Background
Trichinosis (trichinellosis) results from infection by a parasitic nematode belonging to the genus Trichinella. Trichinosis, although often unrecognized and underreported, has been an important disease in humans for thousands of years. An estimated 10,000 cases occur worldwide annually. [1] Virtually all mammals are susceptible to infection; however, humans are especially prone to developing clinical disease via foodborne infection. [2] Humans are infected when they ingest inadequately cooked meat that contains larvae of Trichinella species, usually Trichinella spiralis, which is present mainly in wild game meat or pork. [1] Symptomatic infections characterized by diarrhea, myositis, fever, and periorbital edema develop when large numbers of larvae are ingested. [3]
Species of Trichinella responsible for the infection are widely geographically distributed (see table), with habitats including the Arctic, temperate lands, and the tropics. [4]
Table 1. Biologic and Zoogeographic Features of Trichinella Species (Open Table in a new window)
Species |
Distribution |
Major Hosts |
Reported from Humans |
T spiralis |
Cosmopolitan |
Domestic pigs, wild mammals |
Yes |
T britovi |
Eurasia/Africa |
Wild mammals |
Yes |
T murrelli |
North America |
Wild mammals |
Yes |
T nativa |
Arctic/subarctic, Palaearctic |
Bears, foxes, walrus, seals, and wolves+ |
Yes |
T nelsoni |
Equatorial Africa |
Hyenas, felids |
Yes |
T pseudospiralis * |
Cosmopolitan |
Wild mammals, birds |
Yes |
T papuae * |
Papua New Guinea, Thailand, and Cambodia+ |
Pigs, crocodiles, and turtles+ |
Yes |
| T patagoniensis+ | South America+ | Cougars+ | No+ |
T zimbabwensis * |
East and South Africa |
Crocodiles, lizards, lions |
No |
* Nonencapsulating types |
|
|
|
Reprinted from Adv Parasitol, Vol 63, Murrell KD, Pozio E, Systematics and epidemiology of Trichinella, pg 367, 2006, with permission from Elsevier.
+ [5]
Pathophysiology
Trichinella species require 2 hosts to maintain their life cycles. After development in a first host, they spread to the next through ingestion of infected flesh, as opposed to the traditional arthropod intermediate host. Trichinella species have 3 major life cycles in nature: pig-to-pig, rat-to-rat, and by carnivorous or omnivorous animals in the wild. Rats and pigs are the animals most commonly associated with trichinosis; however, depending on the region, walruses, seals, bears, polar bears, cats, raccoons, wolves, and foxes also may be infected. The life cycle of Trichinella species parasite is depicted in the image below.
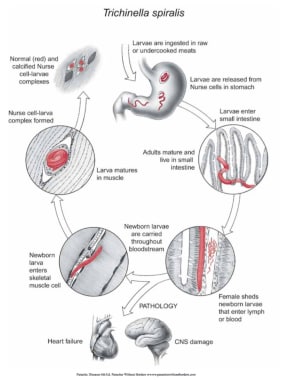 Life cycle of Trichinella in humans. Courtesy of Dickson Despommier, PhD, and Daniel Griffin, MD, PhD, Parasitic Diseases, 6th Ed, published by Parasites Without Borders (www.parasiteswithoutborders.com).
Life cycle of Trichinella in humans. Courtesy of Dickson Despommier, PhD, and Daniel Griffin, MD, PhD, Parasitic Diseases, 6th Ed, published by Parasites Without Borders (www.parasiteswithoutborders.com).
As a foodborne illness, the life cycle begins when raw or inadequately cooked meat that contains viable larvae inside a cyst wall (nurse cells) is consumed. The acidic environment in the host's stomach releases the larvae from the cyst wall. The free larvae migrate into the small intestine and attach to and penetrate the mucosa at the base of the villi. After 4 molts and over a period of 30-36 hours, they develop into adult worms and become obligate intracellular organisms. The adult male measures 1.5 X 0.05 mm, and the adult female measures 3.5 X 0.06 mm. Approximately 5 days after infection, the female begins shedding live newborn larvae that measure 80 µm x 7 µm (L1 stage). The female remains in the intestine for 4 weeks, releasing up to 1500 larvae. After an adequate inflammatory response develops in the intestine, the female is eventually expelled in the feces.
