Background
A Meckel diverticulum is a vestigial remnant of the omphalomesenteric (vitellointestinal) duct. [1] As a congenital anomaly, it is a true diverticulum that includes all three coats of the small intestine. Generally, a Meckel diverticulum ranges from 1 to 12 cm in length and is found 45-90 cm proximal to the ileocecal valve. It frequently contains heterotopic tissue [2] ; when it does, gastric mucosa accounts for 50%. (See the image below.)
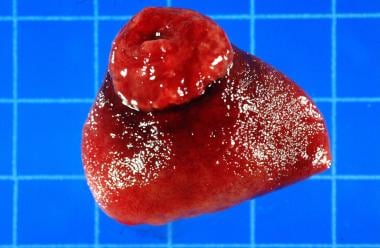
 Ileal (Meckel) diverticula and other remnants of yolk stalk. Section of ileum and diverticulum with ulcer.
Ileal (Meckel) diverticula and other remnants of yolk stalk. Section of ileum and diverticulum with ulcer.
Pluripotential cells line the omphalomesenteric duct; thus, gastric, colonic, duodenal, and pancreatic mucosa may be present. The diverticulum may or may not be attached to the umbilicus with a fibrous cord.
Autopsy records show that Meckel diverticulum occurs in about 2% of the general population. The male-to-female ratio is 3:1 for patients with symptomatic diverticula, but it is 1:1 for patients with asymptomatic diverticula.
Anomalies of Omphalomesenteric Duct
Human embryos initially have convex umbilical loops of primitive gut that communicate freely with the yolk sac through the omphalomesenteric duct. As development proceeds, the duct normally becomes occluded and disappears entirely by weeks 8-10 of gestation. The following anomalies are caused by the persistence of the omphalomesenteric duct:
-
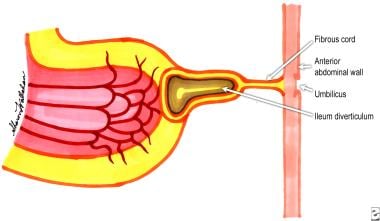
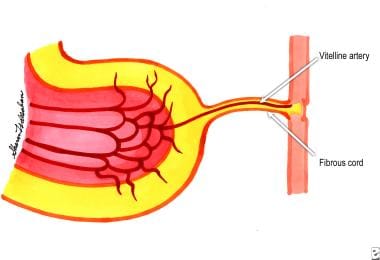
An outpouching diverticulum secondary to persistence of the proximal part of the vitelline duct (Meckel diverticulum), with or without a fibrous cord; Meckel diverticulum is the most common anomaly (see the first image below)
-
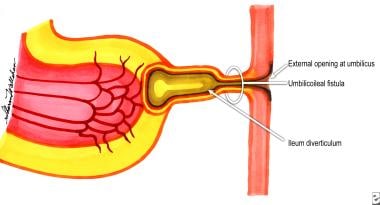
Persistence and patency of the entire tract, leading to a congenital umbilicoileal fistula (see the second image below)
-
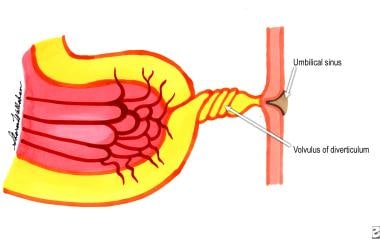
Persistence of the duct near the umbilicus, forming an umbilical sinus (see the third image below)
-
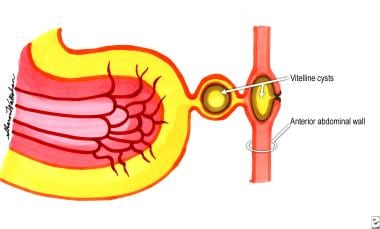
Fluid-filled cysts (enterocystomas) located either intra-abdominally or just below the umbilical skin because of persistence of the middle portion of the duct (see the fourth image below)
-
Obliteration of the lumen of the duct but persistence of the duct, forming a fibrous cord (see the fifth image below)
Complications of Meckel Diverticulum
Although most commonly discovered as an incidental finding on laparotomy or laparoscopy, Meckel diverticulum can be associated with life-threatening disease states. [3] Retrospective studies suggest that the onset and frequency of complications decrease during life. The risk of complications ranges from 4% to 25% in various studies. Complications manifest as the following:
-
Ulceration
-
Hemorrhage
In an excellent population-based study by Cullen et al that covered patient data over a period of 42 years, the lifetime risk of developing a complication that required surgery was estimated to be 6.4%. [4]
Hemorrhage
Hemorrhage is the most common complication of Meckel diverticulum, accounting for about 20-30% of all complications. It is more common in children younger than 2 years and in males. The patient complains of passing bright red blood in the stools. Bleeding may range from minimal recurrent episodes of hematochezia to massive shock-producing hemorrhage.
