Rates of TBI-related Emergency Department Visits, Hospitalizations, and Deaths--United States, 2001-2010. Centers for Disease Control and Prevention. Available at http://www.cdc.gov/traumaticbraininjury/data/rates.html. Accessed: September 11, 2016.
Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, and Deaths - United States, 2007 and 2013. MMWR Surveill Summ. 2017 Mar 17. 66 (9):1-16. [QxMD MEDLINE Link].
Wu AP, Davidson T. Posttraumatic anosmia secondary to central nervous system injury. Am J Rhinol. Nov-Dec/2008. 22:606-7.
Bhatoe HS. Primary brainstem injury: benign course and improved survival. Acta Neurochir (Wien). 1999. 141(5):515-9. [QxMD MEDLINE Link].
Munjal SK, Panda NK, Pathak A. Dynamics of Hearing Status in Closed Head Injury. J Neurotrauma. Feb/2010. 27:309-316.
Mackay LE, Morgan AS, Bernstein BA. Factors affecting oral feeding with severe traumatic brain injury. J Head Trauma Rehabil. 1999 Oct. 14(5):435-47. [QxMD MEDLINE Link].
Ellenberg JH, Levin HS, Saydjari C. Posttraumatic Amnesia as a predictor of outcome after severe closed head injury. Prospective assessment. Arch Neurol. 1996 Aug. 53(8):782-91. [QxMD MEDLINE Link].
Crevits L, Hanse MC, Tummers P, et al. Antisaccades and remembered saccades in mild traumatic brain injury. J Neurol. 2000 Mar. 247(3):179-82. [QxMD MEDLINE Link].
Tisdall M, Crocker M, Watkiss J, Smith M. Disturbances of sodium in critically ill adult neurologic patients: a clinical review. J Neurosurg Anesthesiol. 2006 Jan. 18(1):57-63. [QxMD MEDLINE Link].
Olivecrona M, Koskinen LD. Comment on: Early CSF and serum S 100B concentrations for outcome prediction in traumatic brain injury and subarachoid haemorrhage. Clin Neurol Neurosurg. 2016 Aug 20. [QxMD MEDLINE Link].
Herrmann M, Curio N, Jost S, et al. Release of biochemical markers of damage to neuronal and glial brain tissue is associated with short and long term neuropsychological outcome after traumatic brain injury. J Neurol Neurosurg Psychiatry. 2001 Jan. 70(1):95-100. [QxMD MEDLINE Link].
Voelker R. Taking a Closer Look at the Biomarker Test for Mild Traumatic Brain Injury. JAMA. 2018 May 22. 319 (20):2066-2067. [QxMD MEDLINE Link].
Roberts I. Barbiturates for acute traumatic brain injury. Cochrane Database Syst Rev. 2000. CD000033. [QxMD MEDLINE Link].
Stein SC. Minor head injury: 13 is an unlucky number. J Trauma. 2001 Apr. 50(4):759-60. [QxMD MEDLINE Link].
Matsuyama T, Shimomura T, Okumura Y, et al. Acute subdural hematomas due to rupture of cortical arteries: a study of the points of rupture in 19 cases. Surg Neurol. 1997 May. 47(5):423-7. [QxMD MEDLINE Link].
Eisenberg HM, Gary HE Jr, Aldrich EF, et al. Initial CT findings in 753 patients with severe head injury. A report from the NIH Traumatic Coma Data Bank. J Neurosurg. 1990 Nov. 73(5):688-98. [QxMD MEDLINE Link].
Maxwell WL, MacKinnon MA, Smith DH, et al. Thalamic nuclei after human blunt head injury. J Neuropathol Exp Neurol. 2006 May. 65(5):478-88. [QxMD MEDLINE Link].
Blumbergs PC, Scott G, Manavis J, et al. Topography of axonal injury as defined by amyloid precursor protein and the sector scoring method in mild and severe closed head injury. J Neurotrauma. 1995 Aug. 12(4):565-72. [QxMD MEDLINE Link].
Jennett B, Adams JH, Murray LS, et al. Neuropathology in vegetative and severely disabled patients after head injury. Neurology. 2001 Feb 27. 56(4):486-90. [QxMD MEDLINE Link].
Markianos M, Seretis A, Kotsou S, et al. CSF neurotransmitter metabolites and short-term outcome of patients in coma after head injury. Acta Neurol Scand. 1992 Aug. 86(2):190-3. [QxMD MEDLINE Link].
Bullock R, Zauner A, Woodward JJ, et al. Factors affecting excitatory amino acid release following severe human head injury. J Neurosurg. 1998 Oct. 89(4):507-18. [QxMD MEDLINE Link].
DeGraba TJ, Pettigrew LC. Why do neuroprotective drugs work in animals but not humans?. Neurol Clin. 2000 May. 18(2):475-93. [QxMD MEDLINE Link].
Jonas W, Lin Y, Tortella F. Neuroprotection from glutamate toxicity with ultra-low dose glutamate. Neuroreport. 2001 Feb 12,. 12(2):335-9. [QxMD MEDLINE Link].
Yang SY, Gao ZX. Determination and clinical significance of plasma levels of prostaglandins in patients with acute brain injury. Surg Neurol. 1999 Sep. 52(3):238-45. [QxMD MEDLINE Link].
Zubkov AY, Lewis AI, Raila FA, et al. Risk factors for the development of post-traumatic cerebral vasospasm. Surg Neurol. 2000 Feb. 53(2):126-30. [QxMD MEDLINE Link].
Al-Mufti F, Amuluru K, Changa A, Lander M, Patel N, Wajswol E, et al. Traumatic brain injury and intracranial hemorrhage-induced cerebral vasospasm: a systematic review. Neurosurg Focus. 2017 Nov. 43 (5):E14. [QxMD MEDLINE Link].
Fiandaca MS, Mapstone M, Mahmoodi A, Gross T, Macciardi F, Cheema AK, et al. Plasma metabolomic biomarkers accurately classify acute mild traumatic brain injury from controls. PLoS One. 2018. 13 (4):e0195318. [QxMD MEDLINE Link].
Kumar RG, Diamond ML, Boles JA, Berger RP, Tisherman SA, Kochanek PM, et al. Acute CSF interleukin-6 trajectories after TBI: associations with neuroinflammation, polytrauma, and outcome. Brain Behav Immun. 2015 Mar. 45:253-62. [QxMD MEDLINE Link].
Russo MV, McGavern DB. Inflammatory neuroprotection following traumatic brain injury. Science. 2016 Aug 19. 353 (6301):783-5. [QxMD MEDLINE Link].
Nwachuku EL, Puccio AM, Adeboye A, Chang YF, Kim J, Okonkwo DO. Time course of cerebrospinal fluid inflammatory biomarkers and relationship to 6-month neurologic outcome in adult severe traumatic brain injury. Clin Neurol Neurosurg. 2016 Oct. 149:1-5. [QxMD MEDLINE Link].
Plesnila N, von Baumgarten L, Retiounskaia M, Engel D, Ardeshiri A, Zimmermann R, et al. Delayed neuronal death after brain trauma involves p53-dependent inhibition of NF-kappaB transcriptional activity. Cell Death Differ. 2007 Aug. 14(8):1529-41. [QxMD MEDLINE Link].
Cho YE, Latour LL, Kim H, Turtzo LC, Olivera A, Livingston WS, et al. Older Age Results in Differential Gene Expression after Mild Traumatic Brain Injury and Is Linked to Imaging Differences at Acute Follow-up. Front Aging Neurosci. 2016. 8:168. [QxMD MEDLINE Link].
Wang HE, Peitzman AB, Cassidy LD, et al. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med. 2004 Nov. 44(5):439-50. [QxMD MEDLINE Link].
Haltmeier T, Schnüriger B, Benjamin E, Brodmann Maeder M, Künzler M, Siboni S, et al. Isolated blunt severe traumatic brain injury in Bern, Switzerland, and the United States: A matched cohort study. J Trauma Acute Care Surg. 2016 Feb. 80 (2):296-301. [QxMD MEDLINE Link].
Lannoo E, Van Rietvelde F, Colardyn F, et al. Early predictors of mortality and morbidity after severe closed head injury. J Neurotrauma. 2000 May. 17(5):403-14. [QxMD MEDLINE Link].
Salim A, Hadjizacharia P, DuBose J, Brown C, Inaba K, Chan L. Role of anemia in traumatic brain injury. J Am Coll Surg. 2008 Sep. 207(3):398-406. [QxMD MEDLINE Link].
Robertson CS, Hannay HJ, Yamal JM, et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: a randomized clinical trial. JAMA. 2014 Jul 2. 312 (1):36-47. [QxMD MEDLINE Link].
Tian HL, Geng Z, Cui YH, Hu J, Xu T, Cao HL. Risk factors for posttraumatic cerebral infarction in patients with moderate or severe head trauma. Neurosurg Rev. 2008 Oct. 31(4):431-6; discussion 436-7. [QxMD MEDLINE Link].
Rutland-Brown W, Langlois JA, Thomas KE, Xi YL. Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006 Nov-Dec. 21(6):544-8. [QxMD MEDLINE Link].
