Practice Essentials
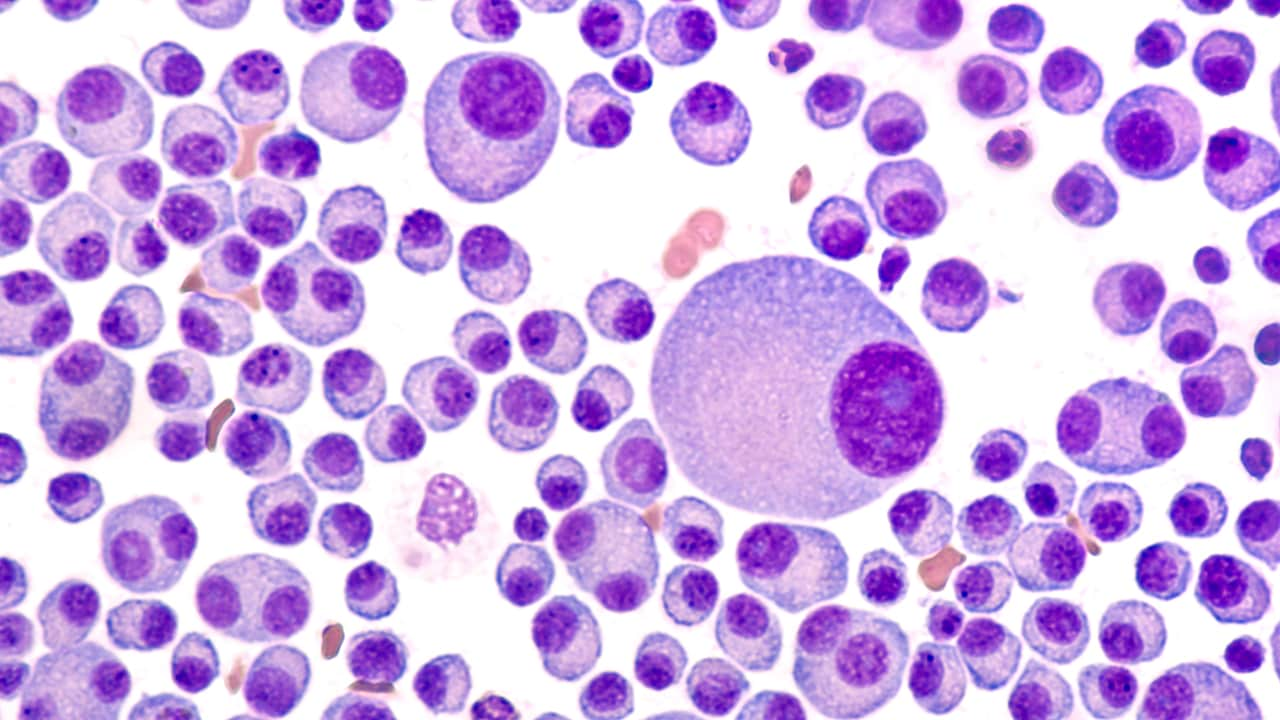
Solitary plasmacytoma (SP) is an early-stage plasma cell malignancy that is in between monoclonal gammopathy of undetermined significance (MGUS) and multiple myeloma (MM) along the spectrum of plasma cell disorders. [1] A plasmacytoma is a discrete, solitary mass of neoplastic monoclonal plasma cells. SPs can be divided into 2 groups according to location:
-
Solitary bone plasmacytoma (SBP) – These occur most commonly in the vertebrae
-
Extramedullary plasmacytoma (EMP) – These encompass all nonosseus SPs; they can occur in any soft tissue but the upper airway tract, including the sinuses, is the most common site.
For a diagnosis of SP, the International Myeloma Working Group (IMWG) requires all four of the following criteria be met [2] :
-
Biopsy-proven solitary lesion of bone or soft tissue with evidence of clonal plasma cells
-
Normal bone marrow with no evidence of clonal plasma cells
-
Normal skeletal survey and MRI (or CT) of the spine and pelvis, except for the primary solitary lesion
-
Absence of end-organ damage, such as CRAB (hypercalcemia, renal failure, anemia, and osteolytic bone lesions), that can be attributed to a lympho-plasma cell proliferative disorder
Patients with an apparent SP who have clonal marrow involvement of less than 10% are considered to have SP with minimal marrow involvement. SP with 10% or greater clonal plasma is diagnosed as multiple myeloma.
SP is a highly radiosensitive tumor and most patients undergo radiation therapy as the first line of treatment, resulting in an excellent local control rate. [3] The risk of recurrence or progression to myeloma within 3 years is approximately 10% for patients with SP; for those who have SP with minimal marrow involvement, the risk is 20% for those with a soft tissue lesion and 60% for those with a bone lesion. [2]
For patient education information, see the Multiple Myeloma Resource Center.
Pathophysiology
A plasmacytoma can arise in any part of the body. A solitary bone plasmacytoma (SBP) arises from the plasma cells located in the bone marrow, whereas an extramedullary plasmacytoma (EMP) is thought to arise from plasma cells located in mucosal surfaces. [4] Both represent a different group of neoplasms in terms of location, tumor progression, and overall survival rate. [5, 6] Some authors suggest that SBPs represent marginal cell lymphomas with extensive plasmacytic differentiation. [6] Both SBP and extramedullary plasmacytoma (EMP) do, however, share many of the biologic features of other plasma cell disorders.