The newborn larvae enter the lymphatics and blood circulatory system and migrate to well-vascularized striated skeletal muscle. The parasite has a predilection for the most metabolically active muscle groups; therefore, the most frequently parasitized muscles include the tongue; the diaphragmatic, masseteric, intercostal, laryngeal, extraocular, nuchal, intercostal, and pectoral muscles; the deltoid; the gluteus; the biceps; and the gastrocnemius. In tissues other than skeletal muscle, such as the myocardium and brain, the parasites soon disintegrate, causing intense inflammation, and are then reabsorbed.
The larvae continue to grow over the next 2-3 weeks until they reach the fully developed L1 infective stage, when they increase in size up to 10-fold. The adult worms are viviparous. The larvae will encyst; it will coil and develop a surrounding cyst wall or nurse cell to help it survive harsher conditions such as acidic environments (except for T pseudospiralis, which does not encyst). The complete cycle takes 17-21 days. The larvae within the cyst wall reach an average size of 400 X 260 µm; however, lengths of 800-1000 µm have been described. The nurse cell–L1 complex may persist for 6 months to several years before calcification and death occur. The Trichinella life cycle is complete when a compatible host ingests the infected muscle (see images below).
 Trichinella nurse cell. Courtesy of Dickson Despommier, PhD, and Daniel Griffin, MD, PhD, Parasitic Diseases, 6th Ed, published by Parasites Without Borders (www.parasiteswithoutborders.com).
Trichinella nurse cell. Courtesy of Dickson Despommier, PhD, and Daniel Griffin, MD, PhD, Parasitic Diseases, 6th Ed, published by Parasites Without Borders (www.parasiteswithoutborders.com).
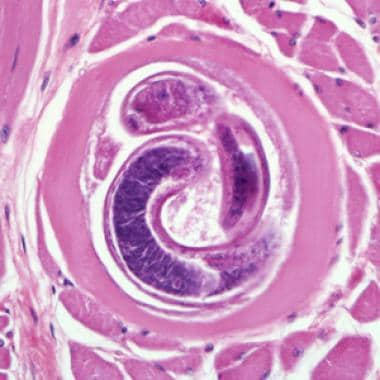 Encysted larvae of Trichinella species in muscle tissue, stained with hematoxylin and eosin (H&E). The image was captured at 400X magnification. Courtesy of the US Centers for Disease Control and Prevention (http://www.dpd.cdc.gov/dpdx/HTML/Trichinellosis.htm).
Encysted larvae of Trichinella species in muscle tissue, stained with hematoxylin and eosin (H&E). The image was captured at 400X magnification. Courtesy of the US Centers for Disease Control and Prevention (http://www.dpd.cdc.gov/dpdx/HTML/Trichinellosis.htm).
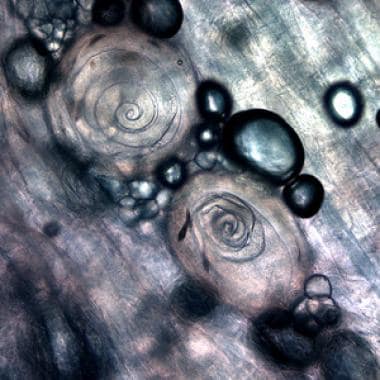 Trichinella larvae, in pressed bear meat, partially digested with pepsin. Courtesy of the US Centers for Disease Control and Prevention ((http://www.dpd.cdc.gov/dpdx/HTML/Trichinellosis.htm).
Trichinella larvae, in pressed bear meat, partially digested with pepsin. Courtesy of the US Centers for Disease Control and Prevention ((http://www.dpd.cdc.gov/dpdx/HTML/Trichinellosis.htm).
 Larvae of Trichinella from bear meat. Courtesy of the US Centers for Disease Control and Prevention (http://www.dpd.cdc.gov/dpdx/HTML/Trichinellosis.htm).
Larvae of Trichinella from bear meat. Courtesy of the US Centers for Disease Control and Prevention (http://www.dpd.cdc.gov/dpdx/HTML/Trichinellosis.htm).
The intensity and frequency of exposure to infected meat determine the severity of the disease. The degree of infection is categorized as light (0-10 larvae ingested), moderate (50-500 larvae ingested), and severe (>1000 larvae ingested).