Büchele G, Rapp K, König HH, Jaensch A, Rothenbacher D, Becker C, et al. The Risk of Hospital Admission Due to Traumatic Brain Injury Is Increased in Older Persons With Severe Functional Limitations. J Am Med Dir Assoc. 2016 Jul 1. 17 (7):609-12. [QxMD MEDLINE Link].
Fu TS, Jing R, McFaull SR, Cusimano MD. Recent trends in hospitalization and in-hospital mortality associated with traumatic brain injury in Canada: A nationwide, population-based study. J Trauma Acute Care Surg. 2015 Sep. 79 (3):449-54. [QxMD MEDLINE Link].
Peeters W, van den Brande R, Polinder S, Brazinova A, Steyerberg EW, Lingsma HF, et al. Epidemiology of traumatic brain injury in Europe. Acta Neurochir (Wien). 2015 Oct. 157 (10):1683-96. [QxMD MEDLINE Link].
Thurman D, Guerrero J. Trends in hospitalization associated with traumatic brain injury. JAMA. 1999 Sep 8. 282(10):954-7. [QxMD MEDLINE Link].
Cassidy JD, Carroll LJ, Peloso PM, Borg J, von Holst H, Holm L. Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004 Feb. (43 Suppl):28-60. [QxMD MEDLINE Link].
Dewan MC, Rattani A, Gupta S, Baticulon RE, Hung YC, Punchak M, et al. Estimating the global incidence of traumatic brain injury. J Neurosurg. 2018 Apr 27. 1-18. [QxMD MEDLINE Link].
Wagner AK, Sasser HC, Hammond FM, et al. Intentional traumatic brain injury: epidemiology, risk factors, and associations with injury severity and mortality. J Trauma. 2000 Sep. 49(3):404-10. [QxMD MEDLINE Link].
Haider AH, Efron DT, Haut ER, DiRusso SM, Sullivan T, Cornwell EE 3rd. Black children experience worse clinical and functional outcomes after traumatic brain injury: an analysis of the National Pediatric Trauma Registry. J Trauma. 2007 May. 62(5):1259-62; discussion 1262-3. [QxMD MEDLINE Link].
Albrecht JS, Hirshon JM, McCunn M, Bechtold KT, Rao V, Simoni-Wastila L, et al. Increased Rates of Mild Traumatic Brain Injury Among Older Adults in US Emergency Departments, 2009-2010. J Head Trauma Rehabil. 2016 Sep-Oct. 31 (5):E1-7. [QxMD MEDLINE Link].
Lau BC, Kontos AP, Collins MW, Mucha A, Lovell MR. Which On-field Signs/Symptoms Predict Protracted Recovery From Sport-Related Concussion Among High School Football Players?. Am J Sports Med. 2011 Nov. 39(11):2311-8. [QxMD MEDLINE Link].
Bernal-Sprekelsen M, Bleda-Vazquez C, Carrau RL. Ascending meningitis secondary to traumatic cerebrospinal fluid leaks. Am J Rhinol. 2000 Jul-Aug. 14(4):257-9. [QxMD MEDLINE Link].
Tien HC, Cunha JR, Wu SN, et al. Do trauma patients with a Glasgow Coma Scale score of 3 and bilateral fixed and dilated pupils have any chance of survival?. J Trauma. 2006 Feb. 60(2):274-8. [QxMD MEDLINE Link].
Mauritz W, Leitgeb J, Wilbacher I, et al. Outcome of brain trauma patients who have a Glasgow Coma Scale score of 3 and bilateral fixed and dilated pupils in the field. European Journal of Emergency Medicine. 2009. 16:153-158.
Krauss JK, Trankle R, Kopp KH. Post-traumatic movement disorders in survivors of severe head injury. Neurology. 1996 Dec. 47(6):1488-92. [QxMD MEDLINE Link].
Matser JT, Kessels AG, Jordan BD, et al. Chronic traumatic brain injury in professional soccer players. Neurology. 1998 Sep. 51(3):791-6. [QxMD MEDLINE Link].
Lobato RD, Rivas JJ, Gomez PA, et al. Head-injured patients who talk and deteriorate into coma. Analysis of 211 cases studied with computerized tomography. J Neurosurg. 1991 Aug. 75(2):256-61. [QxMD MEDLINE Link].
Stuss DT, Binns MA, Carruth FG, et al. The acute period of recovery from traumatic brain injury: posttraumatic amnesia or posttraumatic confusional state?. J Neurosurg. 1999 Apr. 90(4):635-43. [QxMD MEDLINE Link].
Leininger BE, Gramling SE, Farrell AD, et al. Neuropsychological deficits in symptomatic minor head injury patients after concussion and mild concussion. J Neurol Neurosurg Psychiatry. 1990 Apr. 53(4):293-6. [QxMD MEDLINE Link].
Ruffolo LF, Guilmette TJ, Willis GW. Comparison of time and error rates on the trail making test among patients with head injuries, experimental malingerers, patients with suspect effort on testing, and normal controls. Clin Neuropsychol. 2000 May. 14(2):223-30. [QxMD MEDLINE Link].
Hefny AF, Eid HO, Abu-Zidan FM. Severe tyre blast injuries during servicing. Injury. 2009 May. 40(5):484-7. [QxMD MEDLINE Link].
Bhattacharjee Y. Neuroscience. Shell shock revisited: solving the puzzle of blast trauma. Science. 2008 Jan 25. 319(5862):406-8. [QxMD MEDLINE Link].
Belanger HG, Kretzmer T, Yoash-Gantz R, Pickett T, Tupler LA. Cognitive sequelae of blast-related versus other mechanisms of brain trauma. J Int Neuropsychol Soc. 2009 Jan. 15(1):1-8. [QxMD MEDLINE Link].
Reymond MA, Marbet G, Radu EW, et al. Aspirin as a risk factor for hemorrhage in patients with head injuries. Neurosurg Rev. 1992. 15(1):21-5. [QxMD MEDLINE Link].
Wong DK, Lurie F, Wong LL. The effects of clopidogrel on elderly traumatic brain injured patients. J Trauma. Dec/2008. 65:1303-8.
Feeney JM, Santone E, DiFiori M, Kis L, Jayaraman V, Montgomery SC. Compared to warfarin, direct oral anticoagulants are associated with lower mortality in patients with blunt traumatic intracranial hemorrhage: A TQIP study. J Trauma Acute Care Surg. 2016 Sep 3. [QxMD MEDLINE Link].
Uccella L, Zoia C, Bongetta D, Gaetani P, Martig F, Candrian C, et al. Are Antiplatelet and Anticoagulants Drugs A Risk Factor for Bleeding in Mild Traumatic Brain Injury?. World Neurosurg. 2018 Feb. 110:e339-e345. [QxMD MEDLINE Link].
O'Phelan K, McArthur DL, Chang CW, Green D, Hovda DA. The impact of substance abuse on mortality in patients with severe traumatic brain injury. J Trauma. 2008 Sep. 65(3):674-7. [QxMD MEDLINE Link].
Talving P, Plurad D, Barmparas G, et al. Isolated severe traumatic brain injuries: association of blood alcohol levels with the severity of injuries and outcomes. J Trauma. Feb/2010. 68:357-62.
Friedman G, Froom P, Sazbon L, et al. Apolipoprotein E-epsilon4 genotype predicts a poor outcome in survivors of traumatic brain injury. Neurology. 1999 Jan 15. 52(2):244-8. [QxMD MEDLINE Link].
Kutner KC, Erlanger DM, Tsai J, et al. Lower cognitive performance of older football players possessing apolipoprotein E epsilon4. Neurosurgery. 2000 Sep. 47(3):651-7; discussion 657-8. [QxMD MEDLINE Link].
Yue JK, Robinson CK, Burke JF, et al. Apolipoprotein E epsilon 4 (APOE-ε4) genotype is associated with decreased 6-month verbal memory performance after mild traumatic brain injury. Brain Behav. 2017 Sep. 7 (9):e00791. [QxMD MEDLINE Link].
Zhou W, Xu D, Peng X, Zhang Q, Jia J, Crutcher KA. Meta-analysis of APOE4 allele and outcome after traumatic brain injury. J Neurotrauma. 2008 Apr. 25(4):279-90. [QxMD MEDLINE Link].
Li L, Bao Y, He S, Wang G, Guan Y, Ma D, et al. The Association Between Apolipoprotein E and Functional Outcome After Traumatic Brain Injury: A Meta-Analysis. Medicine (Baltimore). 2015 Nov. 94 (46):e2028. [QxMD MEDLINE Link].
Jordan BD. Genetic influences on outcome following traumatic brain injury. Neurochem Res. 2007 Apr-May. 32(4-5):905-15. [QxMD MEDLINE Link].
Shee K, Lucas A, Flashman LA, Nho K, Tsongalis GJ, McDonald BC, et al. Alpha-synuclein (SNCA) polymorphisms exert protective effects on memory after mild traumatic brain injury. Neurosci Lett. 2016 Sep 6. 630:241-6. [QxMD MEDLINE Link].
