Practice Essentials
Atrioventricular (AV) block is an interruption or delay of electrical conduction from the atria to the ventricles due to conduction system abnormalities in the AV node or the His-Purkinje system. Conduction delay or block can be physiologic if the atrial rate is abnormally fast or pathologic at normal atrial rates. AV block is generally defined based on a regular atrial rhythm.
Signs and symptoms
First-degree AV block
-
Generally asymptomatic
-
Excessive delay causes dyspnea, weakness, or dizziness
Second-degree AV block
-
Can be asymptomatic
-
Palpitations, weakness, lightheadedness, or syncope
-
Manifests on physical examination as bradycardia (especially Mobitz II) and/or irregularity of heart rate (during Mobitz I AV block)
Third-degree AV block
-
Fatigue, dizziness, and light-headedness are common and, with concomitant structural heart disease, heart failure, weakness, chest pain, confusion and syncope may occur
-
Associated with profound bradycardia unless the site of the block is located in the AV node
-
Can cause asystole leading to cardiac arrest and/or death
See Clinical Presentation for more specific information.
Diagnosis
Laboratory studies
-
Electrolyte levels (hyperkalemia) and drug levels (eg, digitalis), if elevated potassium level or drug toxicity is suspected
-
Troponin levels: If AV block is suspected due to ischemia/infarction
-
Infection (Lyme titers), myxedema (thyroid stimulating hormone [TSH] levels), or connective tissue disease (ANA) studies in cases of systemic illness
Electrocardiography
-
12-Lead ECG recordings and/or rhythm/monitor strips
-
24-Hour and/or prolonged monitoring
-
Implantable loop recorder
Additional modalities
-
Electrophysiologic test: To determine the location of the block and other arrhythmias
-
Echocardiography: To assess ventricular function (especially if an implantable device is required)
-
Exercise test: To assess if AV block worsens or improves with exercise
See Clinical Presentation and Workup for more specific information on the diagnosis of AV block.
Management
Pacemaker implantation
A pacemaker is indicated when there is irreversible and longstanding asymptomatic bradycardia due to AV block: [1, 2] :
See Treatment: Pacemaker Implantation for more specific information on this topic.
Pharmacologic therapy
Considerations regarding the administration of anticholinergic agents include the following:
-
Atropine and isoproterenol infusion can improve AV conduction in emergencies in which bradycardia is caused by AV block in the AV node
-
Dopamine and dobutamine can occasionally be helpful
See Medication for more specific information on the treatment of atrioventricular block.
Background
Atrioventricular (AV) block is an interruption or delay of electrical conduction from the atria to the ventricles due to conduction system abnormalities in the AV node or the His-Purkinje system. Conduction delay or block can be physiologic if the atrial rate is abnormally fast or pathologic at normal atrial rates. AV block is generally defined based on a regular atrial rhythm.
AV block is categorized as first-, second-, and third-degree AV block. First-degree AV block is defined as AV conduction slowing; on the electrocardiogram (ECG), the PR interval exceeds 0.20 seconds (sec). In second-degree AV block, some P waves conduct while others do not. This type is subdivided into Mobitz I (Wenckebach), Mobitz II, 2:1, paroxysmal, and high-grade AV block. During third-degree (“complete”) AV block, no AV conduction occurs when it should be able to occur.
Symptoms of AV block range from no symptoms to weakness, fatigue, shortness of breath, exercise intolerance, or syncope. Low cardiac output can cause hypotension and end-organ hypoperfusion. Death due to asystole is possible in complete heart block. Treatment involves correction or resolution of underlying causes and, if AV block is progressive, symptomatic, and/or persistent, a pacemaker is required. [3]
First-degree AV block
First-degree AV block consists of the following:
-
PR prolongation (PR interval >0.20 sec in adults and >0.160 sec in young children) with 1:1 AV conduction (see the image below)
-
A narrow QRS is associated with conduction slowing in the AV node, but it may be in the atria, and with a wide QRS, conduction slowing is in the His-Purkinje system
-
Marked PR interval prolongation (>0.30 sec) is usually associated with slowing in the AV node
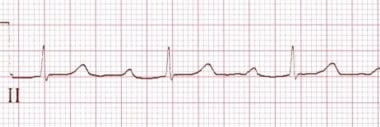 Atrioventricular Block. This rhythm strip shows first-degree atrioventricular block with a PR interval of 0.360 sec. Note the fixed prolonged PR interval.
