Practice Essentials
Pancreatic pseudocysts (see the image below) are best defined as localized fluid collections that are rich in amylase and other pancreatic enzymes, that have a nonepithelialized wall consisting of fibrous and granulation tissue, and that usually appear several weeks after the onset of pancreatitis. They are to be distinguished from acute fluid collections, organized necrosis, and abscesses.
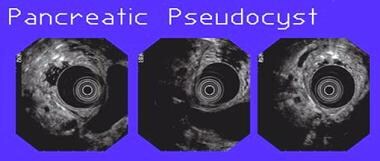 Three views of a pancreatic pseudocyst noted during endoscopic ultrasound. The concentric rings in the center of the images are produced by the ultrasound transducer in the stomach. The cyst is observed as the large hypoechoic structure adjacent to the transducer.
Three views of a pancreatic pseudocyst noted during endoscopic ultrasound. The concentric rings in the center of the images are produced by the ultrasound transducer in the stomach. The cyst is observed as the large hypoechoic structure adjacent to the transducer.
Signs and symptoms
No specific set of symptoms is pathognomonic of pseudocysts; however, the following are suggestive:
-
Persistent abdominal pain, anorexia, or abdominal mass after pancreatitis
-
Jaundice or sepsis from an infected pseudocyst (rare)
Physical examination findings are of limited sensitivity but may include the following:
-
Tender abdomen
-
Palpable mass in the abdomen
-
Peritoneal signs suggesting rupture of the cyst or infection
-
Fever
-
Scleral icterus
-
Pleural effusion
See Presentation for more detail.
Diagnosis
Laboratory studies that may be considered include the following:
-
Serum amylase and lipase levels (limited utility) – Often elevated but may be within the reference ranges
-
Serum bilirubin and liver function tests (limited utility) – Sometimes elevated if the biliary tree is involved
-
Cyst fluid analysis – Carcinoembryonic antigen (CEA) and CEA-125 (low in pseudocysts and elevated in tumors); fluid viscosity (low in pseudocysts and elevated in tumors); amylase (usually high in pseudocysts and low in tumors)
Imaging studies that may be helpful include the following:
-
Abdominal ultrasonography – Not the study of choice for establishing a diagnosis
-
Abdominal computed tomography (CT) – The criterion standard for pancreatic pseudocysts
-
Endoscopic retrograde cholangiopancreatography (ERCP) – Not necessary for diagnosis but useful in planning drainage strategy.
-
Magnetic resonance imaging (MRI) – Not necessary for diagnosis but useful in detecting a solid component to the cyst and in differentiating between organized necrosis and a pseudocyst
-
Endoscopic ultrasonography – Not necessary for diagnosis but very important in planning therapy, particularly if endoscopic drainage is contemplated
See Workup for more detail.
Management
Most pseudocysts resolve without interference and only require supportive care. For some, drainage is indicated. Indications for drainage include the following:
-
Complications
-
Symptoms
-
Concern about possible malignancy
Drainage options are as follows:
-
Percutaneous catheter drainage – The procedure of choice for infected pseudocysts; although recurrence and failure rates are high, it may be a good temporizing measure
-
Endoscopic drainage, either transpapillary (via ERCP) or transmural – The complication rate appears to decrease and efficacy to increase with experience
-
Surgical drainage – The criterion standard; internal drainage is the procedure of choice, but laparoscopic drainage has yielded good results in some cases
No medications are specific to the treatment of pancreatic pseudocysts. Antibiotics and octreotide may be useful adjuncts in some cases.
See Treatment and Medication for more detail.
Background
Pseudocysts are best defined as localized fluid collections that are rich in amylase and other pancreatic enzymes, that have a nonepithelialized wall consisting of fibrous and granulation tissue, and usually appears several weeks after the onset of pancreatitis. [1]
These characteristics contrast with those of acute fluid collections, which are more evanescent and are serosanguinous inflammatory reactions to acute pancreatitis. These collections are noted in moderate-to-severe pancreatitis. Acute fluid collections usually have an irregular shape and lack a well-defined wall. In general, they resolve in about 65% of cases.
