Practice Essentials
Obstructive sleep apnea (OSA)—also referred to as obstructive sleep apnea-hypopnea—is a sleep disorder that involves cessation or significant decrease in airflow in the presence of breathing effort. It is the most common type of sleep-disordered breathing and is characterized by recurrent episodes of upper airway collapse during sleep. [1] These episodes are associated with recurrent oxyhemoglobin desaturations and arousals from sleep.
OSA that is associated with excessive daytime sleepiness is commonly called obstructive sleep apnea syndrome—also referred to as obstructive sleep apnea-hypopnea syndrome.
The image below illustrates the sleep-related disordered breathing continuum ranging from simple snoring to OSA.
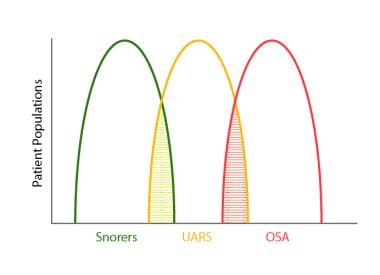 Sleep-related disordered breathing continuum ranging from simple snoring to obstructive sleep apnea (OSA). Upper airway resistance syndrome (UARS) occupies an intermediate position between these extremes. Note areas of overlap among the conditions.
Sleep-related disordered breathing continuum ranging from simple snoring to obstructive sleep apnea (OSA). Upper airway resistance syndrome (UARS) occupies an intermediate position between these extremes. Note areas of overlap among the conditions.
Signs and symptoms
Generally, symptoms of OSA begin insidiously and are often present for years before the patient is referred for evaluation.
Nocturnal symptoms may include the following:
-
Snoring, usually loud, habitual, and bothersome to others
-
Witnessed apneas, which often interrupt the snoring and end with a snort
-
Gasping and choking sensations that arouse the patient from sleep, though in a very low proportion relative to the number of apneas they experience
-
Nocturia
-
Insomnia; restless sleep, with patients often experiencing frequent arousals and tossing or turning during the night
Daytime symptoms may include the following:
-
Nonrestorative sleep (ie, “waking up as tired as when they went to bed”)
-
Morning headache, dry or sore throat
-
Excessive daytime sleepiness that usually begins during quiet activities (eg, reading, watching television); as the severity worsens, patients begin to feel sleepy during activities that generally require alertness (eg, school, work, driving)
-
Daytime fatigue/tiredness
-
Cognitive deficits; memory and intellectual impairment (short-term memory, concentration)
-
Decreased vigilance
-
Morning confusion
-
Personality and mood changes, including depression and anxiety
-
Sexual dysfunction, including impotence and decreased libido
-
Gastroesophageal reflux
-
Hypertension
See Clinical Presentation for more detail.
Diagnosis
In general, the physical examination is normal in patients with OSA, aside from the presence of obesity (body mass index: >30 kg/m2), an enlarged neck circumference (men: >43 cm [17 in]; women: >37 cm [15 in]), and hypertension.
Evaluate the upper airway in all patients, particularly in nonobese adults with symptoms consistent with OSA.
Examination findings may include the following:
-
Abnormal (increased) Mallampati score: Identifies risk for difficult tracheal intubation
-
Narrowing of the lateral airway walls: Independent predictor of the presence of obstructive sleep apnea in men but not women
-
Enlarged (ie, "kissing") tonsils (3+ to 4+)
-
Retrognathia or micrognathia
-
Large degree of overjet
-
High-arched hard palate
-
Systemic arterial hypertension: Present in about 50% of obstructive sleep apnea cases
-
Congestive heart failure
-
Pulmonary hypertension
-
Stroke
-
Metabolic syndrome
-
Type 2 diabetes mellitus
Testing
An overnight sleep study, or polysomnography, is required to diagnose OSA.
Routine laboratory tests, however, are usually not helpful in OSA unless a specific indication is present. Pulmonary function tests are not indicated to make a diagnosis of, or treatment plan for, OSA alone. The standard indications for such testing apply to all patients, with or without OSA.
Obtain a thyrotropin test on any patient with possible OSA who has other signs or symptoms of hypothyroidism, particularly in elderly individuals.
AASM standards and guidelines for diagnostic polysomnography
The American Academy of Sleep Medicine guidelines for the indications and performance of polysomnography include the following [2] :
-
Sleep stages are recorded via an electroencephalogram, electro-oculogram, and chin electromyogram
-
Heart rhythm is monitored with a single-lead electrocardiogram
-
Leg movements are recorded via an anterior tibialis electromyogram
-
Breathing is monitored, including airflow at the nose and mouth (using both a thermal sensor and a nasal pressure transducer), effort (using inductance plethysmography), and oxygen saturation
-
The breathing pattern is analyzed for the presence of apneas and hypopneas (as per definitions standardized by the American Academy of Sleep Medicine)
See Workup for more detail.
Management
Treatment of OSA partly depends on the patients’ severity of sleep-disordered breathing. Those with mild apnea have more options, whereas people with moderate to severe apnea should be treated with nasal continuous positive airway pressure (CPAP).
