodium chloride (saline); therefore a 200-U vial is diluted with 4 mL of preservative-free saline. Each vial contains a vacuum, which should pull the saline into the vial. Do not use a BOTOX® vial if the vacuum is absent or reduced and does not pull all the saline freely from the syringe. Leave the reconstitution needle and syringe in the bottle while gently rotating the vial to mix the BOTOX® and saline.
Next, hold the hub of the needle and remove the reconstitution syringe and replace it with a 1-mL injection syringe. Do not invert the BOTOX® vial while withdrawing the solution into the 1-mL injection syringe. Withdraw 1 mL of the reconstituted solution into the 1-mL injection syringe. Disconnect the first 1-mL injection syringe from the hub of the needle and then attach a sterile 30-gauge 0.5-inch needle to the syringe for injection. Repeat the BOTOX® withdrawal procedure with 3 additional 1-mL injection syringes and then attach 30-gauge, 0.5-inch needles per the Allergan, FDA-approved protocol. An off-label suggestion by the author is to consider attachment of 30-gauge, 1-inch needles to 2 of the syringes for use with the cervical and trapezius injections.
This BOTOX® protocol uses a fixed-site, fixed-dose injection paradigm. Prior to injection the skin over the intended and targeted injection site should be cleaned with an alcohol swab. Each injection consists of 0.1 mL of reconstituted BOTOX® (5 U). This injection protocol is characterized by fixed injection doses into specific muscle sites (eg, a fixed number and location of all injection sites with a fixed total dose of BOTOX®). Hold the needle hub with one hand so that it can be angled appropriately away from any danger and to avoid the periosteum. The bevel of the needle and the numbers on the syringe that delineate measurements on the syringe contents should face upward. The second hand controls the plunger.
The first recommended injection sites are the corrugators. The corrugator muscle injection site (MIS) is located approximately 1 fingerbreadth (approximately 1.5 cm) above the superior edge of the medial orbital ridge. Inject with the beveled needle pointing upward at a 45º angle away from the medial aspect of the muscle to avoid ptosis of the eyelid. The Allergan protocol also suggests starting on the left and moving to the right.
First the left then the right corrugator MIS are each dosed with 0.1 mL or 5 U of BOTOX®. See A in the image below.
Corrugator, procerus, frontalis, and temporalis muscles are all injected (by order of protocol) with the patient supine. Each designated muscle site is injected with 0.1 mL of BOTOX® solution. The procerus is located midline on the forehead approximately 1 fingerbreadth above and midline to the medial superior aspect of the orbital ridge of each eye. The injection site for this muscle should appear approximately midway between both corrugator injection sites. A single straight line should connect all 3 of the injection sites. The injection technique is repeated with a beveled needle upward and the needle pointing approximately 45º upward and away from the pain-sensitive periosteum. The procerus is injected with 1 mL.
See B in the image below.
Next, with the patient remaining supine, a line is drawn upward on the forehead from the medial edge of the orbital ridge about 1 fingerbreadth above each corrugator MIS. These are marked and additional sites are parallel, approximately 1 fingerbreadth lateral to the first 2 frontalis MIS . Each site is injected, first on the left and then on the right. Each of the 4 MIS receives 0.1 mL or 5 units of BOTOX® solution.
See C in the image below.
Next the temporalis muscles are dosed with 4 injections of 0.1 mL each bilaterally. The patient is asked to clinch his or her teeth, whereby the examiner is able to palpate the anterior aspect of the temporalis muscle. The first injection is performed about 2 fingerbreadths beyond this point and beneath the hairline. The second injection is performed 0.5 cm superior and approximately 1 fingerbreadth posterior to the first injection into the medial aspect of the muscle. Injection 3 should be parallel and 1.5 cm posterior to the second injection. Injection 4 should be approximately 1.5 cm below and perpendicular to the second injection into the medial aspect of the muscle.
See D in the image below.
Next, the patient is moved to a sitting posture. Occipital injection sites are identified by palpating the external occipital protuberance. The examiner continues palpation superior to the supranuchal ridge on either side of the occipital protuberance. Beginning with the left occipitalis muscle, the first injection is placed just above the occipital protuberance along the supranuchal ridge, and 1 cm leftward of the external occipital protuberance. The second injection is 1 cm lateral and 1 cm above the first injection site. The third injection is 1 cm medial and superior to the first injection site.