Terrell TR, Abramson R, Barth JT, Bennett E, Cantu RC, Sloane R, et al. Genetic polymorphisms associated with the risk of concussion in 1056 college athletes: a multicentre prospective cohort study. Br J Sports Med. 2018 Feb. 52 (3):192-198. [QxMD MEDLINE Link].
Bacic A, Gluncic I, Gluncic V. Disturbances in plasma sodium in patients with war head injuries. Mil Med. 1999 Mar. 164(3):214-7. [QxMD MEDLINE Link].
Leonard J, Garrett RE, Salottolo K, Slone DS, Mains CW, Carrick MM, et al. Cerebral salt wasting after traumatic brain injury: a review of the literature. Scand J Trauma Resusc Emerg Med. 2015 Nov 11. 23:98. [QxMD MEDLINE Link].
Bareyre FM, Saatman KE, Raghupathi R, McIntosh TK. Postinjury treatment with magnesium chloride attenuates cortical damage after traumatic brain injury in rats. J Neurotrauma. 2000 Nov. 17(11):1029-39. [QxMD MEDLINE Link].
Halpern CH, Reilly PM, Turtz AR, Stein SC. Traumatic coagulopathy: the effect of brain injury. J Neurotrauma. 2008 Aug. 25(8):997-1001. [QxMD MEDLINE Link].
Stalnacke BM, Tegner Y, Sojka P. Playing soccer increases serum concentrations of the biochemical markers of brain damage S-100B and neuron-specific enolase in elite players: a pilot study. Brain Inj. 2004 Sep. 18(9):899-909. [QxMD MEDLINE Link].
Straume-Naesheim TM, Andersen TE, Jochum M, et al. Minor head trauma in soccer and serum levels of S100B. Neurosurgery. Jun/2008. 62:1297-305.
Mercier E, Tardif PA, Cameron PA, Émond M, Moore L, Mitra B, et al. Prognostic value of neuron-specific enolase (NSE) for prediction of post-concussion symptoms following a mild traumatic brain injury: a systematic review. Brain Inj. 2018. 32 (1):29-40. [QxMD MEDLINE Link].
Shahim P, Tegner Y, Marklund N, Blennow K, Zetterberg H. Neurofilament light and tau as blood biomarkers for sports-related concussion. Neurology. 2018 May 15. 90 (20):e1780-e1788. [QxMD MEDLINE Link].
Metting Z, Wilczak N, Rodiger LA, Schaaf JM, van der Naalt J. GFAP and S100B in the acute phase of mild traumatic brain injury. Neurology. 2012 May 1. 78(18):1428-33. [QxMD MEDLINE Link].
Lagerstedt L, Egea-Guerrero JJ, Bustamante A, Rodríguez-Rodríguez A, El Rahal A, Quintana-Diaz M, et al. Combining H-FABP and GFAP increases the capacity to differentiate between CT-positive and CT-negative patients with mild traumatic brain injury. PLoS One. 2018. 13 (7):e0200394. [QxMD MEDLINE Link].
Haydel MJ, Preston CA, Mills TJ, et al. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000 Jul 13. 343(2):100-5. [QxMD MEDLINE Link].
Smits M, Dippel DW, Steyerberg EW, de Haan GG, Dekker HM, Vos PE. Predicting intracranial traumatic findings on computed tomography in patients with minor head injury: the CHIP prediction rule. Ann Intern Med. 2007 Mar 20. 146(6):397-405. [QxMD MEDLINE Link].
Timler D, Dworzyński MJ, Szarpak Ł, Gaszyńska E, Dudek K, Gałązkowski R. Head Trauma in Elderly Patients: Mechanisms of Injuries and CT Findings. Adv Clin Exp Med. 2015 Nov-Dec. 24 (6):1045-50. [QxMD MEDLINE Link].
Wang MC, Linnau KF, Tirschwell DL, Hollingworth W. Utility of repeat head computed tomography after blunt head trauma: a systematic review. J Trauma. 2006 Jul. 61(1):226-33. [QxMD MEDLINE Link].
Smith-Bindman R, McCulloch CE, Ding A, Quale C, Chu PW. Diagnostic imaging rates for head injury in the ED and states' medical malpractice tort reforms. Am J Emerg Med. 2011 Jul. 29(6):656-64. [QxMD MEDLINE Link].
Levin HS, Williams DH, Valastro M, et al. Corpus callosal atrophy following closed head injury: detection with magnetic resonance imaging. J Neurosurg. 1990 Jul. 73(1):77-81. [QxMD MEDLINE Link].
Pierallini A, Pantano P, Fantozzi LM, et al. Correlation between MRI findings and long-term outcome in patients with severe brain trauma. Neuroradiology. 2000 Dec. 42(12):860-7. [QxMD MEDLINE Link].
Rutgers DR, Toulgoat F, Cazejust J, Fillard P, Lasjaunias P, Ducreux D. White matter abnormalities in mild traumatic brain injury: a diffusion tensor imaging study. AJNR Am J Neuroradiol. 2008 Mar. 29(3):514-9. [QxMD MEDLINE Link].
Niogi SN, Mukherjee P, Ghajar J, Johnson C, Kolster RA, Sarkar R. Extent of microstructural white matter injury in postconcussive syndrome correlates with impaired cognitive reaction time: a 3T diffusion tensor imaging study of mild traumatic brain injury. AJNR Am J Neuroradiol. 2008 May. 29(5):967-73. [QxMD MEDLINE Link].
Dailey NS, Smith R, Bajaj S, Alkozei A, Gottschlich MK, Raikes AC, et al. Elevated Aggression and Reduced White Matter Integrity in Mild Traumatic Brain Injury: A DTI Study. Front Behav Neurosci. 2018. 12:118. [QxMD MEDLINE Link].
Sener S, Van Hecke W, Feyen BF, Van der Steen G, Pullens P, Van de Hauwe L, et al. Diffusion Tensor Imaging: A Possible Biomarker in Severe Traumatic Brain Injury and Aneurysmal Subarachnoid Hemorrhage?. Neurosurgery. 2016 Jun 27. [QxMD MEDLINE Link].
Fontaine A, Azouvi P, Remy P, et al. Functional anatomy of neuropsychological deficits after severe traumatic brain injury. Neurology. 1999 Dec 10. 53(9):1963-8. [QxMD MEDLINE Link].
Gowda NK, Agrawal D, Bal C, et al. Technetium Tc-99m ethyl cysteinate dimer brain single-photon emission CT in mild traumatic brain injury: a prospective study. AJNR Am J Neuroradiol. 2006 Feb. 27(2):447-51. [QxMD MEDLINE Link].
Garnett MR, Blamire AM, Rajagopalan B, et al. Evidence for cellular damage in normal-appearing white matter correlates with injury severity in patients following traumatic brain injury: A magnetic resonance spectroscopy study. Brain. 2000 Jul. 123 ( Pt 7):1403-9. [QxMD MEDLINE Link].
Croall I, Smith FE, Blamire AM. Magnetic Resonance Spectroscopy for Traumatic Brain Injury. Top Magn Reson Imaging. 2015 Oct. 24 (5):267-74. [QxMD MEDLINE Link].
Vespa PM, Nuwer MR, Nenov V, et al. Increased incidence and impact of nonconvulsive and convulsive seizures after traumatic brain injury as detected by continuous electroencephalographic monitoring. J Neurosurg. 1999 Nov. 91(5):750-60. [QxMD MEDLINE Link].
Aquino L, Kang CY, Harada MY, Ko A, Do-Nguyen A, Ley EJ, et al. Is Routine Continuous EEG for Traumatic Brain Injury Beneficial?. Am Surg. 2017 Dec 1. 83 (12):1433-1437. [QxMD MEDLINE Link].
Steinbaugh LA, Lindsell CJ, Shutter LA, Szaflarski JP. Initial EEG predicts outcomes in a trial of levetiracetam vs. fosphenytoin for seizure prevention. Epilepsy Behav. 2012 Mar. 23(3):280-4. [QxMD MEDLINE Link].
Carter BG, Butt W. Review of the use of somatosensory evoked potentials in the prediction of outcome after severe brain injury. Crit Care Med. 2001 Jan. 29(1):178-86. [QxMD MEDLINE Link].
Hortobágyi T, Wise S, Hunt N, Cary N, Djurovic V, Fegan-Earl A. Traumatic axonal damage in the brain can be detected using beta-APP immunohistochemistry within 35 min after head injury to human adults. Neuropathol Appl Neurobiol. 2007 Apr. 33(2):226-37. [QxMD MEDLINE Link].
Dressler J, Hanisch U, Kuhlisch E, et al. Neuronal and glial apoptosis in human traumatic brain injury. Int J Legal Med. 2007. 121:365-375.
McKee AC, Cantu RC, Nowinski CJ, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. Jul/2009. 68:709-35.
Stein TD, Alvarez VE, McKee AC. Chronic traumatic encephalopathy: a spectrum of neuropathological changes following repetitive brain trauma in athletes and military personnel. Alzheimers Res Ther. 2014. 6 (1):4. [QxMD MEDLINE Link].
