Practice Essentials
Essential thrombocytosis (primary thrombocythemia) is a nonreactive, chronic myeloproliferative disorder in which sustained megakaryocyte proliferation leads to an increase in the number of circulating platelets [1] (see the images below). Mutations in JAK2, CALR, or MPL are found in approximately 90% of patients with essential thrombocytosis.
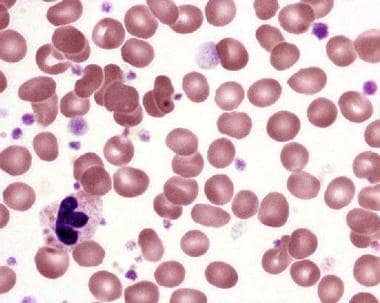 Peripheral blood smear in essential thrombocytosis showing increased platelet numbers. Courtesy Wei Wang, MD, and John Lazarchick, MD; Department of Pathology, Medical University of South Carolina.
Peripheral blood smear in essential thrombocytosis showing increased platelet numbers. Courtesy Wei Wang, MD, and John Lazarchick, MD; Department of Pathology, Medical University of South Carolina.
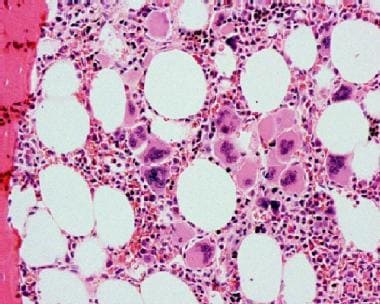 Bone marrow biopsy in essential thrombocytosis showing increased megakaryocytes. Courtesy Wei Wang, MD, and John Lazarchick, MD; Department of Pathology, Medical University of South Carolina.
Bone marrow biopsy in essential thrombocytosis showing increased megakaryocytes. Courtesy Wei Wang, MD, and John Lazarchick, MD; Department of Pathology, Medical University of South Carolina.
Essential thrombocytosis was first described by Epstein and Goedel in 1934, who termed the condition hemorrhagic thrombocythemia. [2, 3] Essential thrombocytosis was traditionally considered a clonal disorder that involved pluripotent stem cells. However, studies have indicated that some patients may have polyclonal hematopoiesis. [4]
Essential thrombocytosis is characterized by the following [5, 6, 7, 8, 9, 10, 11] :
-
A persistently elevated platelet count greater than 450,000/µL
-
Megakaryocytic hyperplasia
-
Splenomegaly
-
A clinical course complicated by thrombotic or hemorrhagic episodes or both
Treatment should be individualized on the basis of risk factors for thrombosis or bleeding. Treatment options range from observation to low-dose aspirin to cytoreductive therapy. In emergencies, plateletpheresis may be useful to achieve a rapid decrease in platelet counts. See Treatment and Medication.
Pathophysiology
Platelet survival is normal in essential thrombocytosis. Instead, the elevated counts result from increased production of platelets by megakaryocytes. The cause of this increase in platelet production remains unclear, but possibilities include the following:
-
Autonomous production
-
Increased sensitivities to cytokines (eg, interleukin-3 [IL-3])
-
Decreased effect of platelet-inhibiting factors (eg, transforming growth factor [TGF] beta)
-
Defects in the accessory cell microenvironment
Bone marrow megakaryocytic precursors (colony-forming unit–megakaryocyte [CFU-Meg]) from patients with essential thrombocytosis form colonies in the absence of exogenous thrombopoietin (Tpo). There is no evidence for mutations in the genes for Tpo, and patients with essential thrombocytosis have normal or even decreased plasma Tpo levels, possibly reflecting increased Tpo clearance due to the elevated circulating platelet mass.
The majority of patients with essential thrombocytosis have mutations in one of three genes: Janus kinase 2 (JAK2), calreticulin (CALR), or myeloproliferative leukemia virus oncogene (MPL). Rare cases involve mutations in the thrombopoietin gene (THPO), which are associated with autosomal dominant hereditary thrombocytosis, and somatic mutations in tet methylcytosine dioxygenase 2 (TET2). [12]
MPL mutations have been associated with only about 3-5% of essential thrombocytosis cases. MPL codes for the thrombopoietin receptor protein, which promotes the growth and proliferation of megakaryocytes. The mutations consist of amino acid substitutions at position 505 in familial cases or 515 in sporadic cases These result in constitutive activation of the thrombopoietin receptor protein. [12]
JAK2 mutations possibly turn the thrombopoietin receptor on permanently, leading to overproduction of megakaryocytes. JAK2 mutation is seen in approximately 50-60% of patients.
Somatic mutations in CALR are detected in peripheral blood in the approximately 25% of essential thrombocythemia cases. CALR mutations are mutually exclusive with JAK2 or MPL mutations.
One study found that patients with JAK2 mutations tend to be older than patients with CALR mutations and to have a higher hemoglobin level and white blood cell count, as well as a lower platelet count and serum erythropoietin level. Risk of thrombosis was twice as high in patients with JAK2 mutations than in those with CALR mutations. Transformation to polycythemia was not observed in patients with CALR mutations, whereas the cumulative risk of polycythemic transformation was 29% at 15 years in those with JAK2 mutations. [13]
The mechanism by which thrombocythemia produces hemorrhage or thrombosis is not well defined. Several defects have been described, including a decrease in aggregation, hyperaggregation, and intracellular concentration of various chemicals. In addition, reports show a decrease in von Willebrand ristocetin cofactor activity and high molecular weight von Willebrand factor multimers. [14, 15] Some reports show patients with an acquired deficiency of antithrombin III, protein C, and protein S. [8]
Epidemiology
Frequency
United States
Clinicians diagnose approximately 6000 cases of essential thrombocytosis (primary thrombocythemia) each year. Some researchers speculate that the incidence rate may be several times higher. A study from southeastern Minnesota reported an incidence of 2.38 cases per 100,000 population per year. [16]
Mortality/Morbidity
Patients with essential thrombocytosis (primary thrombocythemia) have a 10-year survival rate of 64-80%, which may not be significantly different from that of the age-matched general population. Death occurs from thrombotic complications.
Transformation to acute myelogenous leukemia (AML) occurs in 0.6-5% of patients during the first decade and increases significantly in subsequent decades. [17] Risk factors include advanced age, anemia (hemoglobin less than 12 g/dL in females and less than 13.5 g/dL in males), leukocytosis, platelet count of >1,000,000/μL, and sequence variants/mutations involving TP53 and EZH2. [18] Treatment with alkylating agents or radiophosphorus may be associated with higher risk of leukemic transformation.
Morbidity in patients with essential thrombocytosis may involve large-vessel or microvascular thrombosis and bleeding.
Sex
In older patients with essential thrombocytosis, the frequency is similar in both sexes. In younger patients, however, essential thrombocytosis occurs more often in women than in men.
Age
Essential thrombocytosis (primary thrombocythemia) is more frequent in older patients, although younger patients may develop the disease. The median age at diagnosis is 60 years, and perhaps up to 20% of patients are younger than 40 years. The disease is rare in children.
-
Peripheral blood smear in essential thrombocytosis showing increased platelet numbers. Courtesy Wei Wang, MD, and John Lazarchick, MD; Department of Pathology, Medical University of South Carolina.
-
Bone marrow biopsy in essential thrombocytosis showing increased megakaryocytes. Courtesy Wei Wang, MD, and John Lazarchick, MD; Department of Pathology, Medical University of South Carolina.