Conservative therapy and prevention
The following conservative measures may help manage or prevent OSA:
-
Restriction of body positions during sleep (avoid supine position)
-
Sleeping in an upright position for markedly obese patients
-
Avoiding smoking; smoking cessation
-
Avoiding alcohol and other sedatives (particularly 4-6 hours before bedtime)
-
Avoiding sleep deprivation
Mechanical measures
Mechanical measures used in the treatment of OSA include the following:
-
Nasal CPAP: Standard treatment option
-
Bilevel positive airway pressure
-
Oral appliance therapy
Pharmacotherapy
Medications are generally not a part of the primary treatment recommendations for OSA. However, central nervous system stimulants (eg, modafinil, armodafinil) or solriamfetol (a dopamine/norepinephrine reuptake inhibitor) may be considered for adjunctive use to treat excessive daytime sleepiness in the management of this condition.
Surgery
Surgical intervention for OSA includes, but is not limited to, the following:
-
Uvulopalatopharyngoplasty
-
Craniofacial reconstruction with advancement of tongue or maxillomandibular bones
-
Tracheostomy
See Treatment and Medication for more detail.
Background
Obstructive sleep apnea (OSA)—also referred to as obstructive sleep apnea-hypopnea (OSAH)—is a sleep disorder that involves cessation or significant decrease in airflow in the presence of breathing effort. It is the most common type of sleep-disordered breathing (SDB) and is characterized by recurrent episodes of upper airway (UA) collapse during sleep. [1] These episodes are associated with recurrent oxyhemoglobin desaturations and arousals from sleep.
OSA associated with excessive daytime sleepiness (EDS) is commonly called obstructive sleep apnea syndrome (OSAS)—also referred to as obstructive sleep apnea-hypopnea syndrome (OSAHS). Despite being a common disease, OSAS is underrecognized by most primary care physicians in the United States; an estimated 80% of Americans with OSAS are not diagnosed. [3]
Apnea may occur hundreds of times nightly, 1-2 times per minute, in patients with severe OSA, and it is often accompanied by wide swings in heart rate, a precipitous decrease in oxygen saturation, and brief electroencephalographic (EEG) arousals concomitant with stertorous breathing sounds as a bolus of air is exhaled when the airway reopens.
The cardinal symptoms of sleep apnea include the "3 S ’s": S noring, S leepiness, and S ignificant-other report of sleep apnea episodes. This helpful mnemonic has proven to be valuable in teaching residents to be sensitive in the identification and appropriate referral of these patients for further study.
Also helpful is if patients’ spouses or others who are close to them can attend visits. Often, sleepers are unaware that they have OSA and may in fact regard themselves as "good sleepers" because they "can sleep anytime, anywhere" (eg, in the physician’s waiting room, in traffic, in class, at his or her office). Sleepiness is one of the potentially most morbid symptoms of sleep apnea, owing to the accidents that can occur as a result of it.
OSA is a very important diagnosis for physicians to consider because of its strong association with and potential cause of the most debilitating medical conditions, including hypertension, cardiovascular disease, coronary artery disease, insulin-resistance diabetes, depression, and, as mentioned, sleepiness-related accidents.
Go to Childhood Sleep Apnea for complete information on this topic.
Definitions of respiratory events
For the purposes of the following discussion, it is useful to define the breathing events being examined. These breathing events include the following:
-
Apnea
-
Hypopnea
-
Respiratory effort–related arousal (RERA)
Apnea is defined by the American Academy of Sleep Medicine (AASM) as the cessation of airflow for at least 10 seconds. [4] Apnea may last for 30 seconds or even longer.
The most recent guidelines from the American Academy of Sleep Medicine (AASM Weekly Update 9/26/2013) updated the definitions of the terms for scoring hypopneas (recommended and acceptable), as follows:
-
Recommended: Score a respiratory event as a hypopnea if all of the following criteria are met: (1) peak signal excursions drop by at least 30% of pre-event baseline using nasal pressure (diagnostic study), positive airway pressure device flow (titration study), or an alternative hypopnea sensor (diagnostic study); (2) duration of the at least 30% drop in signal excursion is 10 or more seconds; and (3) there is 3% or greater oxygen desaturation from pre-event baseline and/or the event is associated with an arousal.
-
Acceptable: Score a respiratory event as a hypopnea if all of the following criteria are met: (1) the peak signal excursions drop by 30% or greater of pre-event baseline using nasal pressure (diagnostic study), positive airway pressure device flow (titration study), or an alternative hypopnea sensor (diagnostic study); (2) the duration of the at least 30% drop in signal excursion is 10 or more seconds; and (3) there is 4% or greater oxygen desaturation from pre-event baseline.
An RERA is an event characterized by increasing respiratory effort for 10 seconds or longer leading to an arousal from sleep but one that does not fulfill the criteria for a hypopnea or apnea. The criterion standard to measure RERAs is esophageal manometry, as the AASM recommends. However, esophageal manometry is uncomfortable for patients and impractical to use in most sleep centers.
A reliable and valid way to measure RERAs is with the use of a nasal cannula and pressure transducer. Results obtained with this transducer are reliable. With regard to the diagnosis of OSA, this method does not differ from esophageal manometry in a clinically significant manner. With either method, the respiratory disturbance index (RDI) is greater than 5 and the normal RDI cutoff is greater than 15.
Obstructive apneas and hypopneas are typically distinguished from central events. Obstructive events are characterized by continued thoracoabdominal effort in the setting of partial or complete airflow cessation, central events by lack of thoracoabdominal effort in this setting. Mixed events have both obstructive and central features. They generally begin without thoracoabdominal effort and end with several thoracoabdominal efforts in breathing; they are tabulated in the obstructive apnea index.