Shahim P, Linemann T, Inekci D, Karsdal MA, Blennow K, Tegner Y, et al. Serum Tau Fragments Predict Return to Play in Concussed Professional Ice Hockey Players. J Neurotrauma. 2016 Nov 15. 33 (22):1995-1999. [QxMD MEDLINE Link].
Berger-Pelleiter E, Émond M, Lauzier F, Shields JF, Turgeon AF. Hypertonic saline in severe traumatic brain injury: a systematic review and meta-analysis of randomized controlled trials. CJEM. 2016 Mar. 18 (2):112-20. [QxMD MEDLINE Link].
White H, Cook D, Venkatesh B. The use of hypertonic saline for treating intracranial hypertension after traumatic brain injury. Anesth Analg. 2006 Jun. 102(6):1836-46. [QxMD MEDLINE Link].
Shafi S, Diaz-Arrastia R, Madden C, Gentilello L. Intracranial pressure monitoring in brain-injured patients is associated with worsening of survival. J Trauma. 2008 Feb. 64(2):335-40. [QxMD MEDLINE Link].
Farahvar A, Gerber LM, Chiu YL, Carney N, Härtl R, Ghajar J. Increased mortality in patients with severe traumatic brain injury treated without intracranial pressure monitoring. J Neurosurg. 2012 Aug 17. [QxMD MEDLINE Link].
Rosner MJ, Rosner SD, Johnson AH. Cerebral perfusion pressure: management protocol and clinical results. J Neurosurg. 1995 Dec. 83(6):949-62. [QxMD MEDLINE Link].
White H, Venkatesh B. Cerebral perfusion pressure in neurotrauma: a review. Anesth Analg. Sep/2008. 107:979-88.
The SAFE Study Investigators. Saline or Albumin for Fluid Resuscitation in Patients with Traumatic Brain Injury. NEJM. Aug/2007. 357:874-84.
Clifton GL, Miller ER, Choi SC, et al. Lack of effect of induction of hypothermia after acute brain injury. N Engl J Med. 2001 Feb 22. 344(8):556-63. [QxMD MEDLINE Link].
Sydenham E, Roberts I, Alderson P. Hypothermia for traumatic head injury. Cochrane Database Syst Rev. Apr/2009. 15:CD001048.
Clifton GL, Valadka A, Zygun D, et al. Very early hypothermia induction in patients with severe brain injury (the National Acute Brain Injury Study: Hypothermia II): a randomised trial. Lancet Neurol. 2011 Feb. 10(2):131-9. [QxMD MEDLINE Link].
Lazaridis C, Robertson CS. Hypothermia for Increased Intracranial Pressure: Is It Dead?. Curr Neurol Neurosci Rep. 2016 Sep. 16 (9):78. [QxMD MEDLINE Link].
Härtl R, Gerber LM, Ni Q, Ghajar J. Effect of early nutrition on deaths due to severe traumatic brain injury. J Neurosurg. 2008 Jul. 109(1):50-6. [QxMD MEDLINE Link].
Reiff DA, Haricharan RN, Bullington NM, et al. Traumatic brain injury is associated with the development of deep vein thrombosis independent of pharmacologic prophylaxis. J Trauma. May/2009. 66:1436-40.
Depew AJ, Hu CK, Nguyen AC, et al. Thromboembolic prophylaxis in blunt traumatic intracranial hemorrhage: a retrospective review. Am Surg. OCt/2008. 74:906-11.
Roberts I, Yates D, Sandercock P, et al. Effect of intravenous corticosteroids on death within 14 days in 10008 adults with clinically significant head injury (MRC CRASH trial): randomised placebo-controlled trial. Lancet. 2004 Oct 9. 364(9442):1321-8. [QxMD MEDLINE Link].
Zhu C, Chen J, Pan J, Qiu Z, Xu T. Therapeutic effect of intensive glycemic control therapy in patients with traumatic brain injury: A systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2018 Jul. 97 (30):e11671. [QxMD MEDLINE Link].
Temkin NR, Dikmen SS, Wilensky AJ, et al. A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N Engl J Med. 1990 Aug 23. 323(8):497-502. [QxMD MEDLINE Link].
Kruer RM, Harris LH, Goodwin H, Kornbluth J, Thomas KP, Slater LA, et al. Changing trends in the use of seizure prophylaxis after traumatic brain injury: a shift from phenytoin to levetiracetam. J Crit Care. 2013 Oct. 28 (5):883.e9-13. [QxMD MEDLINE Link].
Zangbar B, Khalil M, Gruessner A, Joseph B, Friese R, Kulvatunyou N, et al. Levetiracetam Prophylaxis for Post-traumatic Brain Injury Seizures is Ineffective: A Propensity Score Analysis. World J Surg. 2016 Nov. 40 (11):2667-2672. [QxMD MEDLINE Link].
Temkin NR, Dikmen SS, Anderson GD, et al. Valproate therapy for prevention of posttraumatic seizures: a randomized trial. J Neurosurg. 1999 Oct. 91(4):593-600. [QxMD MEDLINE Link].
Murray GD, Teasdale GM, Schmitz H. Nimodipine in traumatic subarachnoid haemorrhage: a re-analysis of the HIT I and HIT II trials. Acta Neurochir (Wien). 1996. 138(10):1163-7. [QxMD MEDLINE Link].
Temkin NR, Anderson GD, Winn HR, Ellenbogen RG, Britz GW, Schuster J. Magnesium sulfate for neuroprotection after traumatic brain injury: a randomised controlled trial. Lancet Neurol. 2007 Jan. 6(1):29-38. [QxMD MEDLINE Link].
Wright DW, Yeatts SD, Silbergleit R, Palesch YY, Hertzberg VS, Frankel M, et al. Very Early Administration of Progesterone for Acute Traumatic Brain Injury. N Engl J Med. 2014 Dec 10. [QxMD MEDLINE Link].
Skolnick BE, Maas AI, Narayan RK, van der Hoop RG, MacAllister T, Ward JD, et al. A Clinical Trial of Progesterone for Severe Traumatic Brain Injury. N Engl J Med. 2014 Dec 10. [QxMD MEDLINE Link].
Schwamm LH. Progesterone for Traumatic Brain Injury - Resisting the Sirens' Song. N Engl J Med. 2014 Dec 10. [QxMD MEDLINE Link].
Melville, N. A. Progesterone Fails in Traumatic Brain Injury. Medscape Medical News. Available at http://www.medscape.com/viewarticle/836443. December 11, 2014; Accessed: December 11, 2014.
Empey PE, McNamara PJ, Young B, et al. Cyclosporin A disposition following acute traumatic brain injury. J Neurotrauma. 2006 Jan. 23(1):109-16. [QxMD MEDLINE Link].
Ko A, Harada MY, Barmparas G, Thomsen GM, Alban RF, Bloom MB, et al. Early propranolol after traumatic brain injury is associated with lower mortality. J Trauma Acute Care Surg. 2016 Apr. 80 (4):637-42. [QxMD MEDLINE Link].
Li ZM, Xiao YL, Zhu JX, Geng FY, Guo CJ, Chong ZL, et al. Recombinant human erythropoietin improves functional recovery in patients with severe traumatic brain injury: A randomized, double blind and controlled clinical trial. Clin Neurol Neurosurg. 2016 Sep 3. 150:80-83. [QxMD MEDLINE Link].
Maas AI, Murray G, Henney H, et al. Efficacy and safety of dexanabinol in severe traumatic brain injury: results of a phase III randomised, placebo-controlled, clinical trial. Lancet Neurol. 2006 Jan. 5(1):38-45. [QxMD MEDLINE Link].
Nguyen BM, Kim D, Bricker S, Bongard F, Neville A, Putnam B, et al. Effect of marijuana use on outcomes in traumatic brain injury. Am Surg. 2014 Oct. 80 (10):979-83. [QxMD MEDLINE Link].
Tapia-Perez JH, Sanchez-Aguilar M, Torres-Corzo JG, Gordillo-Moscoso A, Martinez-Perez P, Madeville P. Effect of rosuvastatin on amnesia and disorientation after traumatic brain injury (NCT003229758). J Neurotrauma. 2008 Aug. 25(8):1011-7. [QxMD MEDLINE Link].
Khokhar B, Simoni-Wastila L, Slejko JF, Perfetto E, Zhan M, Smith GS. Mortality and Associated Morbidities Following Traumatic Brain Injury in Older Medicare Statin Users. J Head Trauma Rehabil. 2018 Jan 30. [QxMD MEDLINE Link].
Farzanegan GR, Derakhshan N, Khalili H, Ghaffarpasand F, Paydar S. Effects of atorvastatin on brain contusion volume and functional outcome of patients with moderate and severe traumatic brain injury; a randomized double-blind placebo-controlled clinical trial. J Clin Neurosci. 2017 Oct. 44:143-147. [QxMD MEDLINE Link].
Sullivan PG, Geiger JD, Mattson MP, et al. Dietary supplement creatine protects against traumatic brain injury. Ann Neurol. 2000 Nov. 48(5):723-9. [QxMD MEDLINE Link].