The rate of bleeding can be assessed on the basis of the following:
-
Quantity of blood lost in the stools
-
Appearance of the material passed through the rectum
-
Hemodynamic state
Hemorrhage from a Meckel diverticulum may or may not be associated with abdominal pain or tenderness. Patients may also present with weakness and anemia and may have a history of self-limiting episodes of intestinal bleeding.
Characteristics of hemorrhage based on the appearance of stools include the following:
-
Bright red blood in the stools - Brisk hemorrhage
-
Tarry stools - The bleeding is probably minor and associated with slow intestinal transit; tarry stools are commonly observed in patients with upper gastrointestinal (GI) bleeding, because transit through the bowel produces alteration of blood
-
Currant jelly stools - Associated with copious mucus owing to ischemia of the bowel; commonly observed in intussusception
-
Blood-streaked stools - A sign of fissure-in-ano
The gastric mucosa found in the diverticulum (see the image below) may form a chronic ulcer and may also damage the adjacent ileal mucosa through acid production. Ectopic gastric mucosa is found in about 50% of all Meckel diverticula; in bleeding Meckel diverticula, the incidence increases to 75%. Perforation may occur, and the patient then presents with an acute abdomen, often associated with air under the diaphragm, best visualized on an erect chest radiograph.
When a patient presents with painless lower GI bleeding, Meckel diverticulum should always be suspected. Panendoscopy helps exclude disease in the upper GI and colorectal regions, the two most common sites of GI bleeding.
Intestinal obstruction
This is another frequent complication; it is observed in 20-25% of patients with symptomatic Meckel diverticulum. The diagnosis of bowel obstruction due to Meckel diverticulum may not be established preoperatively. At exploration, Meckel diverticulum may be identified as the cause of obstruction. (See the image below.)
 Preoperative CT scan of abdomen in 14-year-old child, showing intestinal obstruction due to Meckel diverticulum.
Preoperative CT scan of abdomen in 14-year-old child, showing intestinal obstruction due to Meckel diverticulum.
Various mechanisms of intestinal obstruction occur with Meckel diverticulum as a causative factor. Because the omphalomesenteric duct may be attached to the abdominal wall by a fibrotic band, a volvulus of the small bowel around the band may occur. The diverticulum may also form the lead point of an intussusception and cause obstruction. Infrequently, a tumor arising in the wall of the diverticulum may form the lead point for intussusception. When incarcerated in an inguinal hernia, a Meckel diverticulum is called a Littré hernia. [5]
Patients with intestinal obstruction due to Meckel diverticulum present with abdominal pain, vomiting, and obstipation. Radiography of the abdomen may indicate an ileus or frank stepladder air-fluid levels, as observed in dynamic intestinal obstruction.
In cases of intussusception, patients may also present with a palpable lump in the lower abdomen and currant jelly stools.
Diverticulitis
This condition develops in approximately 10-20% of patients with symptomatic Meckel diverticulum, occurring more often in the elderly population. Patients may present with symptoms of intermittent, crampy abdominal pain and tenderness in the periumbilical area. Perforation of the inflamed diverticulum leads to peritonitis.
