Background
High-altitude pulmonary edema (HAPE) is a potentially fatal form of severe high-altitude illness, a type of noncardiogenic pulmonary edema caused by hypoxia. [1] (See the following image.)
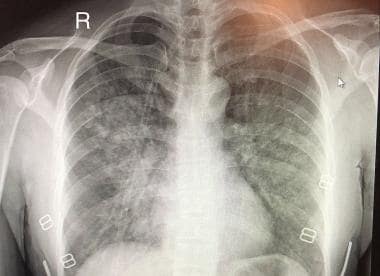 High-altitude pulmonary edema (HAPE). Plain chest x-ray (radiograph) of a patient diagnosed with HAPE. There are patchy infiltrates throughout the lung tissue, with predominant changes in the right middle lobe/right central hemithorax. Courtesy of Wikipedia (https://en.wikipedia.org/wiki/File:Chest_XR_of_HAPE.png).
High-altitude pulmonary edema (HAPE). Plain chest x-ray (radiograph) of a patient diagnosed with HAPE. There are patchy infiltrates throughout the lung tissue, with predominant changes in the right middle lobe/right central hemithorax. Courtesy of Wikipedia (https://en.wikipedia.org/wiki/File:Chest_XR_of_HAPE.png).
High-altitude illness may result from short-term exposures to altitudes in excess of 2000-2500 m (6562 -8202 ft). [1, 2, 3] This illness comprises a spectrum of clinical entities that are probably the manifestations of the same disease process. HAPE and cerebral edema (HACE) are the most ominous of these symptoms, whereas acute mountain sickness, retinal hemorrhages, and peripheral edema are the milder forms of the disease. The rate of ascent, the altitude attained, availability of acclimatization days, the amount of physical activity at high altitude, and individual susceptibility are contributing factors to the incidence and severity of high-altitude illness. [1, 3, 4] It's important to note that high-altitude illness should not be excluded if an individual is below 2500 m.
High-altitude pulmonary edema generally occurs 2-4 days after rapid ascent to altitudes in excess of 2500 m. [2, 3] Young people and previously acclimatized people reascending to a high altitude following a short stay at low altitude seem to be more predisposed to HAPE. Cold weather and physical exertion at high altitude are other predisposing factors.
Signs and symptoms of high-altitude pulmonary edema include:
-
Dyspnea with exertion and, eventually, dyspnea at rest, associated with weakness and cough
-
Decreased exercise tolerance and slow recovery from exercise
-
Extreme fatigue/weakness
-
Tachycardia and tachypnea at rest
-
Nonproductive cough, frothy sputum
-
Rales
-
Cyanosis
-
Symptoms worse at night
High-altitude pulmonary edema may be fatal within a few hours if left untreated. Patients who recover from HAPE have rapid clearing of edema fluid and do not develop long-term complications.
The treatment of high-altitude pulmonary edema includes rest, administration of oxygen, and descent to a lower altitude. If diagnosed early, recovery is rapid with a descent of only 500-1000 m. A portable hyperbaric chamber or supplemental oxygen administration immediately increases oxygen saturation and reduces pulmonary artery pressure, heart rate, respiratory rate, and symptoms. In situations where descent is difficult, these treatments can be lifesaving. [5, 6]
Also see Altitude Illness - Cerebral Syndromes and Altitude Illness - Pulmonary Syndromes.
For patient education resources, visit the First Aid & Emergencies Center. Also, see the patient education article Altitude Sickness.
Pathophysiology
Although all forms high-altitude illness are caused by hypobaric hypoxia leading to hypoxemia, [7] the pathophysiology high-altitude pulmonary edema (HAPE) is not well understood. [8] HAPE is a noncardiogenic form of pulmonary edema resulting from a leak in the alveolar capillary membrane; left-ventricular function is preserved. The various mechanisms believed to be responsible are pulmonary arterial vasoconstriction and elevated pulmonary artery pressure, resulting in circulatory shear forces and a consequent permeability leak and antidiuresis possibly mediated by increased antidiuretic hormones, which contribute to fluid retention. The inciting factor appears to be excessive hypoxia. [9]
A number of compensatory mechanisms improve oxygen delivery when its inspired concentration is reduced. The first adaptation to high altitude is an increase in minute ventilation. The ventilatory response to a relatively hypoxic stimulus can be divided into four phases: (1) initial increase on ascent, (2) subsequent course over hours and weeks, (3) deacclimatization on descent, and (4) long-term response of high-altitude natives.