Sleep-related breathing disorder continuum
A sleep-related breathing disorder (SRBD) continuum has been described and is supported by research. [5] OSA can be thought of as occupying a range of this continuum.
The idea of the SRBD continuum was first described by Elio Lugaresi: "There is a continuum of intermediate clinical conditions between trivial snoring and the most severe forms of OSAS (which we prefer to call heavy snorers disease). This fact should be taken into consideration for any meaningful approach to the clinical problems posed by snoring. Many issues, however, remain unsettled." [6]
The SRBD continuum suggests that snoring is the initial presenting symptom, and it increases in severity over time and it increases in association with medical disorders that may serve to exacerbate the disorder, such as obesity. Snoring has a constellation of pathophysiological effects. [7]
As the disease progresses, SRBD patients begin to develop increased UA resistance that results in a new hallmark symptom: sleepiness. Sleepiness is caused by increased arousals from sleep. [8] This syndrome has been described as the UA resistance syndrome (UARS). UARS patients are not hypoxic, and hypoxia does not explain why they are sleepy, nor can sleep stage percentages or other polysomnography (PSG) variables. The SRBD continuum predicts that over time, a UARS patient develops OSA, if untreated (see the image below).
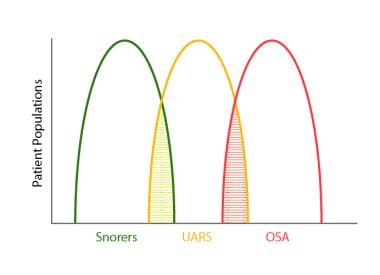 Sleep-related disordered breathing continuum ranging from simple snoring to obstructive sleep apnea (OSA). Upper airway resistance syndrome (UARS) occupies an intermediate position between these extremes. Note areas of overlap among the conditions.
Sleep-related disordered breathing continuum ranging from simple snoring to obstructive sleep apnea (OSA). Upper airway resistance syndrome (UARS) occupies an intermediate position between these extremes. Note areas of overlap among the conditions.
OSA has as its hallmark symptoms snoring, sleepiness, spouse apnea report, and hypoxia. The SRBD continuum suggests that over time, untreated OSA may hasten death through heart disease, hypertension, stroke, myocardial infarction, heart failure, cardiac arrhythmia, diabetes, metabolic syndrome, or vehicular or other accident due to sleepiness or other behavioral effects noted.
Pathophysiology
Conceptually, the UA is a compliant tube and, therefore, is subject to collapse. [9] OSA is caused by soft tissue collapse in the pharynx.
Transmural pressure is the difference between intraluminal pressure and the surrounding tissue pressure. If transmural pressure decreases, the cross-sectional area of the pharynx decreases. If this pressure passes a critical point, pharyngeal closing pressure is reached. Exceeding pharyngeal critical pressure (Pcrit) causes a juggernaut of tissues collapsing inward. The airway is obstructed. Until forces change transmural pressure to a net tissue force that is less than Pcrit, the airway remains obstructed. OSA duration is equal to the time that Pcrit is exceeded.
Most patients with OSA demonstrate upper airway obstruction at either the level of the soft palate (ie, nasopharynx) or the level of the tongue (ie, oropharynx). Research indicates that both anatomic and neuromuscular factors are important.
Anatomic factors (eg, enlarged tonsils; volume of the tongue, soft tissue, or lateral pharyngeal walls); length of the soft palate; abnormal positioning of the maxilla and mandible) may each contribute to a decrease in the cross-sectional area of the upper airway and/or increase the pressure surrounding the airway, both of which predispose the airway to collapse. [10, 11] Note that in adults, it is very rare for enlarged tonsils and adenoids to be a cause of OSA. Removing the enlarged adenoids and tonsils alone rarely is an effective surgical remedy; in children, about 80% who have have OSA are cured with the removal of enlarged adenoids and tonsils. There is often a misconception that enlarged adenoids and tonsils may be a singular cause of OSA in both children and adults, but this is not true.
Neuromuscular activity in the UA, including reflex activity, decreases with sleep, and this decrease may be more pronounced in patients with OSA. [12, 13, 14] Reduced ventilatory motor output to upper airway muscles is believed to be the critical initiating event leading to UA obstruction; this effect is most pronounced in patients with a UA predisposed to collapse for anatomical reasons.
Central breathing instability is a well-established factor contributing to the development of central sleep apnea (CSA), particularly in patients with severe congestive heart failure (CHF). [15, 16, 17] Evidence also indicates that central breathing instability contributes to the development of OSAS.
First, evidence of UA obstruction in the absence of ventilatory motor output (central sleep apnea) has been observed. [18] Second, reduction in pharyngeal dilator activity has been associated with periodic breathing [19, 20, 21] and hypocapnia in subjects with evidence of inspiratory flow limitation. [22] Third, men have been shown to be more susceptible to the development of CSA and less responsive to carbon dioxide than women are, [23] a result consistent with the greater prevalence of OSAS in men than in women.