Stasis in the diverticulum, especially in one with a narrow neck, causes inflammation and secondary infection leading to diverticulitis. Diverticular inflammation can lead to adhesions, which cause intestinal obstruction.
Umbilical anomalies
These occur in up to 10% of patients and consist of fistulas, sinuses, cysts, and fibrous bands between the diverticulum and the umbilicus. A patient may present with a chronic discharging umbilical sinus accompanied by infection or excoriation of periumbilical skin. There may be a history of recurrent infection, sinus healing, or abdominal-wall abscess formation. When a fistula is present, intestinal mucosa may be identified on the skin.
Cannulation and injection with radiographic contrast help to delineate the entire tract and aid in planning a surgical approach for cure. A discharging sinus should be approached surgically with a view toward correction. Exploratory laparotomy may be required.
When found at laparotomy, a fibrous band should be excised because of the risk of internal herniation and volvulus.
Neoplasm
This is the pathology least commonly associated with Meckel diverticulum and is reported in approximately 4-5% of complicated Meckel diverticulum cases. Of the various types of tumors reported, leiomyoma is the one that is most frequently found, followed by leiomyosarcoma, carcinoid tumor, and fibroma. A case of ectopic gastric adenocarcinoma has been reported. Lipoma and angioma have also been found. [6, 7]
Other complications
Other reported complications in Meckel diverticulum include the following:
-
Vesicodiverticular fistula
-
"Daughter" diverticulum (a diverticulum formed within a Meckel diverticulum)
-
Stones and phytobezoar formed in the Meckel diverticulum
Differential Diagnosis
A diagnosis of symptomatic or complicated Meckel diverticulum is difficult to confirm on the basis of traditional history, physical examination, and laboratory testing. [8] It is always considered as a differential diagnosis in cases of intestinal obstruction and intestinal hemorrhage. Painless, profuse hematochezia, especially in a child, should alert a clinician to the possibility of such a diagnosis and should prompt further investigation.
Thus, in a child, the differential diagnosis for right-lower-quadrant pain includes appendicitis, acute mesenteric lymphadenitis, intussusception, or Meckel diverticulitis. In an adult, Meckel diverticulum should be entertained in the diagnosis for lower GI bleeding, which would also include angiodysplasias, malignancy, arteriovenous malformations, and other causes.
Diagnostic Studies
Asymptomatic Meckel diverticulum
Laparoscopy and laparotomy are the most frequent means by which an incidental diverticulum is found. An upper GI series with small-bowel follow-through also detects a diverticulum. The diverticulum appears as a smooth, white, globular shadow on the antimesenteric border of the ileum, approximately 50 cm proximal to the ileocecal valve.
Symptomatic Meckel diverticulum
Technetium-99m pertechnate radioisotope scanning
Diagnosis of a bleeding Meckel diverticulum is established by means of technetium-99m (99mTc) pertechnetate radioisotope scanning. [9] This isotope, administered intravenously, is readily taken up by the gastric mucosa. Reportedly, 1.8 cm2 of ectopic gastric mucosa in Meckel diverticulum is required for a positive result.
Pentagastrin, which is known to increase the acid production of ectopic gastric mucosa, enhances radioisotope uptake by the cells. Using a histamine-2 (H2) receptor blocker with pentagastrin provides a synergistic effect, in that it blocks intraluminal release and promotes retention of the isotope. The value of 99mTc pertechnate scanning is more specific in children. [9]
The incidence of false-negative results is high, especially in adults; therefore, a negative scan finding does not exclude a Meckel diverticulum. False-positive results are observed in patients with intussusception, volvulus, obstruction of the small intestine, acute appendicitis, carcinoid of the appendix, or carcinoma of the cecum. The use of pentagastrin and an H2 receptor blocker helps minimize the number of false-negative results.
Approximately 30 images may be required (at 1-minute intervals) to demonstrate activity in the terminal ileum.
