Background
Proteus species are part of the Enterobacteriaceae family of gram-negative bacilli. They are facultative anaerobes with an ability to ferment maltose and inability to ferment lactose. The first isolates were reported and characterized by Hauser in the late 19th century. The genus is currently composed of Proteus mirabilis, Proteus vulgaris, Proteus penneri, Proteus hauseri, Proteus terrae, and Proteus cibarius.P mirabilis and P vulgaris account for most clinical Proteus isolates. Proteus organisms are implicated as serious causes of infections in humans, along with Escherichia, Klebsiella, Enterobacter, and Serratia species.
Proteus species are most commonly found in the human intestinal tract as part of normal human intestinal flora, along with Escherichia coli and Klebsiella species, of which E coli is the predominant resident. Proteus is also found in multiple environmental habitats, including long-term care facilities and hospitals. In hospital settings, it is not unusual for gram-negative bacilli to colonize both the skin and oral mucosa of both patients and hospital personnel. Infection primarily occurs from these reservoirs. However, Proteus species are not the most common cause of nosocomial infections.
P mirabilis causes 90% of Proteus infections and can be considered a community-acquired infection. P vulgaris and P penneri may be isolated from individuals in long-term care facilities and hospitals and from patients with underlying diseases or compromised immune systems.
Patients with recurrent infections, those with structural abnormalities of the urinary tract, those who have had urethral instrumentation, and those whose infections were acquired in the hospital have an increased frequency of infection caused by Proteus and other organisms (eg, Klebsiella, Enterobacter, Pseudomonas,enterococci, staphylococci).
Pathophysiology
Proteus species possess an extracytoplasmic outer membrane, a feature shared with other gram-negative bacteria. In addition, the outer membrane contains a lipid bilayer, lipoproteins, polysaccharides, and lipopolysaccharides.
Infection depends on the interaction between the infecting organism and the host defense mechanisms. Various components of the membrane interplay with the host to determine virulence. Inoculum size is important and has a positive correlation with the risk for infection.
Certain virulence factors have been identified in bacteria. The first step in the infectious process is adherence of the microbe to host tissue. Fimbriae facilitate adherence and thus enhance the capacity of the organism to produce disease. E coli, P mirabilis, and other gram-negative bacteria contain fimbriae (ie, pili), which are tiny projections on the surface of the bacterium. Specific chemicals located on the tips of pili enable organisms to attach to selected host tissue sites (eg, urinary tract endothelium). The presence of these fimbriae has been demonstrated to be important for the attachment of P mirabilis to host tissue.
The attachment of Proteus species to uroepithelial cells initiates several events in the mucosal endothelial cells, including secretion of interleukin 6 and interleukin 8. Proteus organisms also induce apoptosis and epithelial cell desquamation. Bacterial production of urease has also been shown to increase the risk for pyelonephritis in experimental animals. Urease production, together with the presence of bacterial motility and fimbriae, may favor the production of upper urinary tract infections (UTIs) by organisms such as Proteus.
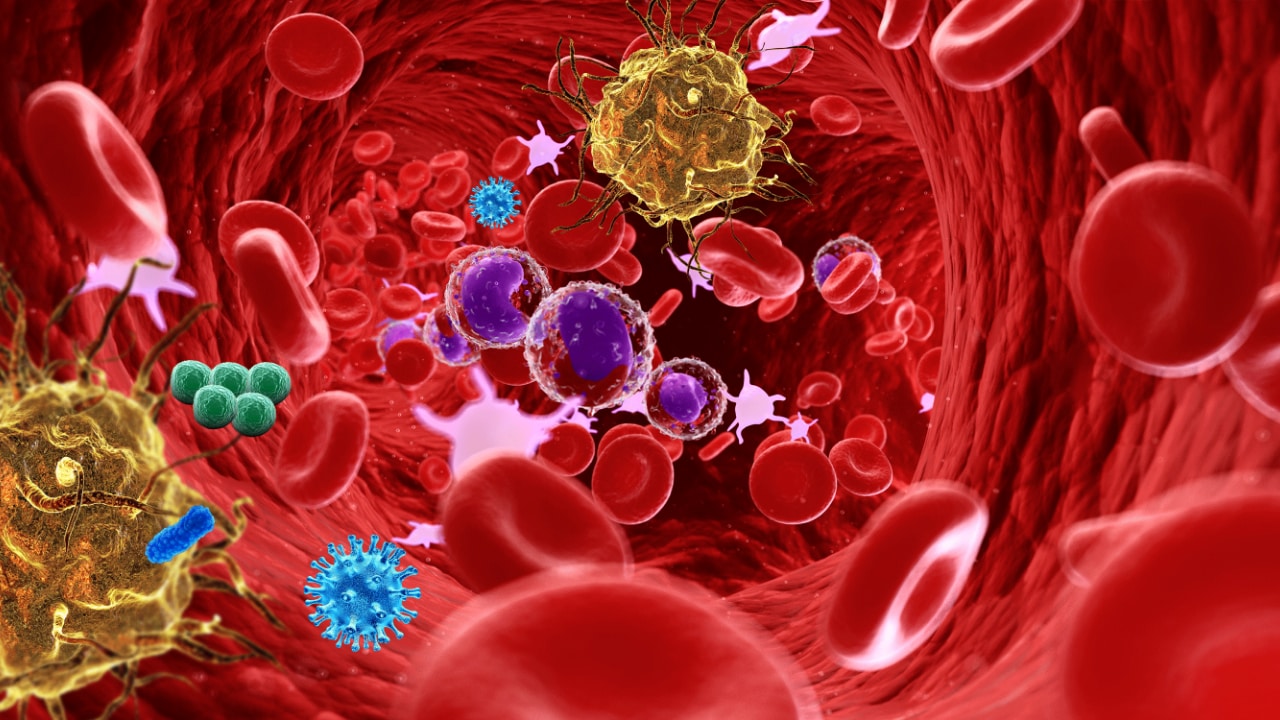
Enterobacteriaceae (of which Proteus is a member) and Pseudomonas species are the microorganisms most commonly responsible for gram-negative bacteremia. When these organisms invade the bloodstream, endotoxin, a component of gram-negative bacterial cell walls, apparently triggers a cascade of host inflammatory responses and leads to major detrimental effects. Because Proteus and Pseudomonas organisms are gram-negative bacilli, they can cause gram-negative endotoxin-induced sepsis, resulting in systemic inflammatory response syndrome (SIRS), which carries a mortality rate of 20-50%.