See E in the image below.
Next, the cervical paraspinal muscle injections are performed. The first injection into the cervical paraspinal muscles is placed about 1 cm to the left of the midline and 3-5 cm inferior to the occipital protuberance. The second injection site is 1 cm superior diagonally toward the ear from the first injection. The same injection sites are measured as mirror images on the right, leading to a total of 4, each receiving 0.1 mL or 5 units.
See F in the image below.
The trapezius muscle is a triangular shaped superficial muscle that spans from the neck to the shoulder. Visualize a proportion of the muscle from the neck to the shoulder into 3 sections per side. Injections are placed into the middle of each of these sections. The protocol recommends that the injector begin by treating the left trapezius muscle. Each of the 3 sites on the left and then on the right (totaling 6) receives 0.1 mL or 5 U of BOTOX® solution.
See G in the image below.
Following the procedure the patient is asked to remain vertical for 2-3 hours and not to rub the injected areas in any vigorous manner. The patient may return to their normal activities on the following day.
Important safety information is included in a black box warning by Allergan regarding the distant spread of toxin effects. Postmarketing reports indicate that the effects of BOTOX® and all BTX products may spread from the area of injection and produce symptoms consistent with BTX effects. These may include asthenia, generalized muscle weakness, diplopia, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence, and breathing difficulties. These symptoms have been reported hours to weeks after injection. Weakness of swallowing and breathing activities can be life threatening, and death has been reported.
The risk of symptoms is probably greatest in children treated for spasticity, but symptoms can also occur in adults treated for spasticity and other conditions, particularly in those who have underlying conditions that predispose them to these symptoms. In unapproved uses, including spasticity in children, and in some approved uses, cases of the distant spread of effect have been reported primarily at doses comparable to those used to treat cervical dystonia but also at lower doses of BOTOX®.
BOTOX® is contraindicated in the presence of infection at any proposed injection site and in individuals with a known hypersensitivity to any BTX preparation or to any of the components of the formulation. Warnings and precautions are important due to the lack interchangeability between BTX products. The potency units of BOTOX® are specific to the preparation and the the specific assay methods used. They are not interchangeable with other preparations of BTX products; therefore, units of biological activity of BOTOX® cannot be accurately compared with or converted into units of any other BTX product.
Physicians must be aware of the risk of a preexisting a neuromuscular disorder. Individuals with peripheral neuropathic motor disease, amyotrophic lateral sclerosis, or neuromuscular junction disorder (eg, myasthenia gravis, Lambert-Eaton syndrome) should be monitored particularly closely when given BTX. Patients with neuromuscular disorders may be at increased risk of clinically significant local or distant effects, including severe dysphagia and respiratory compromise from typical doses of BOTOX®.
Future Directions
Solutions to pain disorders will stem from continued human and animal studies, which further define the biochemical and neurophysiological factors that influence these disorders. Of all medical specialists, neurologists may be best suited to analyze the complex physical and nonphysical components of chronic pain. Biochemical solutions in the chronic illness model also may make the neurologist best suited to adapt new treatments; however, further training in psychology and human behavior may be required in neurology residency programs if the specialty is to establish a prominent role in the management of these disorders. The future of pain management and research resides in multidisciplinary departments dedicated to the cross-section of knowledge and treatment disciplines required to manage pain disorders. As in all cases of human disease, the treatment of pain disorders will become more effective on the basis of results of future clinical research and vigorous outcome studies.
Questions & Answers
Overview
What are therapeutic injections for pain management?
What are the types of therapeutic injections used in pain management?
What equipment is needed to perform therapeutic injections for pain management?
How is needle navigation performed in therapeutic injections for pain management?
What is the role of local anesthetics in therapeutic injections for pain management?
Which local anesthetics are used in therapeutic injections for pain management?
What is the role of lidocaine in the performance of therapeutic injections for pain management?
What is the role of epinephrine in the performance of therapeutic injections for pain management?
What is the role of corticosteroids in therapeutic injections for pain management?