In September 2014, the Society of Nuclear Medicine and Molecular Imaging (SNMMI) and the European Association for Nuclear Medicine (EANM) issued a practice guideline for the use of scintigraphy for Meckel diverticulum. [10]
Angiography
Superior mesenteric angiography may be helpful in patients presenting with acute GI bleeding and is effective when blood loss exceeds 0.5 mL/min.
Computed tomography
Computed tomography (CT), including multidetector CT (MDCT), may be useful in the assessment of Meckel diverticulum and its complications. [11, 12, 13]
Endoscopy
In a study that included 21 pediatric patients with bloody diarrhea, Qi et al found double-balloon enteroscopy (DBE) to be a potentially useful tool for diagnosing Meckel diverticulum and guiding subsequent minimally invasive treatment. [14]
A European multicenter retrospective study by Baltes et al examined the use of small-bowel capsule endoscopy (SBCE) in 69 patients with Meckel diverticulum (median age, 32 y; male-to-female ratio, 3:1). [15] The most common findings were the double-lumen sign and a visible diverticular entrance, sometimes in conjunction with ulcerative lesions.
Indications for Surgery
Symptomatic Meckel diverticulum
Absolute indications for resection in Meckel diverticulum are hemorrhage, intestinal obstruction, diverticulitis, and umbilicoileal fistulas. [16]
Incidentally discovered Meckel diverticulum
When a Meckel diverticulum is incidentally discovered at laparoscopy or laparotomy, the surgeon must decide whether to resect. Most surgeons generally do not resect a diverticulum with a wide mouth. However, a diverticulum with a narrow neck, which may obstruct or twist, can be easily resected at the neck without the need for segmental resection. A diverticulum deemed abnormal because of inflammation, thickening, or intramural pathology should be resected, with the decision for local or segmental resection based on the pathology. [7]
In 1976, Soltero and Bill reported that the lifetime risk of complications from Meckel diverticulum was 4.2% and that the risk decreased with age. [17] Their data indicated that 800 asymptomatic diverticula would have to be removed to save the life of one patient. On that basis, they opposed surgical excision.
Miltiadis et al stated that resection of incidentally found Meckel diverticulum protected patients from future surgery caused by complications of Meckel diverticulum. This strategy could help reduce morbidity and mortality, especially in elderly patients.
Cullen et al reported that prophylactic diverticulectomy is warranted to eliminate the possibility of future deaths. [4] As a result, they advocated diverticulectomy for asymptomatic disease even in the older age group.
Overall, selected cases of incidentally discovered diverticula in adults and most asymptomatic diverticula found in children [18] may be removed. Resection is recommended in the following cases:
-
Patients younger than 40 years
-
Diverticula longer than 2 cm
-
Diverticula with narrow necks
-
Diverticula with fibrous bands
-
Suspected ectopic gastric tissue
-
Inflamed, thickened diverticula
Removal of a healthy diverticulum in the presence of peritonitis, Crohn disease, ulcerative colitis, or any other complication that would militate against resection is not advised.
Resection of Diverticulum
Surgical dissection and excision depend on the evident pathology. In asymptomatic Meckel diverticulum, excision is generally performed if the neck of the diverticulum is narrow or if stasis is present. Tangential excision with suture closure of the base is performed. In complicated cases, the diverticulum must be resected. (See the image below.)
Four possible surgical procedures may be considered, as follows:
-
Diverticulectomy [19] with suture closure of the base
-
Wedge resection of the intestinal wall containing the diverticulum with suture closure
-
Segmental resection of the intestine, including the diverticulum, and end-to-end anastomosis
-
Division of the fibrous band, with or without diverticulectomy
A survey using data from the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) found no significant differences in outcomes between patients with Meckel diverticulum who were treated by means of diverticulectomy and those who were treated by means of intestinal resection. [20] Intestinal resection was associated with a slightly longer operating time. The authors recommended that the choice between the two approaches be individualized in accordance with each patient's clinical situation.