Sakellaris G, Nasis G, Kotsiou M, Tamiolaki M, Charissis G, Evangeliou A. Prevention of traumatic headache, dizziness and fatigue with creatine administration. A pilot study. Acta Paediatr. 2008 Jan. 97 (1):31-4. [QxMD MEDLINE Link].
Cirak B, Rousan N, Kocak A, et al. Melatonin as a free radical scavenger in experimental head trauma. Pediatr Neurosurg. 1999 Dec. 31(6):298-301. [QxMD MEDLINE Link].
Meythaler JM, Guin-Renfroe S, Grabb P, Hadley MN. Long-term continuously infused intrathecal baclofen for spastic-dystonic hypertonia in traumatic brain injury: 1-year experience. Arch Phys Med Rehabil. 1999 Jan. 80(1):13-9. [QxMD MEDLINE Link].
Richardson D, Sheean G, Werring D, et al. Evaluating the role of botulinum toxin in the management of focal hypertonia in adults. J Neurol Neurosurg Psychiatry. 2000 Oct. 69(4):499-506. [QxMD MEDLINE Link].
Gracies JM, Brashear A, Jech R, McAllister P, Banach M, Walker H, et al. Safety and efficacy of abobotulinumtoxinA for hemiparesis in adults with upper limb spasticity after stroke or traumatic brain injury: a double-blind randomised controlled trial. Lancet Neurol. 2015 Oct. 14 (10):992-1001. [QxMD MEDLINE Link].
Plenger PM, Dixon CE, Castillo RM, et al. Subacute methylphenidate treatment for moderate to moderately severe traumatic brain injury: a preliminary double-blind placebo-controlled study. Arch Phys Med Rehabil. 1996 Jun. 77(6):536-40. [QxMD MEDLINE Link].
Kim YH, Ko MH, Na SY, et al. Effects of single-dose methylphenidate on cognitive performance in patients with traumatic brain injury: a double-blind placebo-controlled study. Clin Rehabil. 2006 Jan. 20(1):24-30. [QxMD MEDLINE Link].
Zhang L, Plotkin RC, Wang G, et al. Cholinergic augmentation with donepezil enhances recovery in short-term memory and sustained attention after traumatic brain injury. Arch Phys Med Rehabil. 2004 Jul. 85(7):1050-5. [QxMD MEDLINE Link].
Khateb A, Ammann J, Annoni JM, Diserens K. Cognition-enhancing effects of donepezil in traumatic brain injury. Eur Neurol. 2005. 54(1):39-45. [QxMD MEDLINE Link].
Bhatt M, Desai J, Mankodi A, Elias M, Wadia N. Posttraumatic akinetic-rigid syndrome resembling Parkinson's disease: a report on three patients. Mov Disord. 2000 Mar. 15(2):313-7. [QxMD MEDLINE Link].
Karli DC, Burke DT, Kim HJ, Calvanio R, Fitzpatrick M, Temple D. Effects of dopaminergic combination therapy for frontal lobe dysfunction in traumatic brain injury rehabilitation. Brain Inj. 1999 Jan. 13(1):63-8. [QxMD MEDLINE Link].
Nahas Z, Arlinghaus KA, Kotrla KJ, et al. Rapid response of emotional incontinence to selective serotonin reuptake inhibitors. J Neuropsychiatry Clin Neurosci. 1998 Fall. 10(4):453-5. [QxMD MEDLINE Link].
Garcia-Baran D, Johnson TM, Wagner J, Shen J, Geers M. Therapeutic Approach of a High Functioning Individual With Traumatic Brain Injury and Subsequent Emotional Volatility With Features of Pathological Laughter and Crying With Dextromethorphan/Quinidine. Medicine (Baltimore). 2016 Mar. 95 (12):e2886. [QxMD MEDLINE Link].
Fann JR, Uomoto JM, Katon WJ. Sertraline in the treatment of major depression following mild traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2000 Spring. 12(2):226-32. [QxMD MEDLINE Link].
Page S, Levine Peter. Forced use after TBI: promoting plasticity and function through practice. Brain Inj. 2003 Aug. 17(8):675-84. [QxMD MEDLINE Link].
Salazar AM, Warden DL, Schwab K, et al. Cognitive rehabilitation for traumatic brain injury: A randomized trial. Defense and Veterans Head Injury Program (DVHIP) Study Group. JAMA. 2000 Jun 21. 283(23):3075-81. [QxMD MEDLINE Link].
Zhao H, Bai XJ. Influence of operative timing on prognosis of patients with acute subdural hematoma. Chin J Traumatol. Oct/2009. 12:296-8.
Croce MA, Dent DL, Menke PG, et al. Acute subdural hematoma: nonsurgical management of selected patients. J Trauma. 1994 Jun. 36(6):820-6; discussion 826-7. [QxMD MEDLINE Link].
Orlando A, Levy AS, Rubin BA, Tanner A, Carrick MM, Lieser M, et al. Isolated subdural hematomas in mild traumatic brain injury. Part 1: the association between radiographic characteristics and neurosurgical intervention. J Neurosurg. 2018 Jun 15. 1-10. [QxMD MEDLINE Link].
Patel NY, Hoyt DB, Nakaji P, et al. Traumatic brain injury: patterns of failure of nonoperative management. J Trauma. Mar/2000. 48:367-74.
Nahmias J, Doben A, DeBusk G, Winston S, Alouidor R, Kaye T, et al. Mild Traumatic Brain Injuries Can Be Safely Managed without Neurosurgical Consultation: The End of a Neurosurgical "Nonsult". Am Surg. 2018 May 1. 84 (5):652-657. [QxMD MEDLINE Link].
Hutchinson PJ, Kolias AG, Timofeev IS, Corteen EA, Critchley G, Sahuquillo J, et al. Trial of Decompressive Craniectomy for Traumatic Intracranial Hypertension. N Engl J Med. 2016 Sep 7. [QxMD MEDLINE Link].
Carney N, Totten AM, O'Reilly C, et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Brain Trauma Foundation. Available at https://braintrauma.org/coma/guidelines. September 2016; Accessed: September 22, 2016.
Giza CC, Kutcher JS, Ashwal S, Barth J, Getchius TS, Gioia GA, et al. Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013 Jun 11. 80 (24):2250-7. [QxMD MEDLINE Link].
Updated Mild Traumatic Brain Injury Guideline for Adults. Centers for Disease Control and Prevention. Available at http://www.cdc.gov/traumaticbraininjury/mtbi_guideline.html. January 22, 2016; Accessed: September 24, 2016.
Holder HD, Gruenewald PJ, Ponicki WR, et al. Effect of community-based interventions on high-risk drinking and alcohol-related injuries. JAMA. 2000 Nov 8. 284(18):2341-7. [QxMD MEDLINE Link].
Gentilello LM, Rivara FP, Donovan DM, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. 1999 Oct. 230(4):473-80; discussion 480-3. [QxMD MEDLINE Link].
Thompson DC, Rivara FP, Thompson R. Helmets for preventing head and facial injuries in bicyclists. Cochrane Database Syst Rev. 2000. CD001855. [QxMD MEDLINE Link].
Heng KW, Lee AH, Zhu S, et al. Helmet use and bicycle-related trauma in patients presenting to an acute hospital in Singapore. Singapore Med J. 2006 May. 47(5):367-72. [QxMD MEDLINE Link].
Lee BH, Schofer JL, Koppelman FS. Bicycle safety helmet legislation and bicycle-related non-fatal injuries in California. Accid Anal Prev. 2005 Jan. 37(1):93-102. [QxMD MEDLINE Link].
Siegrist M, Freiberger E, Geilhof B, Salb J, Hentschke C, Landendoerfer P, et al. Fall Prevention in a Primary Care Setting. Dtsch Arztebl Int. 2016 May 27. 113 (21):365-72. [QxMD MEDLINE Link].
Donders J, Boonstra T. Correlates of invalid neuropsychological test performance after traumatic brain injury. Brain Inj. 2007 Mar. 21(3):319-26. [QxMD MEDLINE Link].
Hutchison M, Comper P, Mainwaring L, Richards D. The influence of musculoskeletal injury on cognition: implications for concussion research. Am J Sports Med. 2011 Nov. 39(11):2331-7. [QxMD MEDLINE Link].
Dacey RG Jr, Alves WM, Rimel RW, et al. Neurosurgical complications after apparently minor head injury. Assessment of risk in a series of 610 patients. J Neurosurg. 1986 Aug. 65(2):203-10. [QxMD MEDLINE Link].
Deb S, Lyons I, Koutzoukis C. Neuropsychiatric sequelae one year after a minor head injury. J Neurol Neurosurg Psychiatry. 1998 Dec. 65(6):899-902. [QxMD MEDLINE Link].
Dikmen SS, Corrigan JD, Levin HS, et al. Cognitive Outcome Following Traumatic Brain Injury. J Head Trauma Rehabil. 2009. 24:430-438.