What are possible adverse reactions from corticosteroid injections for pain management?
What is the role of fluoroscopy in the performance of therapeutic injections for pain management?
How is fluoroscopy used to aid in the administration of therapeutic injections for pain management?
Which radiation safety measures are needed during therapeutic injections for pain management?
What are possible toxic reactions to local anesthetics for pain management injections?
What are possible complications of therapeutic injections to manage pain?
How is referred pain differentiated from local pain prior to therapeutic injection?
What is the role of therapeutic injections in the management of bursae pain?
What is the role of therapeutic injections in the management of tendinitis pain?
What is the role of therapeutic injections in the management of muscle spasm and myofascial pain?
What is the role of therapeutic injections in the management of painful scars?
What is the role of therapeutic injections in the management of neuromata?
What is the role of therapeutic injections in the management of muscle spasm and myofascial pain?
What is the role of suprascapular nerve block in pain management?
How is suprascapular nerve block administered for pain management?
What is the role of femoral nerve block in pain management?
How is femoral nerve block administered for pain management?
How is a lateral femoral cutaneous nerve block administered for pain management?
What is the role of sciatic nerve block in pain management?
How is a posterior sciatic nerve block administered in pain management?
What is the anterior approach to sciatic nerve block for pain management?
How is a sciatic nerve block at the popliteal fossa administered for pain management?
What is the role of occipital nerve blocks in pain management?
What is the role of a trigeminal ganglion block in pain management?
How is a trigeminal ganglion block administered for pain management?
What is the role of a maxillary nerve block in pain management?
What is the role of a mandibular nerve block in pain management?
How is a mandibular nerve block administered for pain management?
What is the role of glossopharyngeal nerve blocks in pain management?
How is a glossopharyngeal nerve block administered for pain management?
What is the role of a spinal interventional procedure for pain management?
What is the history of epidural corticosteroid injections for pain management?
What is the rationale for use of epidural steroids in pain management?
What is the role of epidural corticosteroids in pain management?
What is the efficacy of epidural corticosteroids for pain management?
What is the role of spinal synovial joint blocks in pain management?
What is the role of intra-articular corticosteroids in pain management?
What is the role of cervical medial branch blocks for pain management?
What is the role of cervical spinal nerve blocks in pain management?
What is the anatomy relevant to cervical spinal nerve blocks for pain management?
What is the role of cervical selective nerve root blocks in pain management?
How are cervical selective nerve root blocks administered for pain management?
What are the indications of selective nerve root blocks (SNRBs) in pain management?
What are complications of paravertebral block for pain management?
What is the role of cervical epidural blocks (CEBs) in pain management?
What is the efficacy of cervical epidural blocks (CEBs) for pain management?
How is the risk of complications from intraforaminal injections in pain management reduced?
How are interlaminar cervical epidural blocks (CEBs) administered for pain management?
What are possible complications of cervical epidural blocks (CEBs) for pain management?
What is the role of cervical facet blocks in pain management?
How is a cervical facet block administered for pain management?
What is the therapeutic goal of cervical facet blocks?
What is the role of atlantoaxial joint blocks in pain management?
What is the role of thoracic spinal nerve blocks in pain management?
How are thoracic paravertebral somatic nerve blocks administered for pain management?
What is the role of thoracic epidural nerve blocks in pain management?
How are thoracic epidural nerve blocks administered for pain management?
How is the paramedian approach to thoracic epidural nerve blocks for pain management administered?
What are the indications for thoracic epidural spinal blocks in pain management?
How is a mid-thoracic paramedian epidural spinal block performed for pain management?
What is the role of intercostal nerve blocks in pain management?
How is a posterior intercostal block administered for pain management?
How is a lateral intercostal block administered for pain management?
How is an anterolateral intercostal block administered for pain management?
What is the role of thoracic zygapophyseal joint blocks in pain management?
What is the role of lumbar selective nerve root blocks (SNRBs) in pain management?
How is lumbar selective nerve root blocks (SNRBs) administered for pain management?
What is the role of transforaminal epidural corticosteroid injections in pain management?
How are transforaminal epidural corticosteroid injections administered for pain management?
What is the role of lumbar paramedian epidural blocks in pain management?