Atrioventricular Block. This rhythm strip shows first-degree atrioventricular block with a PR interval of 0.360 sec. Note the fixed prolonged PR interval.
Second-degree AV block
Second-degree AV block is characterized by the following:
-
Some, but not all, atrial impulses (generally occurring at a regular rate) failing to conduct to the ventricles
-
Categorized as Mobitz I, II, 2:1, paroxysmal, or high-degree AV block
Mobitz I second-degree AV block
Mobitz I second-degree AV block is associated with constant PP intervals, progressive PR prolongation, followed by one nonconducted P wave. Often, there is progressive shortening of the RR intervals during the Wenckebach cycle and a pause due to a blocked P wave that is less than the sum of two PP intervals. This form of AV block occurs in less then 50% of all types of AV block and is generally due to a block in the AV node. [4] Rarely, it can occur with a block within or below the His Bundle; this is intra or infra-Hisian Wenckebach block, respectively. [5]
Mobitz I block rarely progresses to third-degree block. Distinguishing a block in the AV node versus infra-Hisian block can be challenging. Carotid sinus massage will worsen AV node conduction during Wenckebach block, but it may improve conduction if the block occurs below the His bundle. Exercise will worsen a block in the His-Purkinje system but improve it if the block occurs in the AV node. Mobitz I AV block usually consists of a ratio of nonconducted to conducted beats of 4:3, 3:2, and so on (see the image below).
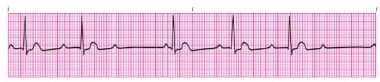 Atrioventricular Block. Second-degree Mobitz type I atrioventricular block. Note the prolongation of the PR interval preceding the dropped beat and the shortened PR interval following the dropped beat.
Atrioventricular Block. Second-degree Mobitz type I atrioventricular block. Note the prolongation of the PR interval preceding the dropped beat and the shortened PR interval following the dropped beat.
Mobitz II second-degree AV block
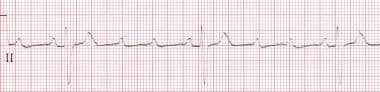
Mobitz II second-degree AV block is characterized by constant PP and RR intervals (see the image below). There is a constant PR interval before failure of an atrial impulse to conduct to the ventricle (small changes can occur in the PR interval after the blocked beat). The pause—including the blocked P waves—equals two PP cycles (unless an early junctional escape beat occurs). Mobitz II block occurs in the His-Purkinje system and may be associated with a narrow QRS but, as there often is in His-Purkinje disease, a wide complex QRS is commonly seen (bundle branch block) in the conducted beats. Mobitz II AV block may progress to complete AV block. Carotid sinus massage improves AV conduction in the His-Purkinje system, as it causes the sinus rate to slow; however, walking, exercise, or atropine use may lead to progressively worse AV block, as impulses may impinge upon an already damaged conduction system.
 Atrioventricular Block. Second-degree Mobitz II atrioventricular block. Note the fixed PR interval, but after the third beat, an atrial impulse fails to conduct to the ventricle. Courtesy of Wikimedia Commons (https://commons.wikimedia.org/wiki/File:Second_degree_heart_block.png).
Atrioventricular Block. Second-degree Mobitz II atrioventricular block. Note the fixed PR interval, but after the third beat, an atrial impulse fails to conduct to the ventricle. Courtesy of Wikimedia Commons (https://commons.wikimedia.org/wiki/File:Second_degree_heart_block.png).
2:1 second-degree AV block
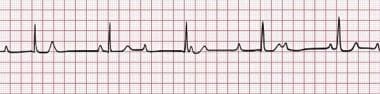
A 2:1 AV block is noted when every other P wave (with a regular PP interval) is conducted to the ventricle (see the image below). The block may be at the level of AV node or below. Close analysis of a long rhythm strip may help define the location of 2:1 AV block, especially during particular maneuvers. For example, if the block is in the His bundle or below, exercise, walking, or even standing may improve the AV node conduction; however, it will slow the ventricular rate and increase the level of the block. Carotid massage or atropine use may improve conduction if the block is in the His-Purkinje system, but it will worsen the block if it is at the level of the AV node.