Cantu RC. Second-impact syndrome. Clin Sports Med. 1998 Jan. 17(1):37-44. [QxMD MEDLINE Link].
McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on Concussion in Sport 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Clin J Sport Med. May/2009. 19:185-200.
McCrory PR, Berkovic SF. Second impact syndrome. Neurology. 1998 Mar. 50(3):677-83. [QxMD MEDLINE Link].
Mayers L. Return-to-Play Criteria After Athletic Concussion. Arch Neurol. Sept/2008. 65:1158-1161.
McLendon LA, Kralik SF, Grayson PA, Golomb MR. The Controversial Second Impact Syndrome: A Review of the Literature. Pediatr Neurol. 2016 Sep. 62:9-17. [QxMD MEDLINE Link].
Asikainen I, Kaste M, Sarna S. Early and late posttraumatic seizures in traumatic brain injury rehabilitation patients: brain injury factors causing late seizures and influence of seizures on long-term outcome. Epilepsia. 1999 May. 40(5):584-9. [QxMD MEDLINE Link].
Angeleri F, Majkowski J, Cacchio G, et al. Posttraumatic epilepsy risk factors: one-year prospective study after head injury. Epilepsia. 1999 Sep. 40(9):1222-30. [QxMD MEDLINE Link].
Diaz-Arrastia R, Agostini MA, Frol AB, et al. Neurophysiologic and neuroradiologic features of intractable epilepsy after traumatic brain injury in adults. Arch Neurol. 2000 Nov. 57(11):1611-6. [QxMD MEDLINE Link].
Obermann M, Holbe D, Katsarava Z. Post-traumatic headache. Expert Rev Neurother. Sep/2009. 9:1361-1370.
Packard RC, Ham LP. Pathogenesis of posttraumatic headache and migraine: a common headache pathway?. Headache. 1997 Mar. 37(3):142-52. [QxMD MEDLINE Link].
Warner JS. Posttraumatic headache--a myth?. Arch Neurol. 2000 Dec. 57(12):1778-80; discussion 1780-1. [QxMD MEDLINE Link].
Jorge RE, Robinson RG, Moser D, Tateno A, Crespo-Facorro B, Arndt S. Major depression following traumatic brain injury. Arch Gen Psychiatry. 2004 Jan. 61(1):42-50. [QxMD MEDLINE Link].
Singh R, Mason S, Lecky F, Dawson J. Prevalence of depression after TBI in a prospective cohort: The SHEFBIT study. Brain Inj. 2018. 32 (1):84-90. [QxMD MEDLINE Link].
Bilgic B, Baral-Kulaksizoglu I, Hanagasi H, et al. Obsessive-compulsive disorder secondary to bilateral frontal damage due to a closed head injury. Cogn Behav Neurol. 2004 Jun. 17(2):118-20. [QxMD MEDLINE Link].
Sachdev P, Smith JS, Cathcart S. Schizophrenia-like psychosis following traumatic brain injury: a chart- based descriptive and case-control study. Psychol Med. 2001 Feb. 31(2):231-9. [QxMD MEDLINE Link].
McCartan DP, Fleming FJ, Motherway C, Grace PA. Management and outcome in patients following head injury admitted to an Irish Regional Hospital. Brain Inj. 2008 Apr. 22(4):305-12. [QxMD MEDLINE Link].
van der Naalt J, van Zomeren AH, Sluiter WJ, et al. One year outcome in mild to moderate head injury: the predictive value of acute injury characteristics related to complaints and return to work. J Neurol Neurosurg Psychiatry. 1999 Feb. 66(2):207-13. [QxMD MEDLINE Link].
Chamelian L, Feinstein A. Outcome after mild to moderate traumatic brain injury: the role of dizziness. Arch Phys Med Rehabil. 2004 Oct. 85(10):1662-6. [QxMD MEDLINE Link].
DiSanto D, Kumar RG, Juengst SB, Hart T, O'Neil-Pirozzi TM, Zasler ND, et al. Employment Stability in the First 5 Years After Moderate-to-Severe Traumatic Brain Injury. Arch Phys Med Rehabil. 2018 Jul 26. [QxMD MEDLINE Link].
Stromberg KA, Agyemang AA, Graham KM, Walker WC, Sima AP, Marwitz JH, et al. Using Decision Tree Methodology to Predict Employment After Moderate to Severe Traumatic Brain Injury. J Head Trauma Rehabil. 2018 Sep 18. [QxMD MEDLINE Link].
Harrison-Felix C, Pretz C, Hammond FM, Cuthbert JP, Bell J, Corrigan J, et al. Life Expectancy after Inpatient Rehabilitation for Traumatic Brain Injury in the United States. J Neurotrauma. 2015 Dec 1. 32 (23):1893-901. [QxMD MEDLINE Link].
Richmond R, Aldaghlas TA, Burke C, Rizzo AG, Griffen M, Pullarkat R. Age: Is It All in the Head? Factors Influencing Mortality in Elderly Patients With Head Injuries. J Trauma. 2011 Feb 17. [QxMD MEDLINE Link].
Ritchie PD, Cameron PA, Ugoni AM, et al. A study of the functional outcome and mortality in elderly patients with head injuries. J Clin Neurosci. 2000 Jul. 7(4):301-4. [QxMD MEDLINE Link].
Røe C, Skandsen T, Manskow U, Ader T, Anke A. Mortality and One-Year Functional Outcome in Elderly and Very Old Patients with Severe Traumatic Brain Injuries: Observed and Predicted. Behav Neurol. 2015. 2015:845491. [QxMD MEDLINE Link].
Wade DT, King NS, Wenden FJ, et al. Routine follow up after head injury: a second randomised controlled trial. J Neurol Neurosurg Psychiatry. 1998 Aug. 65(2):177-83. [QxMD MEDLINE Link].
Cox AL, Coles AJ, Nortje J, et al. An investigation of auto-reactivity after head injury. J Neuroimmunol. 2006 May. 174(1-2):180-6. [QxMD MEDLINE Link].
Thomas KE, Stevens JA, Sarmiento K, Wald MM. Fall-related traumatic brain injury deaths and hospitalizations among older adults--United States, 2005. J Safety Res. 2008. 39(3):269-72. [QxMD MEDLINE Link].
Jennett B. Epidemiology of head injury. J Neurol Neurosurg Psychiatry. 1996 Apr. 60(4):362-9. [QxMD MEDLINE Link].
Wrightson P, Gronwall D. Mild head injury in New Zealand: incidence of injury and persisting symptoms. N Z Med J. 1998 Mar 27. 111(1062):99-101. [QxMD MEDLINE Link].
Schanke AK, Sundet K. Comprehensive driving assessment: neuropsychological testing and on- road evaluation of brain injured patients. Scand J Psychol. 2000 Jun. 41(2):113-21. [QxMD MEDLINE Link].
Anderson P. Hemodynamic Complications Common in Traumatic Brain Injury. Available at http://www.medscape.com/viewarticle/778999. Accessed: March 25, 2013.
Bazarian JJ, McClung J, Shah MN, et al. Mild traumatic brain injury in the United States, 1998--2000. Brain Inj. 2005 Feb. 19(2):85-91. [QxMD MEDLINE Link].
Black K, Zafonte R, Millis S, et al. Sitting balance following brain injury: does it predict outcome?. Brain Inj. 2000 Feb. 14(2):141-52. [QxMD MEDLINE Link].
Blumbergs PC, Scott G, Manavis J, et al. Staining of amyloid precursor protein to study axonal damage in mild head injury. Lancet. 1994 Oct 15. 344(8929):1055-6. [QxMD MEDLINE Link].
Bruce DA, Alavi A, Bilaniuk L, et al. Diffuse cerebral swelling following head injuries in children: the syndrome of "malignant brain edema". J Neurosurg. 1981 Feb. 54(2):170-8. [QxMD MEDLINE Link].
Cassidy JD, Carroll LJ, Cote P, et al. Effect of eliminating compensation for pain and suffering on the outcome of insurance claims for whiplash injury. N Engl J Med. 2000 Apr 20. 342(16):1179-86. [QxMD MEDLINE Link].
Centers for Disease Control and Prevention. Sports-related recurrent brain injuries--United States. MMWR Morb Mortal Wkly Rep. 1997 Mar 14. 46(10):224-7. [QxMD MEDLINE Link].
Cernak I, Savic VJ, Kotur J, et al. Characterization of plasma magnesium concentration and oxidative stress following graded traumatic brain injury in humans. J Neurotrauma. 2000 Jan. 17(1):53-68. [QxMD MEDLINE Link].
Chesnut RM. Intracranial pressure monitoring in brain-injured patients is associated with worsening of survival. J Trauma. Aug/2008. 65:500-1.
Chesnut RM, Marshall LF, Klauber MR, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993 Feb. 34(2):216-22. [QxMD MEDLINE Link].
Chiu WT, Kuo CY, Hung CC, et al. The effect of the Taiwan motorcycle helmet use law on head injuries. Am J Public Health. 2000 May. 90(5):793-6. [QxMD MEDLINE Link].