Preoperative, intraoperative, and postoperative management of Meckel diverticulum follows the general principles of abdominal surgery and includes the use of perioperative antibiotics. Additional surgical considerations include the following:
-
Hemorrhage - In cases of hemorrhage, wedge or segmental resection ensures adequate excision of the part containing gastric and ulcerated ileal mucosa
-
Intestinal obstruction - In cases of intestinal obstruction, the viability of the bowel wall delineates the extent of excision
-
Segmental resection - This is advised in children with broad-based diverticula in whom the risk of ileal stenosis is greater if diverticulectomy or wedge resection is performed
-
Umbilical sinus and fistula - These may necessitate excision of the umbilicus
-
Meckel diverticulitis - Because Meckel diverticulitis often mimics appendicitis, examine the distal ileum for diverticulitis when the appendix is discovered to be normal during exploration for suspected appendicitis
Principles of surgical treatment include the following:
-
Ensuring adequate blood supply to the resectional margins
-
Recognition of bowel viability
-
Awareness of suture-line tension
-
Alertness to the potential for intestinal stenosis due to narrowing
Handsewn technique versus stapling
All procedures may be carried out either by handsewn technique or by stapling, depending on the preference of the surgeon. Stapling enables faster resection of a Meckel diverticulum without the need to open the bowel's lumen, thus avoiding potential septic and postoperative complications. Meckel diverticulum, which fits well into the stapling device, is easy to remove, and removal has a low complication rate, especially when the diverticulum was found incidentally.
Laparoscopic management
Laparoscopic techniques are increasingly being used for Meckel diverticulectomy and intestinal resection. [19, 21, 22, 23] With advances in technology, minimally invasive therapeutic interventions, such as intracorporeal resection or laparoscopic-assisted extracorporeal resection, [24] can easily be performed. Laparoscopic management of Meckel diverticulum has largely been limited to symptoms of abdominal pain and GI bleeding. For symptoms of obstruction, diagnostic laparoscopy is not recommended, because of difficulties in establishing pneumoperitoneum. [25]
A retrospective comparative study by Ezekian et al used data from the NSQIP-Pediatric (NSQIP-Ped) database to compare current practice patterns and outcomes of laparoscopic resection vs open laparotomy for Meckel diverticulum in children. [26] Primary outcomes were length of stay (LOS), readmission rate, and 30-day mortality; secondary outcomes included operating time, anesthesia time, postoperative complications, and reoperation rate. The two approaches were found to have equivalent outcomes.
Treatment Complications
How best to manage a Meckel diverticulum in an asymptomatic patient is controversial. The risk of postoperative complications following excision of an incidental diverticulum has been reported to be as high as 8%.
Symptomatic patients have a 10-12% incidence of early postoperative complications, such as ileus, suture-line or anastomotic leakage, intra-abdominal abscess, and pulmonary embolism.
Late postoperative complications occur in 6-8% of patients and primarily consist of small-bowel obstruction due to intestinal adhesions. The reported mortality for surgery in symptomatic patients is 2-5%.
With incidental diverticulectomy for asymptomatic disease, the morbidity is 2%, the late postoperative complication rate is 2%, and the mortality is 1%.
-
Ileal (Meckel) diverticula and other remnants of yolk stalk. Section of ileum and diverticulum with ulcer.
-
Diverticulum connected to umbilicus by fibrous cord.
-
Umbilicoileal fistula resulting from persistence of entire intra-abdominal portion of yolk stalk.
-
Vitelline cysts at umbilicus and in fibrous remnant of yolk stalk.
-
Umbilical sinus resulting from persistence of yolk stalk near umbilicus.
-
Yolk stalk has persisted as fibrous cord connecting ileum with umbilicus. Persistent vitelline artery extends along fibrous cord to umbilicus.
-
Preoperative CT scan of abdomen in 14-year-old child, showing intestinal obstruction due to Meckel diverticulum.
-
Intraoperative photograph of Meckel diverticulum.
-
Specimen of Meckel diverticulum (mucosal surface) showing gastric mucosa.