Background
Thymoma originates within the epithelial cells of the thymus, a lymphoid organ located in the anterior mediastinum. This organ is located behind the sternum in front of the great vessels; it reaches its maximum weight at puberty and undergoes involution thereafter.
In early life, the thymus is responsible for the development and maturation of cell-mediated immunologic functions. The thymus is composed predominantly of epithelial cells and lymphocytes. Precursor cells migrate to the thymus and differentiate into lymphocytes. Most of these lymphocytes are destroyed, with the remainder of these cells migrating to tissues to become T cells.
A relation between myasthenia gravis (MG) and thymomas was determined incidentally in 1939, when Blalock et al reported the first excision of a thymic cyst in a 19-year-old girl with MG. [1] This patient achieved long-term remission; therefore, thymectomy became the definitive therapy for treatment of generalized MG.
No clear histologic distinction between benign and malignant thymomas exists. The propensity of a thymoma to be malignant is determined by the invasiveness of the thymoma. Malignant thymomas can invade the vasculature, lymphatics, and adjacent structures within the mediastinum. The 15-year survival rate is 12.5% for a person with an invasive thymoma and 47% for a person with a noninvasive thymoma. Death usually occurs from cardiac tamponade or other cardiorespiratory complications.
Anatomy
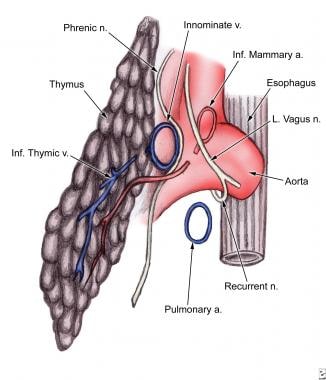
The thymus gland is located behind the sternum, in front of the great vessels and the pericardium; it can extend laterally to the phrenic nerves (see the images below). The main blood supply is from the internal thoracic arteries; however, the gland also is supplied with blood by the inferior thyroid and pericardiophrenic arteries.
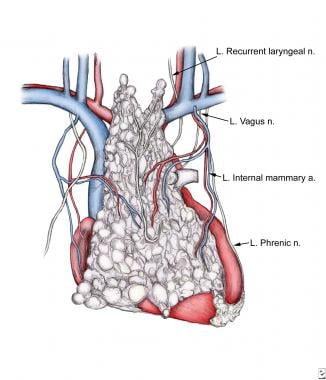 Anatomy of thymus, with emphasis on blood supply and relation to recurrent laryngeal and phrenic nerves.
Anatomy of thymus, with emphasis on blood supply and relation to recurrent laryngeal and phrenic nerves.
Etiology
The etiology of thymomas has not been elucidated; however, these lesions have been associated with various systemic syndromes. As many as 30-40% of patients who have a thymoma experience symptoms suggestive of MG. An additional 5% of patients who have a thymoma have other systemic syndromes, including red cell aplasia, dermatomyositis, systemic lupus erythematosus (SLE), Cushing syndrome, and syndrome of inappropriate antidiuretic hormone secretion (SIADH).
Epidemiology
Thymoma is the most common neoplasm of the anterior mediastinum, accounting for 20-25% of all mediastinal tumors and 50% of anterior mediastinal masses. Its peak incidence occurs in the fourth and fifth decades of life; the mean age of patients is 52 years. No sexual predilection exists.
Prognosis
The prognosis is worse for patients with symptomatic thymomas because these patients are more likely to have a malignant thymoma. The single most important factor predicting the outcome of patients with thymomas is evidence of invasion. Histologic characteristics, such as microscopic capsular invasion, should be assessed. [2] The surgeon should perform a gross inspection. Cellular characteristics are inconsequential because they have no impact on patient treatment.
Because of the well-documented propensity for late recurrences, long-term survival should be considered in terms of a 10-year follow-up after treatment of the thymoma. A study conducted by the Memorial Sloan-Kettering Cancer Center reported 5-year and 10-year survival rates for various stages of thymomas (see Table 1 below). [3]
Table 1. Survival of Thymoma by Stage: Memorial Sloan-Kettering Experience (Open Table in a new window)
Stage |
5-Year Survival |
10-Year Survival |
I |
90% |
80% |
II |
90% |
80% |
III |
60% |
30% |
IV |
Less than 25% |
N/A |
Thymomas are associated with the development of second malignancies. A review of the Surveillance, Epidemiology, and End Results (SEER) database of thymoma cases in the United States (1973-1988) identified 849 cases, of which 66 had second malignancies. There was an excess occurrence of non-Hodgkin lymphoma and soft-tissue sarcoma but of no other specific cancers. Notably, an increase in digestive system cancers (colon/rectum, stomach, esophagus, liver/biliary tract) occurred; however, these increases were not statistically significant.
-
Anatomy of thymus, with emphasis on blood supply and relation to recurrent laryngeal and phrenic nerves.
-
Lateral view of thymus. Thymic arteries are derived from adjacent internal mammary arteries; inferior thymic vein empties into innominate vein. Thymus gland's surrounding vascular and neural structures may be invaded during spread of thymoma.
-
CT scan clearly illustrates mass in right anterolateral mediastinum.