Cho YW, Jang SH, Lee ZI, et al. Effect and appropriate restriction period of constraint-induced movement therapy in hemiparetic patients with brain injury: a brief report. NeuroRehabilitation. 2005. 20(2):71-4. [QxMD MEDLINE Link].
Collins MW, Grindel SH, Lovell MR, et al. Relationship between concussion and neuropsychological performance in college football players. JAMA. 1999 Sep 8. 282(10):964-70. [QxMD MEDLINE Link].
Dharap SB, Khandkar AA, Pandey A, Sharma AK. Repeat CT scan in closed head injury. Injury. 2005 Mar. 36(3):412-6. [QxMD MEDLINE Link].
Drake AI, Gray N, Yoder S, et al. Factors predicting return to work following mild traumatic brain injury: a discriminant analysis. J Head Trauma Rehabil. 2000 Oct. 15(5):1103-12. [QxMD MEDLINE Link].
Eisenberg HM, Frankowski RF, Contant CF, et al. High-dose barbiturate control of elevated intracranial pressure in patients with severe head injury. J Neurosurg. 1988 Jul. 69(1):15-23. [QxMD MEDLINE Link].
Fabbri A, Servadei F, Marchesini G, et al. Early predictors of unfavorable outcome in subjects with moderate head injury in the emergency department. J Neurol Neurosurg Psychiatry. May/2008. 79:567-73.
Feldman Z, Gurevitch B, Artru AA, et al. Effect of magnesium given 1 hour after head trauma on brain edema and neurological outcome. J Neurosurg. 1996 Jul. 85(1):131-7. [QxMD MEDLINE Link].
Gordon WA, Brown M, Sliwinski M, et al. The enigma of "hidden" traumatic brain injury. J Head Trauma Rehabil. 1998 Dec. 13(6):39-56. [QxMD MEDLINE Link].
Guerra WK, Gaab MR, Dietz H, et al. Surgical decompression for traumatic brain swelling: indications and results. J Neurosurg. 1999 Feb. 90(2):187-96. [QxMD MEDLINE Link].
Gusmao SN, Pittella JE. Extradural haematoma and diffuse axonal injury in victims of fatal road traffic accidents. Br J Neurosurg. 1998 Apr. 12(2):123-6. [QxMD MEDLINE Link].
Haig AJ, Ruess JM. Recovery from vegetative state of six months'' duration associated with Sinemet (levodopa/carbidopa). Arch Phys Med Rehabil. 1990 Dec. 71(13):1081-3. [QxMD MEDLINE Link].
Hall JR, Reyes HM, Horvat M, et al. The mortality of childhood falls. J Trauma. 1989 Sep. 29(9):1273-5. [QxMD MEDLINE Link].
Haltiner AM, Newell DW, Temkin NR, et al. Side effects and mortality associated with use of phenytoin for early posttraumatic seizure prophylaxis. J Neurosurg. 1999 Oct. 91(4):588-92. [QxMD MEDLINE Link].
Hamill RW, Woolf PD, McDonald JV, et al. Catecholamines predict outcome in traumatic brain injury. Ann Neurol. 1987 May. 21(5):438-43. [QxMD MEDLINE Link].
Hanlon RE, Demery JA, Martinovich Z, et al. Effects of acute injury characteristics on neurophysical status and vocational outcome following mild traumatic brain injury. Brain Inj. 1999 Nov. 13(11):873-87. [QxMD MEDLINE Link].
Harders A, Kakarieka A, Braakman R. Traumatic subarachnoid hemorrhage and its treatment with nimodipine. German tSAH Study Group. J Neurosurg. 1996 Jul. 85(1):82-9. [QxMD MEDLINE Link].
Homayoun P, Parkins NE, Soblosky J, et al. Cortical impact injury in rats promotes a rapid and sustained increase in polyunsaturated free fatty acids and diacylglycerols. Neurochem Res. 2000 Feb. 25(2):269-76. [QxMD MEDLINE Link].
Ikonomidou C, Stefovska V, Turski L. Neuronal death enhanced by N-methyl-D-aspartate antagonists. Proc Natl Acad Sci U S A. 2000 Nov 7. 97(23):12885-90. [QxMD MEDLINE Link].
Inamasu J, Hori S, Aoki K, et al. CT scans essential after posttraumatic loss of consciousness. Am J Emerg Med. 2000 Nov. 18(7):810-1. [QxMD MEDLINE Link].
Jordan BD, Relkin NR, Ravdin LD, et al. Apolipoprotein E epsilon4 associated with chronic traumatic brain injury in boxing. JAMA. 1997 Jul 9. 278(2):136-40. [QxMD MEDLINE Link].
Keenan HT, Brundage SI, Thompson DC, et al. Does the face protect the brain? A case-control study of traumatic brain injury and facial fractures. Arch Surg. 1999 Jan. 134(1):14-7. [QxMD MEDLINE Link].
Knoller N, Levi L, Shoshan I, et al. Dexanabinol (HU-211) in the treatment of severe closed head injury: a randomized, placebo-controlled, phase II clinical trial. Crit Care Med. 2002 Mar. 30(3):548-54. [QxMD MEDLINE Link].
Kobori N, Clifton GL, Dash P, et al. Altered expression of novel genes in the cerebral cortex following experimental brain injury. Brain Res Mol Brain Res. 2002 Aug 15. 104(2):148-58. [QxMD MEDLINE Link].
Kobrine AI, Timmins E, Rajjoub RK, et al. Demonstration of massive traumatic brain swelling within 20 minutes after injury. Case report. J Neurosurg. 1977 Feb. 46(2):256-8. [QxMD MEDLINE Link].
Lal S, Merbtiz CP, Grip JC. Modification of function in head-injured patients with Sinemet. Brain Inj. 1988 Jul-Sep. 2(3):225-33. [QxMD MEDLINE Link].
Landau WM. Tizanidine and spasticity. Neurology. 1995 Dec. 45(12):2295-6. [QxMD MEDLINE Link].
Landy PJ. Neurological sequelae of minor head and neck injuries. Injury. 1998 Apr. 29(3):199-206. [QxMD MEDLINE Link].
Lane PL, Skoretz TG, Doig G, et al. Intracranial pressure monitoring and outcomes after traumatic brain injury. Can J Surg. 2000 Dec. 43(6):442-8. [QxMD MEDLINE Link].
Lang DA, Teasdale GM, Macpherson P, et al. Diffuse brain swelling after head injury: more often malignant in adults than children?. J Neurosurg. 1994 Apr. 80(4):675-80. [QxMD MEDLINE Link].
Levin HS, Gary HE Jr, Eisenberg HM, et al. Neurobehavioral outcome 1 year after severe head injury. Experience of the Traumatic Coma Data Bank. J Neurosurg. 1990 Nov. 73(5):699-709. [QxMD MEDLINE Link].
Levin HS, Mattis S, Ruff RM, et al. Neurobehavioral outcome following minor head injury: a three-center study. J Neurosurg. 1987 Feb. 66(2):234-43. [QxMD MEDLINE Link].
Levin HS, Williams DH, Eisenberg HM, et al. Serial MRI and neurobehavioural findings after mild to moderate closed head injury. J Neurol Neurosurg Psychiatry. 1992 Apr. 55(4):255-62. [QxMD MEDLINE Link].
Li J, Brown J, Levine M. Mild head injury, anticoagulants, and risk of intracranial injury. Lancet. 2001 Mar 10. 357(9258):771-2. [QxMD MEDLINE Link].
Macfarlane DP, Nicoll JA, Smith C, et al. APOE epsilon4 allele and amyloid beta-protein deposition in long term survivors of head injury. Neuroreport. 1999 Dec 16. 10(18):3945-8. [QxMD MEDLINE Link].
Marion DW, Penrod LE, Kelsey SF, et al. Treatment of traumatic brain injury with moderate hypothermia. N Engl J Med. 1997 Feb 20. 336(8):540-6. [QxMD MEDLINE Link].
Marmarou A, Anderson RL, Ward JD, et al. Impact of ICP instability and hypotension on outcome in patients with severe head trauma. J Neurosurg. 1991. 75:S59-66.
Marshall LF, Gautille T, Klauber MR, et al. The outcome of severe head injury. J Neurosurg. 1991. 75:S28-36.
Mayers l. Return-to-Play Criteria after Athletic Concussion. Archives of Neurology. Sep/2008. 65:1158-1161.
Miller EC, Derlet RW, Kinser D. Minor head trauma: Is computed tomography always necessary?. Ann Emerg Med. 1996 Mar. 27(3):290-4. [QxMD MEDLINE Link].
Mittenberg W, Strauman S. Diagnosis of mild head injury and the postconcussion syndrome. J Head Trauma Rehabil. 2000 Apr. 15(2):783-91. [QxMD MEDLINE Link].
Mosimann UP, Muri RM, Felblinger J, et al. Saccadic eye movement disturbances in whiplash patients with persistent complaints. Brain. 2000 Apr. 123 ( Pt 4):828-35. [QxMD MEDLINE Link].