Static and dynamic pathophysiologic factors
Both static factors and dynamic factors are involved in the development of OSA. Static factors include surface adhesive forces, neck and jaw posture, tracheal tug, and gravity. Any anatomic feature that decreases the size of the pharynx (eg, retrognathia) increases the likelihood of OSA. Gravitational forces are felt simply by tilting one’s head back to where the retroposition of the tongue and soft palate reduce the pharyngeal space. For most patients, OSA worsens in the supine sleeping position.
An important static factor that has been found is the reduced diameter of the pharyngeal airway in wakefulness in OSA patients compared with non-OSA patients. In the absence of craniofacial abnormalities, the soft palate, tongue, parapharyngeal fat pads, and lateral pharyngeal walls are enlarged in OSA patients versus non-OSA patients.
Dynamic factors include nasal and pharyngeal airway resistance, the Bernoulli effect, and dynamic adherence.
The Bernoulli effect plays an important dynamic role in OSA pathophysiology. In accordance with this effect, airflow velocity increases at the site of stricture in the airway. As airway velocity increases, pressure on the lateral wall decreases. If the transmural closing pressure is reached, the airway collapses. The Bernoulli effect is exaggerated in areas where the airway is most compliant. Loads on the pharyngeal walls increase adherence and, hence, increase the likelihood of collapse.
This effect helps to partially explain why obese patients, and particularly those with fat deposition in the neck, are most likely to have OSA. Moreover, the cross-sectional area of the airway in patients with OSA is smaller than that of people without OSA; this difference is due to the volume of the soft tissue, including the tongue, lateral pharyngeal walls, soft palate, and parapharyngeal fat pads. In one study, the increased volume of these areas was independent of sex, age, ethnicity, craniofacial size, and fat deposition surrounding the UA. [10]
Given these principles, it is understandable why the likelihood of OSA is increased among obese patients, why weight loss decreases the risk of OSA, and why physical examination helps in predicting the presence of OSA. However, the clinical situation is complex because of the interplay of known static and dynamic factors and because of unknown factors.
Data do not explain why sex, age, and ethnicity are not evenly distributed across epidemiologic studies of OSA patients. (See Epidemiology.) Furthermore, data or physical findings are not helpful for determining with precision who will or will not have OSA and who can or who cannot be cured with UA surgery.
Apnea clusters and oxygen desaturation
OSA often occurs in clusters. An oxygen desaturation occurs with each apnea. The end of the apnea sequence typically ends with a brief (>3 sec) EEG arousal. In patients with severe OSA, the cluster of apneas occurs throughout sleep. The desaturation from the first apnea event is typically associated with a higher desaturation percentage change than subsequent apneas in the series.
An underlying mechanism for how clusters of apneas occur and the rate of oxygen desaturation has been recently studied. [24] The researchers paralyzed lambs and withdrew mechanical ventilation to produce apnea and target oxygen saturation. Once the target was reached and the number of recurrent apneas was met, they stimulated respiration through the ventilator so that oxygen saturation was more than 85%.
The study found that oxygen desaturation was not significantly correlated with resting oxygen saturation, independent of mixed-venous oxygen saturation, using forward stepwise regression modeling. It predicted increased desaturation rates solely based on the size of oxygen reuptake. [24] This occurs when mixed-venous blood with depleted oxygen saturation arrives at the lung in time with the apnea phase.
The rapid change in oxygen desaturation occurred after the second apnea in a series of 10 produced; apneas that followed the second apnea did not have accelerated changes when compared with the second apnea. Isolated apneas did not show rapid changes in oxygen saturation.
The clinical implications of these findings suggest that the reason why continuous positive airway pressure (CPAP) and supplemental oxygen may work to ameliorate rapid desaturation is related to the extent that apneas can remain isolated. This results in a longer ventilatory phase to allow venous reoxygenation.
It should be kept in mind that the events studied were not obstructive events but were apneas associated with hypoxemia. They were not terminated by EEG arousals in a natural way to end an apnea sequence and were not produced in humans. Therefore, this study’s clinical application is associated with several caveats.
Oxidative stress, inflammation, and cardiovascular disease
An excellent review article by Gozal and Kheirandish-Gozal provides a model that attempts to integrate how oxidative stress and inflammatory processes link OSA and cardiovascular disease. [25]
Genetic studies have revealed that the gene that encodes for oxidative stress uniquely contributes toward OSA. [26] This suggests that the development of OSA may be related to inflammation and is not necessarily related to a trigger for oxidative stress, as was previously thought. The gene may play a pivotal role by operating in a positive feedback loop, causing the OSA to begin with and then triggering an inflammatory response that further narrows the UA, exacerbating the OSA.
Etiology
The etiology of OSA involves both structural and nonstructural factors, including genetic factors.
Structural factors
Structural factors related to craniofacial bony anatomy that predispose patients with OSA to pharyngeal collapse during sleep include the following:
-
Innate anatomic variations (facial elongation, posterior facial compression)
-
Retrognathia and micrognathia
-
Mandibular hypoplasia
-
Brachycephalic head form - Associated with an increased AHI in whites but not in African Americans. [27]
-
Inferior displacement of the hyoid
-
Adenotonsillar hypertrophy, particularly in children and young adults
-
High, arched palate (particularly in women)
Structural factors related to nasal obstruction that predispose patients with OSA to pharyngeal collapse during sleep include polyps, septal deviation, tumors, trauma, and stenosis. Structural factors related to retropalatal obstruction include (1) an elongated, posteriorly placed palate and uvula and (2) tonsil and adenoid hypertrophy (particularly in children). Structural factors related to retroglossal obstruction include macroglossia and tumor.
