Practice Essentials
Arteriovenous malformations (AVMs) are congenital lesions composed of a complex tangle of arteries and veins connected by one or more fistulae (see the image below). They most commonly occur in young adults, with morbidity and death occurring in 30–50% and 10–15% of patients, respectively. [1]
Signs and symptoms
History
Considerations regarding patient history include the following:
-
AVMs tend to be clinically silent until the presenting event occurs; therefore, the diagnosis usually is made at the time of the first seizure or hemorrhage
-
A history of minor learning disability is found in as many as two thirds of patients; such dysfunction is rarely apparent in adult life
-
A history of headaches is found in as many as half of all patients with cerebral AVM; the headaches subsequently may take the form of classic migraine or more generalized headache
-
If seizures have occurred, a careful seizure history should be obtained; seizures are simple, partial, or secondarily generalized
Physical examination
Considerations regarding the physical examination of patients with AVM include the following:
-
Focal neurologic findings are rare in the absence of seizure or hemorrhage in patients with cerebral AVMs; they are more common in AVMs that are deeply located or in the brainstem
-
Detailed neuropsychological testing may disclose subtle right or left hemisphere dysfunction
-
If parenchymal hemorrhage is present, the physical findings are indistinguishable from those produced by intracranial hemorrhage from other causes
-
Intraventricular hemorrhage generally produces a less severe neurologic deficit than does hemorrhage into other areas of the brain
-
In the rare patients in whom focal neurologic deficits are present, the deficit may reflect the location of the AVM
See Clinical Presentation for more detail.
Diagnosis
The following imaging studies are used in the diagnosis and assessment of cerebral AVM:
-
Computed tomography (CT) scanning: Easily identifies intracerebral hemorrhages, raising suspicion of AVM in a younger person or a patient without clear risk factors for hemorrhage; however, this modality can identify only large AVMs.
-
Magnetic resonance imaging (MRI): Essential for the initial diagnosis of AVMs; the malformations appear as irregular or globoid masses anywhere within the hemispheres or brainstem; a retrospective analysis demonstrated that silent intralesional microhemorrhage on CT scan/MRI may be a risk factor for intracerebral hemorrhage from a brain AVM rupture [2]
-
Cerebral angiography: Required for hemodynamic assessment, which is essential for planning treatment
-
Superselective angiography: Performed with standard cerebral angiography, with access via a femoral artery puncture
See Workup for more detail.
Management
Invasive treatment is recommended for younger patients with 1 or more high-risk features for an AVM rupture. Older individuals and patients with no high-risk features may be best treated through management of the medical aspects of the illness alone; in such patients, anticonvulsants for seizure control and appropriate analgesia for headaches may be the only treatment recommendations necessary.
Invasive treatment of AVMs may include endovascular embolization, surgical resection, and focal beam radiation, alone or in any combination. The current American Heart Association multidisciplinary management guidelines for the treatment of brain AVMs recommend the following approach: [3]
-
Surgical extirpation is strongly suggested as the primary treatment for AVMs of Spetzler-Martin grade I or II if they are surgically accessible with low risk
-
Radiation therapy alone is recommended for AVMs of Spetzler-Martin grade I or II if they are less than 3 cm in size and surgery has an increased surgical risk based on location and vascular anatomy
-
Brain AVMs of Spetzler-Martin grade III can often be treated with a multimodal approach that uses embolization followed by surgical extirpation. If the lesion has a high surgical risk based on location and vascular anatomy, radiation therapy may be performed after embolization
-
AVMs of Spetzler-Martin grade IV or V are often not amenable to surgical treatment alone because of the high procedural risk; these AVMs can be treated using a combined multimodal approach that includes embolization, radiosurgery, and/or surgery
-
In general, embolization should be performed only if the goal is complete AVM eradication with other treatment modalities; the only exception is palliative embolization in patients with an AVM of Spetzler-Martin grade IV or V with venous outflow obstruction or true steal phenomenon, in order to reduce arterial inflow to control edema or to reduce the amount of shunt, respectively
See Treatment for more detail.
Background
Arteriovenous malformations (AVMs) are congenital lesions composed of a complex tangle of arteries and veins connected by one or more fistulae. They most commonly occur in young adults, with morbidity and death occurring in 30–50% and 10–15% of patients, respectively. [1] Hemorrhage from cerebral (AVMs) represents 2% of all hemorrhagic strokes. A clear understanding of the diagnostic and treatment algorithms involved with AVM management is imperative, because AVMs are a cause of hemorrhage in young adults.
Pathophysiology
Arteriovenous malformations (AVMs) are congenital lesions composed of a complex tangle of arteries and veins connected by one or more fistulae. The vascular conglomerate is called the nidus. The nidus has no capillary bed, and the feeding arteries drain directly to the draining veins. [4] The arteries have a deficient muscularis layer. The draining veins often are dilated owing to the high velocity of blood flow through the fistulae. How the abnormal vessels appear or exactly when the process begins is unknown. Deranged production of vasoactive proteins is under investigation as the angiogenetic link to pathophysiology.