Epidemiology
Frequency
United States
National surveillance has documented a decline in the reported incidence of trichinosis in the United States since 1947, the first year nationwide data were collected systematically. Between 2011 and 2015, 80 reported cases occurred in 24 states and the District of Columbia. Of these cases, 57 (71%) had a confirmed or suspected source, 25 of which involved bear meat (44%), 13 involved wild boar meat (23%), and 9 involved unspecified pork (16%). [6] One case was not linked to consumption of meat but to consumption of residual larvae on a preparation table. [7] Often, infection resulted from ingestion of the meat sources, denoting that trichinosis could be considered a foodborne illness.
Trichinella also is tied to geopolitical factors, including movement of persons, livestock, and food (especially including Mexico and Asia).The percentage of infected domestic swine in the United States is 0.001%; however, one autopsy study documented a 4% incidence of old infection. In 2008, an outbreak in Northern California affected 38 individuals who ate black bear infected with T murrelli. [8] Data also have shown the presence of T murrelli in raccoons and coyotes. [9]
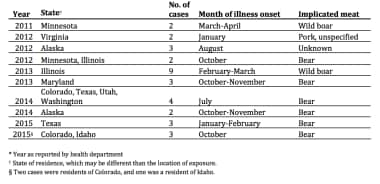 Epidemiology of trichinellosis in the US. Courtesy of Centers for Disease Control and Prevention (CDC) (https://www.cdc.gov/parasites/trichinellosis/resources/trichinellosis_surveillance_summary_2015.pdf).
Epidemiology of trichinellosis in the US. Courtesy of Centers for Disease Control and Prevention (CDC) (https://www.cdc.gov/parasites/trichinellosis/resources/trichinellosis_surveillance_summary_2015.pdf).
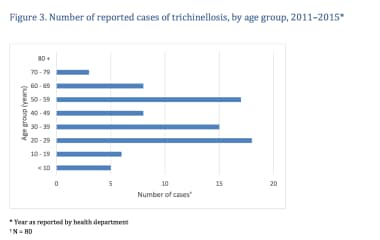
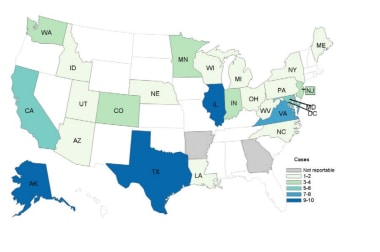 Reported cases of trichinellosis 2011-2015. Courtesy of Centers for Disease Control and Prevention (CDC) (https://www.cdc.gov/parasites/trichinellosis/resources/trichinellosis_surveillance_summary_2015.pdf).
Reported cases of trichinellosis 2011-2015. Courtesy of Centers for Disease Control and Prevention (CDC) (https://www.cdc.gov/parasites/trichinellosis/resources/trichinellosis_surveillance_summary_2015.pdf).
International
In Europe, where pork inspection is mandatory, most cases of trichinosis are associated with horse or wild boar meat. In Latin America and Asia, domestic pork is the chief source of infection. The rate of Trichinella infection in swine in China is as high as 20%. Studies have reported increased rates of trichinosis in former European countries such as Romania and Hungary due to political changes and regional food habits. [10, 11] In addition, the European Centre for Disease Prevention and Control and the European Safety Authority reported 779 human cases of trichinosis in the European Union found in farm animals and wild animals, particularly in the latter. [12]
The worldwide incidence of trichinosis has declined substantially during the past few decades, but outbreaks are still frequent, especially in developing countries. [13, 14] Each year, 10,000 trichinellosis cases are estimated to occur. [1] The estimated death rate is 0.2%. [15]
Mortality/Morbidity
Although Trichinella infections are most likely underreported in the United States, fewer than 25 cases are documented per year, with a very low mortality rate.
Patients with light infection usually are asymptomatic. Those with mild symptoms improve in 2-3 weeks. Symptoms associated with heavy infections may persist for 2-3 months.
Factors that may affect morbidity include the quantity of larvae ingested, the species of Trichinella (most notably T spiralis), and the immune status of the host. Patients succumb to exhaustion, pneumonia, pulmonary embolism, encephalitis, or cardiac failure and/or arrhythmia. Death from trichinosis usually occurs in 4-8 weeks but may occur as early as in 2-3 weeks.
Race
Although Trichinella infections may be related to cultural differences in food cooking and storing methods (eg, the inadequate cooking or freezing of meat), outcomes do not vary based on race among infected individuals.