Studies confirm that craniofacial abnormalities are important in the pathogenesis of OSA, particularly in nonobese patients and children. Moreover, given that different racial groups are inclined to develop OSA at varying degrees of obesity, clinicians should particularly consider the possibility of this disorder in the presence of clinically detectable craniofacial abnormalities. [28, 29]
Previous studies of craniofacial risk factors for OSA have been based predominantly on cephalometry. However, differences in head form (measured by the cranial index) and facial form (measured by the facial index) are considered by anthropologists to provide a basis for structural variation in craniofacial anatomy.
The association of head and facial form with the AHI was assessed in 364 whites and 165 African Americans. Cranial and facial dimensions were measured using anthropometric calipers, and other data collected included the body mass index (BMI), neck circumference, and the AHI.
Cranial index and facial index in whites with OSA (AHI ≥15) differ from those in whites without OSA (AHI < 5). The cranial index was increased and the facial index decreased in subjects with OSA. Cranial and facial indices did not differ in African American subjects based on OSA diagnosis. In whites with OSA, the cranial index was again greater and the facial index was again smaller than in African Americans. The researchers suggested that the cranial index may be useful in phenotyping and identifying population subsets with OSA. [27]
Nonstructural risk factors
Nonstructural risk factors for OSA include the following:
-
Obesity
-
Central fat distribution
-
Male sex
-
Age
-
Postmenopausal state
-
Alcohol use
-
Sedative use
-
Smoking
-
Habitual snoring with daytime somnolence
-
Supine sleep position
-
Rapid eye movement (REM) sleep
Familial factors also play a role (see below). [30] Families with a high incidence of OSA are reported. Relatives of patients with SDB have a 2- to 4-fold increased risk of SDB compared with control subjects.
Other conditions associated with the development of OSA are as follows:
-
Hypothyroidism
-
Neurologic syndromes
-
Stroke
-
Acromegaly
-
Environmental exposures
Hypothyroidism is associated with macroglossia and increased soft tissue mass in the pharyngeal region and thus with an increased risk of SDB. Hypothyroidism is also associated with myopathy that may contribute to UA dysfunction. Although it has been linked with the development of OSA, evidence indicates that its prevalence is no higher in patients with OSA than in the general population. Accordingly, patients with OSA should not be routinely screened for hypothyroidism, except possibly elderly women.
Neurologic syndromes associated with OSA include postpolio syndrome, muscular dystrophies, and autonomic failure syndromes such as Shy-Drager syndrome.
The relationship of OSA to cerebrovascular disease is still being determined. Growing evidence indicates that the prevalence of OSA is increased in patients who have had a stroke. However, whether OSA is a risk factor for stroke or stroke is a risk factor for developing OSA remains unclear.
Like hypothyroidism, acromegaly is associated with macroglossia and increased soft tissue mass in the pharyngeal region and thus with an increased risk of SDB.
Environmental exposures include smoke, environmental irritants or allergens, and alcohol and hypnotic-sedative medications.
Genetic factors
A study examined 52 candidate genes most likely to influence OSA. [26] The study sample included 792 African Americans and 694 European Americans, all older than 18 years. An AHI of 15 or higher was used to define OSA as a clinical entity; the AHI was statistically used as both a continuous and a dichotomous trait. In the African American subjects, 1,080 single nucleotide polymorphisms (SNPs) were genotypes; in the European Americans, 505 SNPs were genotypes. Statistical analysis controlled for adjusted for age, age-squared, and sex, with and without BMI.
The study found the following variants in European Americans: C-reactive protein (CRP) and glial cell line-derived neurotrophic factor (GDNF) were associated with the AHI as both a longitudinal and a dichotomous trait. CRP findings increased the odds ratio for the risk of OSA between 1.45 and 2.87; GDNF increased the odds ratio between 1.53 and 3.89-3.92 for the GDNF gene that looked at risk allele G and GDNF risk allele A, respectively.
The study found the following variant in African Americans with OSA: r9s526240 within serotonin receptor 2a. Risk allele A increased the odds ratio for risk of obstructive sleep apnea from 1.45-2.91 using the reported 95% confidence interval.
CRP appears to mediate inflammation; it is thought to be a marker of inflammation. Such inflammation may increase OSA by increasing mucosal edema and reducing airway caliber.
GDNF influences ventilatory control. It appears to sense oxygen and carbon dioxide at sleep onset transitions, hence playing a role in CSA. GDNF influences the growth of sensory afferent neurons of the carotid body, influencing responses to hypoxia. Its role extends to influencing the growth of neural pathways that are important for normal respiration, specifically at the A5 nucleus of the ventrolateral pons, a critical area that regulates respiratory pattern generation.
The role of 5HT2A includes effects on sleep-wake cycles, importantly influencing rapid eye movement (REM) sleep stage percentage. Medications such as selective serotonin reuptake inhibitors (SSRIs) that occupy 5HT2A receptors reduce or eliminate REM sleep percent time. Other mentioned roles include regulation of upper airway dilator muscle through an excitatory influence on hypoglossal motor output. 5HT2a is involved in appetite regulation, thus playing a role in obesity, a well-known risk factor for obstructive sleep apnea.