How is a lumbar paramedian epidural block administered for pain management?
How are lumbar facet blocks administered for pain management?
How are lumbar medial branch blocks performed for pain management?
How are sacroiliac joint blocks administered for pain management?
How are caudal lumbar epidural blocks administered for pain management?
When is sympathetic blockade indicated in pain management?
What is the role of cervicothoracic sympathetic block in pain management?
How is a cervicothoracic sympathetic block administered for pain management?
How is an IV regional sympathetic block administered for pain management?
What are possible complications of IV regional sympathetic blocks for pain management?
How are IV neural blocks administered for pain management?
Which neurolytic agents are used in IV neural blocks for pain management?
When are neurolytic blocks indicated for pain management?
What are the disadvantages and complications of neurolytic blocks indicated for pain management?
What is the role of subarachnoid blocks in pain management?
How are subarachnoid blocks administered for pain management?
What is the role of extradural or epidural blockade in pain management?
What is the role of botulinum toxin (BTX) injections in pain management?
What is the role of botulinum toxin (BTX) injections for the management of musculoskeletal pain?
What is the efficacy of botulinum toxin (BTX) injections for the management of musculoskeletal pain?
What is the efficacy of botulinum toxin (BTX) injections for the management of myofascial pain?
What is the role of botulinum toxin (BTX) injection in the treatment of neck pain?
What is the role of botulinum toxin (BTX) in the treatment of low back pain?
What is the role of botulinum toxin (BTX) injections in the management of neuropathic pain?
What is the role of botulinum toxin (BTX) injection for the treatment of osteoarticular pain?
What is the role of botulinum toxin (BTX) injection for pain management in muscle spasticity?
What is the role of botulinum toxin (BTX) injections in urological pain management?
What is the role of botulinum toxin (BTX) injection for the treatment of interstitial cystitis (IC)?
What is the role of botulinum toxin (BTX) injections for pain management in rectal disorders?
What is the role of botulinum toxin (BTX) injection for pelvic pain management?
What is the role of botulinum toxin (BTX) injections in the treatment of primary headache disorders?
What is the efficacy of botulinum toxin (BTX) injections in the treatment of tension headaches?
What is the efficacy of botulinum toxin (BTX) injections for the treatment of cluster headaches?
What is the efficacy of botulinum toxin (BTX) for the treatment of chronic daily headaches?
What is the efficacy of botulinum toxin (BTX) injections for the treatment of cervicogenic headache?
What is the role of botulinum toxin (BTX) injections in the treatment of occipital neuralgia?
What are the indications for BOTOX® botulinum toxin (BTX) for pain management?
What are the guidelines for use of BOTOX® injections for the treatment of headaches?
What are dosing considerations for BOTOX® injections in pain management?
What are technical considerations for the use of botulinum toxin (BTX) in pain management?
What is included in preprocedural planning of botulinum toxin (BTX) injections for pain management?
What are the risks of BOTOX® injections for pain management?
What are future directions for therapeutic injections in pain management?
-
Anatomy of the suprascapular nerve and parascapular structures.
-
Suprascapular nerve block technique. See text for details.
-
Suprascapular nerve block technique. See text for details.
-
Anatomical relationship of the femoral nerve, artery, and vein.
-
Femoral nerve block technique (cross-sectional view). See text for details.
-
Lateral femoral cutaneous nerve block technique. See text for details.
-
Sciatic nerve block technique (lateral approach). See text for details.
-
Sciatic nerve block technique (lateral approach). See text for details.
-
Sciatic nerve block technique, lateral approach (cross-sectional view).
-
Anatomy of the fifth cranial nerve ganglion (trigeminal) along with innervation and peripterygoid relationship.
-
Anatomy of the fifth cranial nerve (trigeminal) ganglion and foramen ovale (cross-sectional view).
-
Lateral view of mandibular notch and plane of zygoma. Correlate with cross-sectional view of the fifth cranial nerve (trigeminal) ganglion and foramen ovale.
-
Anatomy and needle-insertion plane of trigeminal ganglion block technique. See text for details.
-
Anatomy and technique of trigeminal ganglion block. See text for details.
-
Pertinent anatomy with regard to the maxillary block.