The barometric pressure decreases with distance above the Earth's surface in an approximately exponential manner. The pressure at 5500 m (18,000 ft) is only half the normal 760 mm Hg, so that the partial pressure of oxygen (PO2) of moist inspired gas is (380-47) × 0.2093 = 70 (47 mm Hg is the partial pressure of water vapor at body temperature [ie, 37ºC]). At the summit of Mount Everest (altitude 8848 m or 29,028 ft), the inspired PO2 is only 43. In spite of hypoxia associated with high altitude, approximately 15 million people live at elevations over 3050 m, and some permanent residents live higher than 4900 m in the Andes. A remarkable degree of acclimatization occurs when humans ascend to these altitudes. Climbers have lived for several days at altitudes that would cause unconsciousness within a few seconds in the absence of acclimatization.
Spirometric studies have shown that with increasing altitude, both forced vital capacity (FVC) and forced expiratory volume in one second (FEV1) are reduced by up to 25% (74.8% / 74.6% of baseline). In the same study, peak expiratory flow (PEF) initially increased up to 4451 m and returned to baseline values above 5000 m. After descent below 2000 m, all values normalized within one day. These findings were consistent with increasing pulmonary restriction at high altitudes (without a marked reduction of PEF). Portable spirometry may provide clinically relevant information (impending pulmonary edema) in high-altitude travelers. [10, 11, 12]
Bronchoalveolar lavage fluid (BALF) studies have shown that after heavy exercise, under all conditions, athletes develop a permeability edema with high BALF RBC and protein concentrations in the absence of inflammation. Exercise at altitude (3810 m) caused significantly greater leakage of RBCs (92,000 [SD 3.1] cells/mL) into the alveolar space than that seen with normoxic exercise (54,000 [SD 1.2] cells/mL). At altitude, the 26-hour postexercise BALF had significantly higher RBC and protein concentrations, suggesting an ongoing capillary leak. These findings suggest that pulmonary capillary disruption occurs with intense exercise in healthy humans and that hypoxia augments the mechanical stresses on the pulmonary microcirculation. [13]
Autopsy studies performed on patients who died of HAPE have shown a proteinaceous exudate with hyaline membranes. The studies have shown areas of pneumonitis with neutrophil accumulation, although none was noted to contain bacteria. Pulmonary veins were not dilated. Most reports mention capillary and arteriolar thrombi with deposits of fibrin, hemorrhage, and infarcts. The findings suggest a protein-rich edema with a possibility that clotting abnormalities may be partially responsible for this illness.
Bronchoalveolar lavages performed on patients with HAPE have also shown the fluid to have a high protein content, higher than in patients with adult respiratory distress syndrome (ARDS). The fluid was also highly cellular. Unlike ARDS, which primarily has neutrophils in the lavage fluid, HAPE fluid contains a higher percentage of alveolar macrophages. Additionally, chemotactic (leukotriene B4) and vasoactive (thromboxane B2) mediators were present in the lavage.
Etiology
High-altitude pulmonary edema (HAPE) generally occurs 2-4 days after rapid ascent to altitudes in excess of 2500 m (8202 ft). Young people and previously acclimatized people reascending to a high altitude following a short stay at low altitude seem more predisposed to HAPE. Other predisposing factors include the following [1] :
-
Cold weather
-
Physical exertion at high altitude
-
Male sex
-
Use of sleep medications
-
Excessive salt ingestion
Preexisting conditions that may predispose toward the development of high-altitude pulmonary edema include the following [1] :
-
Conditions that lead to increased pulmonary blood flow
-
Pulmonary hypertension
-
Increased pulmonary vascular reactivity
-
Patent foramen ovale
Epidemiology
United States data
The incidence of high-altitude pulmonary edema (HAPE) ranges from an estimated 0.01% to 15.5%. In Colorado, the incidence of HAPE is 1 per 10,000 skiers and up to 1 per 100 climbers at more than 4,270 m (14,010 ft).