The study used rather strict criteria to identify other candidate genes, and less stringent criteria identified other possible candidate genes that may influence the risk of OSA.
Epidemiology
SDB is common in the United States. The National Commission on Sleep Disorders Research estimated that minimal SDB (RDI >5) affects 7-18 million people in the United States and that relatively severe cases (RDI >15) affect 1.8-4 million people. The prevalence increases with age. SDB remains undiagnosed in approximately 92% of affected women and 80% of affected men.
OSA is increasingly prevalent, in both adults and children, in modern society. The estimated prevalence has been 2% for women and 4% for men. [31, 32] Similar data have been found in an epidemiologic study from Pennsylvania. [10, 33] More recent research indicates a prevalence of 4% for women and 9% for men. Data from the Wisconsin Cohort Study indicate that the prevalence of OSA in people aged 30-60 years is 9-24% for men and 4-9% for women.
The prevalence in children is less certain, but the author’s sleep center is seeing increasing numbers of adolescent patients, who are often obese and present similarly to many of their adult counterparts, with the important exception that they may be sleepy and/or hyperactive. A 2007 study has suggested that approximately 6% of adolescents have weekly SDB. [34]
International statistics
The prevalence of OSA in non-American populations has only been studied in men and has been found to be as low as 0.3% (England) and as high as 20-25% (Israel and Australia). The prevalence of OSA in Australian men is estimated to be 3%.
Age distribution for OSA
Aging is an important consideration of risk for OSA. OSA prevalence increases 2-3 times in older persons (>65 y) compared with individuals aged 30-64 years, [35, 36] with an estimated rate as high as 65% in a community sample of people older than 65 years. [37]
After age 65 years, no further relative disparity is noted in the incidence of OSA. One explanation for this plateau is the relative increase in mortality in persons older than 65 years; however, data to support this contention, as attractive as it appears, are insufficient. Scant data are available to help clinicians determine if clinical management should differ between the age cohorts.
Sex distribution for OSA
The male-to-female ratio in community-based studies is 2-3:1. [31, 38] Androgenic patterns of body fat distribution (deposition in the trunk, including the neck area) predispose men to OSA. In general, sex hormones may affect neurologic control of UA-dilating muscles and ventilation.
In population studies that have examined the incidence of OSA, women were not only less likely than men to have OSA but also less likely to be diagnosed early in the disease process. Survival rates are lower for women than for men, after an OSA diagnosis has been established by PSG, presumably due to the delayed OSA diagnosis.
Three large epidemiologic studies have demonstrated that the prevalence of OSA in women appears to increase after menopause. [39, 40, 41] In these studies, women on hormone replacement therapy (HRT) had a prevalence similar to that of premenopausal women. Postmenopausal women are 3 times more likely to have moderate-to-severe OSA compared with premenopausal women. Women who are on HRT are half as likely to have OSA compared with postmenopausal women who are not on HRT. [42]
Premenopausal women with OSAHS tend to be more obese than men with the same severity of disease. Thin women with symptoms of OSAHS appear to have an increased frequency of craniofacial abnormalities.
Evidence indicates that women underreport the symptoms of loud snoring and witnessed apneas, leading to underreferral to sleep centers. This may explain the marked male predominance (male-to-female ratio of approximately 8:1) in sleep center–based studies. Additionally, women have lower AHIs than men, even after correcting for other demographic factors such as BMI and neck circumference. [43, 44, 45]
Prevalence of OSA by race or ethnicity
African American individuals appear to be more predisposed to SDB than white persons. This increased predisposition varies according to age. The odds ratio is greater than 3 in children younger than 13 years and is 1.88 in persons younger than 25 years. In elderly African Americans, the risk is increased 2-fold. Examination of craniofacial morphology found that brachycephaly is associated with an increased AHI in whites but not in African Americans. [27]
Chinese patients with OSA have a more crowded upper airway and relative retrognathia compared with their white counterparts, with statistical controls for BMI and neck circumference. [9] Asians are known to have a shorter cranial base and a more acute cranial base flexure, increasing OSA risk, with BMI and neck circumference being roughly equal. Therefore, interestingly, obesity plays a more prominent role in OSA predisposition in whites than in Chinese persons. This may serve to underscore the role that craniofacial factors have in Chinese patients.
Other populations that may be at increased risk include Mexican Americans and Pacific Islanders.
Prognosis
The short-term prognosis, in relation to symptoms such as daytime sleepiness and snoring, ranges from good to excellent with regular use of CPAP. Several studies, including placebo-controlled studies, have shown significant improvement in measures of cognitive function and general health status (eg, as measured by the Medical Outcome Study Short-Form 36 health survey) after 4-8 weeks of treatment with CPAP. However, studies have not been performed in a large population or for more than a 4- to 8-week treatment period.
The long-term prognosis is unknown because no randomized treatment studies investigating the effect of CPAP on preventing the development of cardiovascular sequelae have been conducted.
Cardiovascular mortality and morbidity
The effect of OSA on mortality has been investigated using observational cohort studies. Marin et al found in a Spanish cohort that severe untreated OSA (AHI >30) is associated with an increased risk of cardiovascular mortality, defined by fatal myocardial infarction (MI) or stroke. [46] Patients with mild OSA or those undergoing treatment with CPAP did not have a significantly increased odds ratio compared with a group of subjects without OSA. [46]
In this study, the authors also found that untreated severe OSA is a significant risk factor for the development of cardiovascular morbidity, which included nonfatal MI and stroke.