-
Anatomy of maxillary block. See text for details.
-
Pertinent anatomy with regard to the mandibular block.
-
Pertinent coronal anatomy with regard to trigeminal nerve block.
-
Anatomy of mandibular block and needle insertion technique. See text for details.
-
Distal trigeminal block technique. See text for details.
-
Peristyloid anatomy (cross-sectional view).
-
Intraoral anatomy and glossopharyngeal block technique. See text for details.
-
Glossopharyngeal block, peristyloid technique.
-
Anatomy of the cervical nerves (anterior view).
-
Anatomy of the cervical nerves in the neck (transverse section).
-
Anatomy of the cervical nerves (lateral view).
-
Paravertebral block technique (posterior approach). See text for details.
-
Cervical spine local injection technique into the cavity of the right C5-C6 zygapophyseal joint (lateral view). See text for details.
-
Lateral position of patient for thoracic paravertebral somatic nerve block (paralaminar technique).
-
Anatomy of intercostal nerves (cross-sectional view).
-
Position of patient for posterior intercostal block technique.
-
Intercostal block technique. See text for details.
-
A - Posterior intercostal block technique. See text for details.
-
B - Posterior intercostal block technique. See text for details.
-
C - Posterior intercostal block technique. See text for details.
-
Lateral intercostal block along the posterior axillary line.
-
Anterolateral intercostal nerve block technique. See text for details.
-
Position of the patient for lumbar paravertebral somatic block technique.
-
Lumbar paravertebral somatic block technique. See text for details.
-
Lumbar paravertebral somatic block technique. See text for details.
-
Lateral view showing needle position of lumbar paravertebral somatic block technique.
-
Surface anatomy of caudal block and sacral hiatus localization.
-
Patient in the prone position for caudal block technique.
-
Caudal block technique. See text for details.
-
Three important sites that can be used to interrupt the peripheral sympathetic nervous system. The colored areas represent patterns of diffusion of local anesthetic solutions for the following techniques: cervicothoracic sympathetic block, celiac-splanchnic block, and lumbar sympathetic block.
-
Schematic anatomical representations, sympathetic chain and stellate ganglion.
-
Cervical and superior thoracic anatomy (anterolateral view).
-
Stellate block, important anatomical landmarks (surface and cross-sectional views).
-
Stellate block technique and anatomy. See text for details.
-
Pertinent anatomy for celiac plexus block.
-
Pertinent anatomy for celiac plexus block (cross-sectional view).
-
Retrocrural and anterocrural relationships (celiac plexus block).
-
Celiac plexus block, retrocrural (deep splanchnic) technique. See text for details.
-
Surface anatomy and markings for celiac plexus block.
-
Pertinent anatomy for lumbar sympathetic block (cross-sectional view).
-
Surface technique of lumbar sympathetic block. See text for details.
-
Lumbar sympathetic block, cross-sectional technique. See text for details.
-
Injection paragdigm for chronic migraine.
-
Lateral injection sites.
-
Frontal injection sites.
-
Oblique "Scotty Dog" view is shown in the bottom radiographic image of the lumbar spine.
-
C-arm fluoroscopic unit.
-
Typical fluoroscopic instrument panel.
-
The fluoroscopic imaging chain.
-
Needle tracking paths with bevel alone, bevel plus bend and rotation
-
Pushing sideways on a superficial needle changes the needle tips' direction. Pushing sideways on a deep needle bends the needle shaft without changing direction of tip.
-
Changing the needle's direction when needle tip is deep. Technique of bowing the needle shaft changes the direction of a deep needle tip.
-
Typical placements for cervical, thoracic, and lumbar interlaminar epidural steroid injections.
Tables
What would you like to print?
- Types of Therapeutic Injections
- Guidelines for Therapeutic Application
- Technical Application
- Adverse Effects and Complications of Neural Blockade
- Commonly Practiced Neural and Structural Blocks
- Clinical Application of Spinal Injection Techniques
- Technical Principles of Spinal Neural Blockade
- Sympathetic Nervous System Blockade
- Chemodenervation with Botulinum Toxin for Pain Treatment
- Future Directions
- Questions & Answers
- Show All
- Media Gallery
- Tables
- References