Culture
A 2017 outbreak involved the consumption of walrus meat in Alaska. [7] The first point of healthcare contact included village healthcare centers, which are primarily used by Alaskan Native populations. Traditional cultural practices, including the hunting of polar bear and walrus, may lead to differential infection rates with Trichinella within Alaska Native communities.
Some studies have found that cultural practices, such as avoidance of pork consumption in Jewish and Muslim communities, may serve as a protective factor against Trichinella infection. [16]
Sex
No differences in the rates of trichinosis between males and females are reported. Pregnant patients have milder trichinosis symptoms than patients who are not pregnant; however, abortions and stillbirths have been reported. Symptoms of trichinosis typically are worse in females who are lactating than in females who are not.
Age
Children appear to be more resistant to Trichinella infection; however, their symptoms may be more intense. Children also have fewer complications and recover more rapidly. The figure below shows the cumulative number of patients with trichinosis in the United States between 2011 and 2015, displayed by sex and age group. During this time period, a total of 80 cases were reported among persons whose age was known. Age was unknown for an additional patient, and sex was unknown for another patient. Of the 80 cases, 51 occurred in males and 29 in females. Among the 53 patients whose age was known, the median age was 37 years (range, 1-71 years).
Prognosis
Severe disease develops in only 5-20% of patients during epidemics.
Patient Education
Adequate cooking and freezing methods prevent trichinosis.
The most effective measure to eradicate Trichinella species is by adequate cooking to kill the parasite. The current recommendation for heating is 160°F (71°C) for all food-borne disease. Trichinella species can typically be killed by adequate cooking to 140°F (60°C) for 2 minutes or 131°F (55°C) for 6 minutes. If no trace of pink in fluid or flesh is found, these temperatures have been reached.
Freezing also is an effective method for killing most species of Trichinella. For a 6-inch piece of meat, the recommended temperatures to kill larvae are as follows:
-
5°F (-15°C) for 20 days
-
-10°F (-23°C) for 10 days
-
-20°F (-29°C) for 6 days
Salting, smoking, or drying the meat does not kill cysts.
Excellent patient education resources regarding the esophagus, stomach, and intestine are available at eMedicineHealth's Digestive Disorders Center. Patient education material specific to diarrhea is found in the article Diarrhea. Patient education material specific to vomiting and nausea is found in the article Vomiting and Nausea.
-
Encysted larvae of Trichinella species in muscle tissue, stained with hematoxylin and eosin (H&E). The image was captured at 400X magnification. Courtesy of the US Centers for Disease Control and Prevention (http://www.dpd.cdc.gov/dpdx/HTML/Trichinellosis.htm).
-
Trichinella larvae, in pressed bear meat, partially digested with pepsin. Courtesy of the US Centers for Disease Control and Prevention ((http://www.dpd.cdc.gov/dpdx/HTML/Trichinellosis.htm).
-
Larvae of Trichinella from bear meat. Courtesy of the US Centers for Disease Control and Prevention (http://www.dpd.cdc.gov/dpdx/HTML/Trichinellosis.htm).
-
The number of cases of trichinellosis by age. Courtesy of Centers for Disease Control and Prevention (CDC) (https://www.cdc.gov/parasites/trichinellosis/resources/trichinellosis_surveillance_summary_2015.pdf).
-
Epidemiology of trichinellosis in the US. Courtesy of Centers for Disease Control and Prevention (CDC) (https://www.cdc.gov/parasites/trichinellosis/resources/trichinellosis_surveillance_summary_2015.pdf).
-
Reported cases of trichinellosis 2011-2015. Courtesy of Centers for Disease Control and Prevention (CDC) (https://www.cdc.gov/parasites/trichinellosis/resources/trichinellosis_surveillance_summary_2015.pdf).
-
Trichinella nurse cell. Courtesy of Dickson Despommier, PhD, and Daniel Griffin, MD, PhD, Parasitic Diseases, 6th Ed, published by Parasites Without Borders (www.parasiteswithoutborders.com).
-
Life cycle of Trichinella in humans. Courtesy of Dickson Despommier, PhD, and Daniel Griffin, MD, PhD, Parasitic Diseases, 6th Ed, published by Parasites Without Borders (www.parasiteswithoutborders.com).