The risk of HAPE rises with increased altitude and faster ascent. At 4500 m, the incidence is 0.6% to 6%,; at 5500 m, the incidence is 2% to 15%. [1] Climbers with a previous history of HAPE, who ascent rapidly above 4,500 m (14,764 ft) have up to a 60% chance of illness recurrence. [1, 14]
International data
In a study on Mount Everest trekkers, the incidence of high-altitude pulmonary edema (HAPE) was about 1.6%. The incidence of mountain sickness appears to be unusually high in trekkers on Mount Rainier; however, the incidence of pulmonary edema is the same as in other places. One study reported that Everest region trekkers were more likely to be evacuated for altitude illness than trekkers in other regions. [15]
Sex-related demographics
Men and women are equally susceptible to acute mountain sickness, but women may be less likely to develop high-altitude pulmonary edema. In addition to individual differences in susceptibility, other factors, such as alcohol, respiratory depressants, and respiratory infections, may enhance vulnerability to altitude illness.
Age-related demographics
The typical patient with high-altitude pulmonary edema (HAPE) is a young person who is otherwise physically fit. HAPE is rare in infants and small children.
Prognosis
High-altitude pulmonary edema (HAPE) may be fatal within a few hours if left untreated. Patients who recover from HAPE have rapid clearing of edema fluid and do not develop long-term complications. Although outcome varies significantly depending on altitude, management, and access to medical care, the mortality rate has been reported to be as high as 11% with treatment [16] but up to 50% if untreated. [1] As many as 50% of patients with high-altitude pulmonary edema may have concurrent acute mountain sickness, and up to 14% have concurrent high-altitude cerebral edema. [1]
One study has shown that the estimated incidence of altitude illness–related death was 7.7 deaths in 100,000 trekkers. The mortality has been increasing over the last decade. [15]
Although reports document successful ascents of Mount Everest following episodes of high-altitude pulmonary edema, the safety of continuing ascent following treatment and resolution of high-altitude pulmonary edema remains controversial. If ascent is pursued, the individual should be symptom-free and off any medications for at least several days before initiating further ascent, and they should strongly consider pharmacologic prophylaxis for their ascent. [2, 17]
-
High-altitude pulmonary edema (HAPE). Plain chest x-ray (radiograph) of a patient diagnosed with HAPE. There are patchy infiltrates throughout the lung tissue, with predominant changes in the right middle lobe/right central hemithorax. Courtesy of Wikipedia (https://en.wikipedia.org/wiki/File:Chest_XR_of_HAPE.png).
-
High-altitude pulmonary edema (HAPE). Medical students demonstrate the use of a portable hyperbaric chamber. Courtesy of Wikipedia (https://en.wikipedia.org/wiki/File:Portable_hyperbaric_chamber.jpg).
-
High-altitude pulmonary edema (HAPE). Initial chest x-ray showing pulmonary infiltrates in the right lung especially in the right mid and lower lung zones indicative of pulmonary edema. The patient was a middle-aged woman trekker who was emergency air-lifted from an altitude of 4410 m in the Nepal Himalayas to 1300 m in Kathamandu. She had continued ascending despite experiencing mild altitude symptoms at Namche (3440 m), with considerably worsened symptoms at Tengboche (3860 m). Courtesy of Extreme Physiology & Medicine (PMID: 24636661, online at https://extremephysiolmed.biomedcentral.com/track/pdf/10.1186/2046-7648-3-6).
-
High-altitude pulmonary edema (HAPE). Repeat chest x-ray after 2 days showing rapid resolution of the pulmonary edema in the same Himalayan trekker discussed in the previous image. The patient received bed rest, supplemental oxygen, and oral sustained-release nifedipine 20 mg twice daily. Courtesy of Extreme Physiology & Medicine (PMID: 24636661, online at https://extremephysiolmed.biomedcentral.com/track/pdf/10.1186/2046-7648-3-6).
-
High-altitude pulmonary edema (HAPE). Pulmonary embolism masquerading as HAPE. Axial computed tomography (CT) pulmonary angiogram showing thrombi as filling defects in the right main pulmonary artery (right arrow) extending into its branch and in the distal left pulmonary artery (left arrow) with extension into its superior branch. Courtesy of High Altitude Medicine & Biology (PMID: 27768392, online at https://www.liebertpub.com/doi/full/10.1089/ham.2016.0008).
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Treatment
- Guidelines
- Guidelines Summary
- HAPE Prevention and Treatment Guidelines (WMS, CDC)
- FDA Policy for Face Masks, Face Shields, and Respirators in COVID-19 (2020)
- COVID-19–Related Airway Management Clinical Practice Guidelines (SIAARTI/EAMS, 2020)
- COVID-19 Ventilation Clinical Practice Guidelines (ESICM, 2020)
- Show All
- Medication
- Media Gallery
- References