Cytogenetic studies show recurrent losses in chromosome 13, chromosome arm 1p, and chromosome arm 14q, as well as gains in chromosome arms 19p, 9q, and 1q. [7] Interleukin-6 (IL-6) is still considered the principal growth factor in the progression of plasma cell disorders. [8]
The specific roles of surface markers, adhesion molecules, and angiogenesis in solitary plasmacytoma need to be studied further.
In a study by Kumar et al, high-grade angiogenesis in SBP was associated with increased progression to multiple myeloma and shorter progression-free survival. Some have postulated that SBP may be considered an intermediate step in the evolution from monoclonal gammopathy of undetermined significance to multiple myeloma. [8, 9]
Etiology
No definite cause has been found for solitary bone plasmacytoma (SBP). Because of its presentation in the mucosa of the aerodigestive tract (> 80%), the etiology of extramedullary plasmacytoma (EMP) may be related to chronic stimulation of inhaled irritants or viral infection. [10]
Epidemiology
Solitary plasmacytoma (SP) has an annual incidence of less than 450 cases in the United States. [3] Solitary bone plasmacytoma (SBP) affects fewer than 5% of patients with plasma cell disorders. [11, 8] Extramedullary plasmacytoma (EMP) represents approximately 3% of all plasma cell neoplasms. [12] In the United States during 2003‐2016, overall incidence rates in adults were 0.45 per 100,000 persons for SP and 0.09 per 100,000 persons for extramedullary plasmacytoma. [13]
Population studies have reported a male predominance in the SP with a male-to-female ratio of 1.6:1. In studies focusing primarily on SBP, the male-to-female ratio ranges from 1.5–2.4:1. Among EMP patients, a 3:1 male predominance has been reported in sites involving upper airway tract. [3]
SP primarily affects adults over 40 years old, and its incidence increases with age. [3] The median age of patients with either SBP or EMP is 55 years. This median age is 10 years younger than in patients with multiple myeloma. [14, 4, 15, 16, 17]
Prognosis
A review by Sharpley et al of 66 patients with solitary plasmacytoma found that with a median follow-up of 53.6 months the 5-year overall survival was 90.7% (95% confidence index [CI] 79–96%). The median progression-free survival (PFS) from diagnosis was 61 months. The cumulative incidence of progression to multiple myeloma at 5 years was 49.9% (95% CI 35.6–62.6%) and was significantly higher with bone plasmacytoma (47.2%, 95% CI 31.9–61.1%), than extramedullary plasmacytoma (8.3%, 95%CI 0.4–32.3%, Gray test P = 0.0095). [18]
Solitary bone plasmacytoma (SBP)
Solitary bone plasmacytoma (SBP) progresses to multiple myeloma at a rate of 65-84% at 10 years and 65-100% at 15 years. The median onset of conversion to multiple myeloma is 2-5 years with a 10-year disease-free survival rate of 15-46%. The overall median survival time is 10 years. [15]
Kyle described the following 3 patterns of treatment failure [19] :
-
Development of multiple myeloma (54%)
-
Local recurrence (11%)
-
Development of new bone lesions in the absence of multiple myeloma (2%)
Prognostic features for conversion of SBP to multiple myeloma, although controversial, include the following [20, 21, 22] :
-
Lesion size of at least 5 cm
-
Patient age 40 years and older
-
High M protein levels
-
Persistence of M protein after treatment
-
Spine lesions
In a study by Wilder et al, 10-year myeloma-free survival in patients whose M protein resolved within 1 year after radiation therapy was 91%, versus 29% in patients whose M-protein persisted beyond that time. [23]
Yadav et al reported that on fluorescence in situ hybridization (FISH), the presence of del(17p), t(14;16), t(4;14), or +1q (gain or amplification) in the clonal plasma cells of patients with SBP indicated high risk of progression to multiple myeloma. Median time to progression in patients with high-risk FISH findings was 8 months, compared with 42 months in patients without those findings (P< 0.001). On multivariate analysis, high-risk FISH results were the only significant predictor for shorter time to progression, independent of minimal marrow involvement and an abnormal serum free light chain ratio at diagnosis. [24]
As with some other cancers, marital status has been identified as a prognostic factor in SBP. Married patients may have a better prognosis because they receive better financial, emotional support, and life care from their partners or family members. [25, 26]
Extramedullary plasmacytoma (EMP)
Patients with EMP have a 5-year survival rate of about 82% and 10-year disease-specific survival rate greater than 50%. [12] The rate of progression to multiple myeloma is lower than in SBP, ranging from 11% to 30% at 10 years. [15] Patients with EMP that progressed to multiple myeloma had a 5-year survival rate of 100%, compared with 33% for those with SBP. [27] In a review of 721 cases by Alexiou and colleagues, after treatment, approximately 65% of patients were free of recurrence and did not progress to multiple myeloma, 22% experienced recurrence, and 15% of cases evolved to multiple myeloma. [16]
In one study, local control following radiation therapy was achieved in 83% of patients with low-grade histology versus 17% of patients with intermediate- to high-grade tumors. [28]