Two 2008 population-based studies, one from the United States [47] and one from Australia, [48] also showed increased all-cause mortality in subjects with moderate-to severe OSA. The adjusted hazard ratios in both studies ranged from 3-6.24 for subjects with moderate-to-severe disease compared with no disease.
In the Sleep Heart Health Study, [49] 6441 men and women were followed for a mean of 8.2 years. Increased mortality was observed in patients with OSA, but the effect was primarily observed in men younger than 70 years. Women and men older than 70 years did not have increased mortality. In addition, the increased mortality was seen primarily in patients with the most oxygen desaturation during their sleep.
A 2012 study examined the association between OSA and mortality. Using portable sleep studies with more than 77,000 patients, the authors found that OSA was associated with all-cause mortality in patients younger than 50 years of age. While this is a general conclusion from the study, other variables played a substantial role in mediating this relationship. These data are consistent with earlier data showing that the negative impact of OSA on health is more profound in younger patients. [50]
Campos-Rodriguez et al reported that severe OSA is associated with cardiovascular death in women, and adequate CPAP treatment may reduce this risk. [51] A study in the elderly also suggests that severe OSA not treated with CPAP is associated with an increased risk of cardiovascular death. [52]
Several other studies indicate that CPAP mitigates the increased mortality observed in OSA. In addition to the article from Spain discussed above, a 2005 article [53] suggests that mortality is associated with compliance with CPAP. In a historical cohort of 871 patients, patients who used CPAP more than 6 hours per night had an increased survival rate (96.4%) at 5 years compared with those who used CPAP 1-6 hours per night (91.3%) and less than 1 hour per night (85.5%). Use for more than 6 hours per night was associated with a significantly decreased odds ratio of 0.1.
Patients with a history of ischemic stroke and sleep apnea who regularly used their CPAP device had a decreased mortality compared with those who did not use their CPAP device. [54]
A 2005 study found that OSA was associated with an increased risk of sudden death between the hours of midnight and 6 AM, as compared with the general population (in whom sudden death is more common between 6 AM and noon). [55]
Evidence indicates that OSA is not an independent risk factor for the development of pulmonary hypertension in the absence of other lung disease, as evidenced by the presence of daytime hypoxemia, hypercapnia, or obstructive airway disease. [56]
A study of 150 newly diagnosed patients with OSA by Baguet determined that left ventricular diastolic dysfunction is common in these patients and is related to the severity of oxygen desaturation. [57]
All of the above evidence strongly suggests that OSA is an independent risk factor for the development of cardiovascular disease and death. However, at this time, no definitive randomized studies have investigated the effect of CPAP in preventing the potential cardiovascular risks.
Increased risk of motor vehicle accidents
Many studies have identified a relationship between OSA and motor vehicle accidents. Patients with OSA have been reported to be 2-7 times as likely as control individuals to have a motor vehicle crash; the overall estimated risk was 2.5 in a meta-analysis of 6 studies. [58] Many studies indicate that motor vehicle accidents are more common in patients with severe OSA (generally, AHI >30), [59, 60] but this is not a universal finding. [61]
Methods for predicting if an individual patient will have an automobile accident are not yet sufficiently reliable. Using increasingly refined and realistic driving simulators, Ghosh et al could predict those who failed a driving simulation test compared to those who passed the test. The simulation is a step forward in prediction, but simulation has not yet reached levels that would allow a clinician to determine if an OSA patient is safe to drive a vehicle or not. Though the more severely impaired OSA patients were selected for the study, many of them were able to finish the 50-minute driving simulator without incident. The authors continue to work to refine the simulator. It would be an advance to find a test that is sufficiently reliable for use in the clinical setting. [62]
A study from Australia found that truck drivers with Epworth Sleepiness Scale (ESS) scores higher than 18 had an odds ratio of 2.67 for multiple accidents. [63]
An Internet-linked survey of 35,217 respondents found that subjects who reported at least one near-miss sleepy accident were 1.13 times as likely to have had one actual accident compared with subjects not reporting a near-miss accident. [64] The odds ratio increased to 1.87 for those reporting 4 or more near-miss sleepy accidents. This study indicates that asking patients about near-miss sleepy accidents may be predictive of future accident risk.
Predicting accident risk in patients with OSA is difficult because many individuals with OSA do not accurately perceive their level of drowsiness. No evidence indicates that sleep latency derived from either the multiple sleep latency test (MSLT; a measure of sleep propensity) or the maintenance of wakefulness test (MWT; a measure of wake tendency) are predictive of accident risk.
A large body of work has been compiled on the influence of OSA on driving-simulator performance, with most studies indicating poor performance, similar to that seen with alcohol impairment while driving [65, 66] (though performance may return to normal after treatment). However, whether driving-simulator performance is an accurate predictor of real-world driving is unclear, [67] and no evidence indicates that simulator performance can be used to predict accident risk in OSA patients. [68]
Evidence indicates that CPAP improves driving performance. At least 2 studies have shown improvement on a driving simulator after CPAP use. [69, 70] Specifically, in one study, the number of off-road events decreased from 17.8 to 9 after 1 month of effective CPAP therapy, but no change was noted after a month of ineffective pressure set at 1 cm water.