Look for the presence of a bundle branch block. If present, a 2:1 AV block is more likely occurring in the His-Purkinje system.
 Atrioventricular Block. A constant PP interval and normal PR interval in conducted beats is present. This progresses to 2:1 atrioventricular (AV) block. A 2:1 AV block can be present with conduction delay in the AV node or His-Purkinje system, but it is more likely to be in the AV node for all patients (with a greater chance of AV block in the His-Purkinje system if there is a bundle branch block). Review extended monitoring strips because Mobitz I or Mobitz II may be present at other times, and this might help to determine the level of the block.
Atrioventricular Block. A constant PP interval and normal PR interval in conducted beats is present. This progresses to 2:1 atrioventricular (AV) block. A 2:1 AV block can be present with conduction delay in the AV node or His-Purkinje system, but it is more likely to be in the AV node for all patients (with a greater chance of AV block in the His-Purkinje system if there is a bundle branch block). Review extended monitoring strips because Mobitz I or Mobitz II may be present at other times, and this might help to determine the level of the block.
Paroxysmal AV block
Paroxysmal AV block is a form of second-degree AV block that is not persistent or repetitive, as there is an abrupt block in AV conduction. It may occur due to paroxysmal augmentation in vagal activation.
High-degree AV block
High-degree AV block consists of multiple constant P waves in a row that do not conduct. The conduction ratio can be 3:1 or higher; the PR interval of conducted beats can be constant (with His-Purkinje disease) or variable (with AV nodal block). This is distinct from complete AV block, because some P waves conduct to the ventricle. Atrial fibrillation with pauses greater than 5 seconds is due to a high-degree AV block. It can be associated with a narrow or wide QRS complex.
 Atrioventricular Block. High-degree atrioventricular block is demonstrated with a 4:1 atrial-to-ventricular conduction ratio. Note the P wave prior to the QRS conducts whereas the others do not. Courtesy of Life in the Fast Lane (https://lifeinthefastlane.com/ecg-library/basics/high-grade-block/), Edward J Burns, MD, Sydney, Australia.
Atrioventricular Block. High-degree atrioventricular block is demonstrated with a 4:1 atrial-to-ventricular conduction ratio. Note the P wave prior to the QRS conducts whereas the others do not. Courtesy of Life in the Fast Lane (https://lifeinthefastlane.com/ecg-library/basics/high-grade-block/), Edward J Burns, MD, Sydney, Australia.
Third-degree AV block
Third-degree AV block consists of the following features:
-
No atrial impulses conduct to the ventricle when they should conduct (ie, complete AV block)
-
The P waves, generally regular, reflect a sinus node rhythm independent from a junctional (narrow) or ventricular (wide) escape rhythm (see the image below), and they may be regular or irregular
-
The junctional escape rate is 40-60 bpm, and the ventricular escape rate is 20-40 bpm
-
Non-sinus atrial rhythms such as atrial fibrillation, atrial flutter, or atrial tachycardia can be associated with third-degree AV block
 Atrioventricular Block. This rhythm strip shows third-degree atrioventricular block (complete heart block). The atrial rate is faster than the ventricular rate, and no association exists between the atrial and ventricular activity. Courtesy of Life in the Fast Lane (https://lifeinthefastlane.com/ecg-library/basics/complete-heart-block/), Edward J Burns, MD, Sydney, Australia.
Atrioventricular Block. This rhythm strip shows third-degree atrioventricular block (complete heart block). The atrial rate is faster than the ventricular rate, and no association exists between the atrial and ventricular activity. Courtesy of Life in the Fast Lane (https://lifeinthefastlane.com/ecg-library/basics/complete-heart-block/), Edward J Burns, MD, Sydney, Australia.
AV block mimickers
Blocked premature atrial complexes can be a physiologic process. These are not considered a form of AV block but are due to ectopic beats that occur when the AV node is refractory.
Paroxysmal vagal activation can occur during sleep and may be associated with sleep apnea. Other causes include cough, vomiting, urination, eating, and defecation. When AV block is present, the PR interval slows around the time of the AV block. With high vagal tone, the PR intervals will lengthen, whereas in 2:1 AV block, for example, the PR intervals are constant.