Two other types of fluid collection should be considered. First, an organized necrosis is actually devitalized pancreatic tissue that appears cystlike on computed tomography (CT) scans, but it appears to be solid on other imaging modalities. Second, an abscess is an infected area of necrosis or fluid.
Acute or, rarely, chronic pancreatitis or abdominal trauma causes pseudocysts. If no history of pancreatitis or trauma exists, the diagnosis must be carefully confirmed.
Single or multiple fluid collections that look like cysts on pancreatic imaging are often observed during acute pancreatitis. Because of increasing sensitivity of imaging modalities and improvements in technology providing enhanced therapeutic abilities, the question arises as to when and whether drainage should be performed and what modality should be used to drain the cysts. [2] Strictly defining the type of fluid collection is very important when reviewing pancreatic fluid collections. The therapeutic approach is different depending on the type of collection.
Pathophysiology
Pancreatic pseudocysts can be single or multiple. Multiple cysts are more frequently observed in patients with alcoholism, and they can be multiple in about 15% of cases. Size varies from 2-30 cm. About one third of pseudocysts manifest in the head of the gland, and two thirds appear in the tail. The fluid in pseudocysts has been well characterized as clear or watery, or it can be xanthochromic. The fluid in pseudocysts usually contains very high amounts of amylase, lipase, and trypsin, though the amylase level may decrease over time.
The pathogenesis of pseudocysts seems to stem from disruptions of the pancreatic duct due to pancreatitis and extravasation of the enzymatic material. Two thirds of patients with pseudocysts have demonstrable connections to the pancreatic duct. In the other third, an inflammatory reaction is supposed to have sealed the connection so that it is not demonstrable. The cause of pseudocysts parallels the cause of acute pancreatitis; 75-85% of cases are caused by alcohol or gallstone disease–related pancreatitis. In children, pseudocysts and trauma are frequently associated.
Epidemiology
Sex- and age-related demographics
The male predominance in the incidence of pseudocysts mirrors the male predominance in the incidence of pancreatitis.
Pseudocysts may occur after pancreatitis in any age group. In children, pseudocysts are most likely observed after abdominal trauma. In elderly persons, care should be taken not to confuse cystic neoplasms with pseudocysts.
Prognosis
Most pseudocysts resolve without interference, and patients do well without intervention. The outcome is much worse for patients who develop complications or who have the cyst drained. The presence of pancreatic necrosis is a poor prognostic sign.
The failure rate for drainage procedures is about 10%, the recurrence rate is about 15%, and the complication rate is 15-20%.
Complications
Bleeding is the most feared complication and is caused by the erosion of the pseudocyst into a vessel. Consider the possibility of bleeding in any patient who has a sudden increase in abdominal pain coupled with a drop in hematocrit level or a change in vital signs. Therapy is emergent surgery or angiography with embolization of the bleeding vessel.
Do not perform a percutaneous or endoscopic drainage procedure under any circumstances in patients with suspected bleeding into a pseudocyst. Consider the possibility of infection of the pseudocyst in patients who develop fever or an elevated WBC count. Treat infection with antibiotics and urgent drainage.
GI obstruction, manifesting as nausea and vomiting, is an indication for drainage.
The pseudocyst can also rupture. A controlled rupture into an enteric organ occasionally causes GI bleeding. On rare occasions, a profound rupture into the peritoneal cavity causes peritonitis and death.
Patient Education
Patients who are being managed expectantly must be educated about the warning signs for potential complications (eg, abdominal pain, fever), which may indicate bleeding, infection, or pseudocyst rupture.
For patient education resources, see the Digestive Disorders Center, as well as Pancreatitis and Abdominal Pain in Adults.
-
Three views of a pancreatic pseudocyst noted during endoscopic ultrasound. The concentric rings in the center of the images are produced by the ultrasound transducer in the stomach. The cyst is observed as the large hypoechoic structure adjacent to the transducer.
-
These photographs show the endoscopic view of transpapillary pseudocyst drainage in a patient with pancreas divisum and a pseudocyst that communicates with the pancreatic duct. The image on the left shows the ampullary area. The middle image shows a wire placed in the minor papilla into the dorsal pancreatic duct. The right image shows a stent in place in the minor papilla.