Murray JA, Demetriades D, Berne TV, et al. Prehospital intubation in patients with severe head injury. J Trauma. 2000 Dec. 49(6):1065-70. [QxMD MEDLINE Link].
Nagy KK, Joseph KT, Krosner SM, et al. The utility of head computed tomography after minimal head injury. J Trauma. 1999 Feb. 46(2):268-70. [QxMD MEDLINE Link].
Owings JT, Wisner DH, Battistella FD, et al. Isolated transient loss of consciousness is an indicator of significant injury. Arch Surg. 1998 Sep. 133(9):941-6. [QxMD MEDLINE Link].
Packard RC, Ham LP. Posttraumatic headache. J Neuropsychiatry Clin Neurosci. 1994 Summer. 6(3):229-36. [QxMD MEDLINE Link].
Palmer AM, Marion DW, Botscheller ML, et al. Traumatic brain injury-induced excitotoxicity assessed in a controlled cortical impact model. J Neurochem. 1993 Dec. 61(6):2015-24. [QxMD MEDLINE Link].
Patel NY, Hoyt DB, Nakaji P, et al. Traumatic brain injury: patterns of failure of nonoperative management. J Trauma. 2000 Mar. 48(3):367-74; discussion 374-5. [QxMD MEDLINE Link].
Paterakis K, Karantanas AH, Komnos A, et al. Outcome of patients with diffuse axonal injury: the significance and prognostic value of MRI in the acute phase. J Trauma. 2000 Dec. 49(6):1071-5. [QxMD MEDLINE Link].
Pop E. Dexanabinol Pharmos. Curr Opin Investig Drugs. 2000 Dec. 1(4):494-503. [QxMD MEDLINE Link].
Procaccio F, Stocchetti N, Citerio G, et al. Guidelines for the treatment of adults with severe head trauma (part II). Criteria for medical treatment. J Neurosurg Sci. 2000 Mar. 44(1):11-8. [QxMD MEDLINE Link].
Report of the Quality Standards Subcommittee, American Academy of Neurology. Practice parameter: the management of concussion in sports (summary statement). Report of the Quality Standards Subcommittee. Neurology. 1997 Mar. 48(3):581-5. [QxMD MEDLINE Link].
Rugg-Gunn FJ, Symms MR, Barker GJ, et al. Diffusion imaging shows abnormalities after blunt head trauma when conventional magnetic resonance imaging is normal. J Neurol Neurosurg Psychiatry. 2001 Apr. 70(4):530-3. [QxMD MEDLINE Link].
Salmond CH, Menon DK, Chatfield DA, et al. Diffusion tensor imaging in chronic head injury survivors: correlations with learning and memory indices. Neuroimage. 2006 Jan 1. 29(1):117-24. [QxMD MEDLINE Link].
Signoretti S, Marmarou A, Tavazzi B, et al. The protective effect of cyclosporin A upon N-acetylaspartate and mitochondrial dysfunction following experimental diffuse traumatic brain injury. J Neurotrauma. 2004 Sep. 21(9):1154-67. [QxMD MEDLINE Link].
Sloan RL, Brown KW, Pentland B. Fluoxetine as a treatment for emotional lability after brain injury. Brain Inj. 1992 Jul-Aug. 6(4):315-9. [QxMD MEDLINE Link].
Snoek JW, Minderhoud JM, Wilmink JT. Delayed deterioration following mild head injury in children. Brain. 1984 Mar. 107 ( Pt 1):15-36. [QxMD MEDLINE Link].
Speech TJ, Rao SM, Osmon DC, et al. A double-blind controlled study of methylphenidate treatment in closed head injury. Brain Inj. 1993 Jul-Aug. 7(4):333-8. [QxMD MEDLINE Link].
Struchen MA, Hannay HJ, Contant CF, et al. The relation between acute physiological variables and outcome on the Glasgow Outcome Scale and Disability Rating Scale following severe traumatic brain injury. J Neurotrauma. 2001 Feb. 18(2):115-25. [QxMD MEDLINE Link].
Sturmi JE, Smith C, Lombardo JA. Mild brain trauma in sports. Diagnosis and treatment guidelines. Sports Med. 1998 Jun. 25(6):351-8. [QxMD MEDLINE Link].
Sullivan PG, Rabchevsky AG, Waldmeier PC, Springer JE. Mitochondrial permeability transition in CNS trauma: cause or effect of neuronal cell death?. J Neurosci Res. 2005 Jan 1-15. 79(1-2):231-9. [QxMD MEDLINE Link].
Teasdale GM. Head injury. J Neurol Neurosurg Psychiatry. 1995 May. 58(5):526-39. [QxMD MEDLINE Link].
The Brain Trauma Foundation, The American Association of Neurological Surgeons, The Joint Section on Neurotrauma and Critical Care. Role of steroids. J Neurotrauma. 2000 Jun-Jul. 17(6-7):531-5. [QxMD MEDLINE Link].
The Brain Trauma Foundation, The American Association of Neurological Surgeons, The Joint Section on Neurotrauma and Critical Care. Use of barbiturates in the control of intracranial hypertension. J Neurotrauma. 2000 Jun-Jul. 17(6-7):527-30. [QxMD MEDLINE Link].
Thurman DJ, Alverson C, Dunn KA, et al. Traumatic brain injury in the United States: A public health perspective. J Head Trauma Rehabil. 1999 Dec. 14(6):602-15. [QxMD MEDLINE Link].
Towne AR, Waterhouse EJ, Boggs JG, et al. Prevalence of nonconvulsive status epilepticus in comatose patients. Neurology. 2000 Jan 25. 54(2):340-5. [QxMD MEDLINE Link].
van Reekum R, Cohen T, Wong J. Can traumatic brain injury cause psychiatric disorders?. J Neuropsychiatry Clin Neurosci. 2000 Summer. 12(3):316-27. [QxMD MEDLINE Link].
Velmahos GC, Jindal A, Chan LS, et al. "Insignificant" mechanism of injury: not to be taken lightly. J Am Coll Surg. 2001 Feb. 192(2):147-52. [QxMD MEDLINE Link].
Wesson D, Spence L, Hu X, et al. Trends in bicycling-related head injuries in children after implementation of a community-based bike helmet campaign. J Pediatr Surg. 2000 May. 35(5):688-9. [QxMD MEDLINE Link].
Whelan FJ, Walker MS, Schultz SK. Donepezil in the treatment of cognitive dysfunction associated with traumatic brain injury. Ann Clin Psychiatry. 2000 Sep. 12(3):131-5. [QxMD MEDLINE Link].
Whyte J, Hart T, Schuster K, et al. Effects of methylphenidate on attentional function after traumatic brain injury. A randomized, placebo-controlled trial. Am J Phys Med Rehabil. 1997 Nov-Dec. 76(6):440-50. [QxMD MEDLINE Link].
Wilberger JE Jr, Harris M, Diamond DL. Acute subdural hematoma: morbidity, mortality, and operative timing. J Neurosurg. 1991 Feb. 74(2):212-8. [QxMD MEDLINE Link].
Withaar FK, Brouwer WH, van Zomeren AH. Fitness to drive in older drivers with cognitive impairment. J Int Neuropsychol Soc. 2000 May. 6(4):480-90. [QxMD MEDLINE Link].
Young B, Runge JW, Waxman KS, et al. Effects of pegorgotein on neurologic outcome of patients with severe head injury. A multicenter, randomized controlled trial. JAMA. 1996 Aug 21. 276(7):538-43. [QxMD MEDLINE Link].
Zafonte RD, Mann NR. Cerebral salt wasting syndrome in brain injury patients: a potential cause of hyponatremia. Arch Phys Med Rehabil. 1997 May. 78(5):540-2. [QxMD MEDLINE Link].
Orlando A, Levy AS, Rubin BA, Tanner A, Carrick MM, Lieser M, et al. Isolated subdural hematomas in mild traumatic brain injury. Part 1: the association between radiographic characteristics and neurosurgical intervention. J Neurosurg. 2018 Jun 15. 1-10. [QxMD MEDLINE Link].
Leland A, Tavakol K, Scholten J, Libin AV, Mathis D, Maron D, et al. Affective and Cognitive Conditions are Stronger Predictors of Success with Community Reintegration than Gait and Balance Performance in Veterans with Mild Traumatic Brain Injury. Med Arch. 2017 Dec. 71 (6):417-423. [QxMD MEDLINE Link].
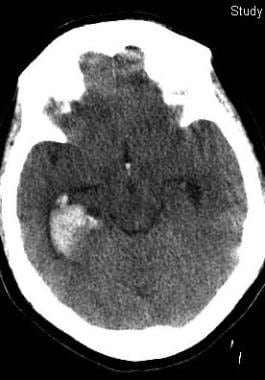 This 50-year-old woman with epilepsy seized and struck her head. Her initial Glasgow Coma Scale score was 12. Her scan shows prominent right temporal bleeding. She recovered to baseline without surgery.
This 50-year-old woman with epilepsy seized and struck her head. Her initial Glasgow Coma Scale score was 12. Her scan shows prominent right temporal bleeding. She recovered to baseline without surgery.