AVMs produce neurological dysfunction through 3 main mechanisms. [5] First, hemorrhage may occur in the subarachnoid space, the intraventricular space or, most commonly, the brain parenchyma. Second, in the absence of hemorrhage, seizures may occur as a consequence of AVM: approximately 15-40% of patients present with seizure disorder. Finally, but rarely, a progressive neurological deficit may occur in 6-12% of patients over a few months to several years. These slowly progressive neurological deficits are thought to relate to siphoning of blood flow away from adjacent brain tissue (the "steal phenomenon"), a concept that has been recently challenged. Neurological deficits may be explained alternatively by the mass effect of an enlarging AVM or venous hypertension in the draining veins.
Epidemiology
Frequency
United States
The detection rate in the general population based on prospective data from the New York Islands AVM Study is approximately 1.34 per 100,000 person-years. [6] The prevalence of cerebral arteriovenous malformations (AVMs) in the United States is not known. Given the low threshold for MRI neuroimaging, many patients' conditions are now discovered before they experience a brain hemorrhage. [5]
International
Reported detection rates range between 0.89 and 1.24 per 100,000 person-years according to reports from Australia, Sweden, and Scotland. The prevalence of cerebral AVMs in Scotland has been estimated to be 18 per 100,000 person-years.
Mortality/Morbidity
Although 300,000 persons in the United States may harbor AVMs, only 12% of AVMs are estimated to become symptomatic. Death occurs in 10–15% of patients who have hemorrhage, and morbidity of various degrees occurs in approximately 30–50%.
-
Hemorrhage: In population-based studies, 38–70% of brain AVMs present initially with hemorrhages. The overall risk of intracranial hemorrhage in patients with known AVM is 2–4% per year. Patients presenting with a hemorrhage are at increased risk for rebleeding, particularly during the first year after the initial hemorrhage (recurrent hemorrhage rate within 12 months after initial hemorrhage: patients with hemorrhagic presentation 7–33%; patients with nonhemorrhagic presentation 0–3%). [7, 8] Hemorrhage rates progressively converge with time for both patients groups after 1 year. [8] Clinical and angiographic features associated with the risk for hemorrhagic presentation are male gender, small AVM size, location in the basal ganglia or posterior fossa, deep venous drainage, single or only few draining veins, high pressure in the feeding arteries as measured during angiography, and intranidal and flow-related feeding artery aneurysms.
-
Although the initial presentation of a cerebral hemorrhage may be indistinguishable from those of other causes of hemorrhage, the neurological deficit in AVM-related hemorrhage tends to be less severe compared with a non–AVM-related hemorrhage. Recovery of AVM-related hemorrhage tends to be better, partly because of the relatively younger age of patients with AVM and partly because of functional cerebral reorganization in patients with cerebral AVMs.
-
Seizures and epilepsy: Seizures unrelated to hemorrhage occur as the presenting symptom in 15-40% of patients with brain AVM. These may be focal or become secondarily generalized. Satisfactory treatment of seizures is usually possible with standard anticonvulsants. Presentation with seizures is associated with young age, large AVM size, lobar location (especially temporal lobe), and feeders mainly from the middle cerebral artery. Patients with brain ruptured AVM, especially if it is of cortical or subarachnoid location, are at increased risk to develop seizures and epilepsy similar to patients with this type of hemorrhages of other causes unrelated to brain AVM.
-
Headache and migraine: In the general population, headache due to a brain AVM is an extremely uncommon cause. Headache unrelated to hemorrhage occurs in 4–14% of patients with AVM and may be the presenting symptom. The headache may be typical for migraine or may be present with a less specific complaint of more generalized head pain.
Age
Despite the presumed congenital origin of AVMs, the clinical presentation most commonly occurs in young adults.
AVM hemorrhage or seizure as an incident event may occur in young children or adults older than 40 years; however, childhood migraine is common.
A history of subtle learning disorder is elicited in 66% of adults with AVMs. This suggests early effects that are largely subclinical and do not come to medical attention.
Prognosis
With an overall risk of intracerebral hemorrhage of 2-4% per year, angiographic assessment is recommended to further define prognosis for patients with arteriovenous malformations (AVMs).
Those with superficial, moderate-sized AVMs have a good long-term prognosis and may not have any additional benefit with interventional treatment.
Lifetime risk of hemorrhage may be substantial for young patients with AVM.
Prognosis after AVM hemorrhage is generally better than that after intracerebral hemorrhage from other causes. Better prognosis may be due to the relatively younger age of patients and a greater potential for reorganization of brain function. More accurate prognosis awaits the results of currently active, long-term, population-based outcome studies.
-
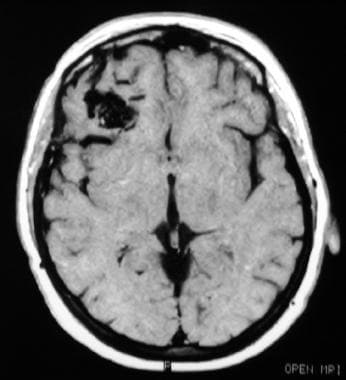
Axial T2 MRI showing an arteriovenous malformation with hemorrhage, in the territory of the left posterior cerebral artery.
-
T1 axial MRI showing a small subcortical arteriovenous malformation in the right frontal lobe.
-
T2 coronal MRI showing an arteriovenous malformation in the left medial temporal lobe.
-
Magnetic resonance angiography showing a left medial temporal arteriovenous malformation.
-
Angiogram (anteroposterior view) showing an arteriovenous malformation in the deep left middle cerebral artery territory measuring approximately 3 cm in diameter, with a deep draining vein (arrow).