In addition, 2 studies have looked at the effect of CPAP on actual motor vehicle accident rates. George derived crash rates from Department of Motor Vehicle data for 210 patients with OSA over a 3-year period before and after CPAP therapy; the crash rate was 0.18 while untreated, but fell to 0.06 with treatment. [71] Findley et al reported no further crashes in a group of 36 patients with OSA regularly using CPAP therapy. [72] Thus, evidence suggests that effective treatment of OSA should decrease accident rates.
Despite the elevated risk of crashing, most patients with OSA have not had a crash; therefore, determining which OSA patients are likely to have an accident, which patients should have driving restrictions, and how much benefit would accrue from these restrictions is not clear. [73]
No recent evidence-based guidelines are available regarding driving for the average patient with OSA. The most recent statement on this topic is from 1994. [74]
One approach to this problem outlined in the 1994 statement is the concept of shared responsibilities. Educating the patient about the risks of driving while sleepy or inattentive is the physician’s responsibility. One suggestion is that the patient acknowledges this education by signing a statement to that effect. After receiving proper education, the patient’s responsibilities are to avoid driving while sleepy and, preferably, to refrain from driving until starting treatment for OSA.
Physicians should be referred to their individual state or country motor vehicle departments for local guidelines.
Patient Education
All patients should receive education about sleep and proper sleep hygiene, OSA, and the risks of driving while sleepy. They also should receive education regarding the role of nasal CPAP and the importance of daily use, as well as training in the use of CPAP, from a physician, trained technician, or nurse for at least the first month of therapy. This training promotes long-term adherence with treatment.
For more information, see the Ear, Nose, and Throat Center; Mental Health and Behavior Center; and Sleep Disorders Center, as well as Snoring, Fatigue, Insomnia, Sleep Disorders in Women, and Sleep Disorders and Aging.
-
Sleep-related disordered breathing continuum ranging from simple snoring to obstructive sleep apnea (OSA). Upper airway resistance syndrome (UARS) occupies an intermediate position between these extremes. Note areas of overlap among the conditions.
-
In this polysomnogram summary graph, obstructive sleep apnea (OSA) severity and the degree of oxygen desaturation (SpO2%) worsen in rapid eye movement (REM) sleep (the black underlined sections) compared with non-REM sleep. This is often the case in OSA patients, especially in OSA patients with comorbid lung disease.
-
MRI rendering of a patient without obstructive sleep apnea (OSA) (left panel) and a patient with OSA (right panel).
-
Top image is 3-dimensional surface renderings of the upper airway demonstrating the effect of progressive increases in continuous positive airway pressure (CPAP) from 0-15 cm of water on upper-airway volume in a patient with upper airway narrowing. CPAP significantly increases airway volume in the retropalatal (RP) and retroglossal (RG) regions. Bottom image is soft tissue images in the same patient in the RP region at analogous levels of CPAP. With increasing CPAP, the upper airway progressively enlarges, particularly in the lateral dimension. Note the progressive thinning of the lateral pharyngeal walls as the level of CPAP increases. Little movement occurs in the parapharyngeal fat pads, the white structures lateral to the airway. The first image in each series depicts the baseline upper airway narrowing present in this patient.
-
Potential relationship between obstructive sleep apnea-hypopnea syndrome (OSAHS) and the metabolic syndrome. OSAHS has been associated with 3 of the 5 major clinical abnormalities associated with the metabolic syndrome, which is hypertension, insulin resistance, and proinflammatory/oxidative stress. OSAHS may be contributing to and/or modulating the severity of these metabolic abnormalities.
-
The Mallampati Classification is illustrated. The airway class is based on this visual heuristic.
-
Tonsil grades.
-
Obstructive sleep apnea. Note the absence of flow (red arrow) despite paradoxical respiratory effort (green arrow).
-
Central sleep apnea (thick areas). Note the absence of both flow and respiratory effort (green double arrows).
-
Comparison of a central apnea (box) and obstructive apnea (circle).
-
Mixed sleep apnea. Note that the apnea (orange arrow) begins as a central apnea (effort absent; red double arrow) and ends as an obstructive apnea (effort present; green double arrow). Note the arousal (blue arrow) that terminates the apnea and the desaturation (purple arrow) that follows.
-
A 2-minute recording of sleep showing 4 hypopneas (thick arrows) and associated oxygen desaturations (red arrows). This recording illustrates the recurrent nature of the sleep-disordered breathing observed in many patients.
-
Effect of nasal continuous positive airway pressure (CPAP) on oxygen saturation in sleep apnea. The upper portion of this figure shows the raw oxygen saturation trace from 1 night of a sleep study. Below the raw trace are vertical lines that indicate the presence of either an apnea or hypopnea. Before CPAP, frequent respiratory events with significant desaturations occurred. During the night, CPAP was applied, resulting in the elimination of the apnea and hypopneas and normalization of the oxygen trace.
-
Examples of good (upper panel) and poor (lower panel) compliance. In the upper panel, the patient is using continuous positive airway pressure (CPAP) most nights and generally for more than 4 hours (solid black line). In the lower panel, the patient is using CPAP infrequently and, when used, is wearing the CPAP device for less than 4 hours.
-
Approach to a patient with excessive daytime sleepiness after treatment with nasal continuous positive airway pressure.