Although other organisms can trigger a similar response, it is useful to consider gram-negative bacteremia as a distinct entity because of its characteristic epidemiology, pathogenesis, pathophysiology, and treatment. The presence of the sepsis syndrome associated with a UTI should raise the possibility of urinary tract obstruction. This is especially true of patients who reside in long-term care facilities, who have long-term indwelling urethral catheters, or who have a known history of urethral anatomic abnormalities.
The ability of Proteus organisms to produce urease and to alkalinize the urine by hydrolyzing urea to ammonia makes it effective in producing an environment in which it can survive. This leads to precipitation of organic and inorganic compounds, which leads to struvite stone formation. Struvite stones are composed of a combination of magnesium ammonium phosphate (struvite) and calcium carbonate-apatite.
Struvite stone formation can be sustained only when ammonia production is increased and the urine pH is elevated to decrease the solubility of phosphate. Both of these requirements can occur only when urine is infected with a urease-producing organism such as Proteus. Urease metabolizes urea into ammonia and carbon dioxide: Urea → 2NH3 + CO2. The ammonia/ammonium buffer pair has a pK of 9.0, resulting in the combination of highly alkaline urine rich in ammonia.
Symptoms attributable to struvite stones are uncommon. More often, women present with UTI, flank pain, or hematuria and are found to have a persistently alkaline urine pH (>7.0).
The acquisition of a particular phenotype known as "swarm cell differentiation" facilitates the ascent of P mirabilis into the urinary tract. The swarming behavior of Proteus species results in a characteristic bullseye pattern on a plate culture. When Proteus species swarm, the production of secreted proteins, including virulence factors such as the protease ZapA, dramatically increases. This swarming motility is regulated through a complex network acting on the flagellar transcription regulator flhDC. The name Proteus follows from the character in Homer's Odyssey who is capable of changing form.
Epidemiology
Frequency
United States
The genitourinary tract is the site of disease responsible for gram-negative bacteremia in approximately 35% of patients. In previously healthy outpatients, E coli is by far the most often implicated cause of UTIs. In contrast, individuals with multiple prior episodes of UTI, multiple antibiotic treatments, urinary tract obstruction, or infection developing after instrumentation frequently become infected with Proteus bacteria or other bacteria such as Enterobacter, Klebsiella, Serratia, and Acinetobacter.
Bacteriuria occurs in 10-15% of hospitalized patients with indwelling catheters. The risk for infection is 3-5% per day of catheterization.
Mortality/Morbidity
Among long-term care residents, UTIs are the second most common infection responsible for hospital admission, second only to pneumonia. UTIs can result in sepsis if not recognized and treated rapidly. Failure to treat or a delay in treatment can result in SIRS, which carries a mortality rate of 20-50%.
Sex
Other factors that increase infection rates include female sex, duration of catheterization, underlying illness, faulty catheter care, and lack of systemic antibiotic therapy. Infection occurs either by migration of bacteria up the catheter along the mucosal sheath or by migration up the catheter lumen from infected urine.
UTIs are the most common clinical manifestation of Proteus infections. Proteus infection accounts for 1-2% of UTIs in healthy women and 5% of hospital-acquired UTIs. Complicated UTIs (ie, those associated with catheterization) have a prevalence of 20-45%.
UTIs are more common in males then females in the neonatal population. This is a result of congenital abnormalities seen more often in males.
After age 50 years, the ratio between men and women begins to decline because of the increasing incidence of prostate disease. UTIs in men younger than 50 years are usually caused by urologic abnormalities.
Age
UTIs are more common in persons aged 20-50 years.
-
After 24 hours, this inoculated MacConkey agar culture plate cultivated colonial growth of gram-negative, rod-shaped, and facultatively anaerobic Proteus vulgaris bacteria. Courtesy of the CDC.