Atrial tachycardia/atrial flutter with 2:1 AV conduction is not a form of AV block. It is due physiologic impingement on AV nodal refractoriness.
AV dissociation
During AV dissociation, the atria and ventricles beat independently of each other. AV dissociation occurs when a subsidiary pacemaker in the AV node or the ventricle overtakes the sinus node for impulse initiation due to slowing of the sinus node, or it may occur when a subsidiary site beats faster than the sinus node. Complete AV block can occur with AV dissociation, but AV dissociation alone does not indicate AV block.
See the Medscape Drugs & Diseases article Atrioventricular Dissociation for more detailed information on this topic.
Pathophysiology
Atrioventricular (AV) block is due to the following conditions:
-
Ischemia
-
Degenerative changes
-
Infection (myocarditis) and infiltrative processes such as Lyme disease and sarcoidosis
-
Drugs (beta blockers, calcium antagonists) that slow AV nodal or block His-Purkinje (eg, procainamide, flecainide) conduction or lengthen AV node refractoriness
-
Bezold-Jarisch reflex: An inferior myocardial infarction may cause a temporarily increased vagal tone leading to transient Mobitz I or complete AV block
Etiology
Delay or lack of conduction through the atrioventricular (AV) node and below has multiple causes. Degenerative changes (eg, fibrosis, calcification, or infiltration) are the most common cause of non-ischemic AV block. Idiopathic fibrosis or calcification of the AV conduction system, commonly seen in the elderly, can cause complete AV block.
First-degree AV block
Causes of first-degree AV block include the following:
-
Delayed conduction within the AV node or His-Purkinje system
-
Intrinsic disease of the AV node, high vagal tone, or dual AV nodal pathways (two separate PR intervals)
-
Medications that block the AV node (beta-blockers, calcium channel antagonists, digitalis, and select antiarrhythmic medications) may prolong the PR interval
First-degree AV block is also associated with a greater risk of atrial fibrillation and a poorer prognosis in the general population and in patients with heart failure.
Second-degree AV block
Causes of Mobitz I second-degree AV block include the following:
-
Increased vagal tone (functional block)
-
Degenerative disease of the AV conduction system (commonly seen in the elderly)
-
Occurs physiologically at high heart rates (especially with pacing) as a result of increased refractoriness of the AV node
-
AV node–blocking medications
-
Lyme disease, myocarditis, and radiofrequency ablation of the slow pathway
Causes of Mobitz II second-degree AV block include the following:
-
Degenerative disease of the His-Purkinje system
-
Damage of the conduction system from coronary artery disease, valve surgery, myocardial infarction, myocarditis, infiltrative cardiomyopathies (sarcoidosis, hemochromatosis), myxedema, Lyme disease, neuromuscular disease, and AV junction ablation [6]
-
Systemic diseases (eg, ankylosing spondylitis, Reiter syndrome)
Third-degree AV block
Causes of third-degree AV block include the following:
-
Reversible causes: AV node–blocking drugs and ischemia
-
Pathologic causes: Include cardiomyopathy (infiltrative, idiopathic, and infarction), myocarditis (Lyme disease), endocarditis with abscess formation, and hyperkalemia
-
Anterior myocardial infarction causing ischemia or infarction of the bundle branches
-
Cardiac surgery, catheter ablation of the AV node, alcohol septal ablation, or neuromuscular disease
Epidemiology
Epidemiology of specific AV blocks in the United States
All types of AV blocks occur more frequently in people older than 70 years, especially in those who have structural heart disease.
First-degree AV block
-
Can be found in healthy adults but is associated with an increased risk of atrial fibrillation and adverse outcomes in some studies
-
Incidence increases with age
-
At age 20 years: PR interval may exceed 0.20 sec in 0.5-2% of healthy people
-
At age 60 years: Over 5% of healthy individuals have PR intervals exceeding 0.20 seconds
Mobitz type II second-degree AV block
-
Rare in healthy individuals
-
Wenckebach observed in 1-2% of healthy young people, especially during sleep
Congenital third-degree AV block
-
About 1 case per 15,000-20,000 births, primarily the result of AV node injury from maternal antibodies in women with lupus or Sjogren syndrome [7]
-
Most commonly diagnosed between 18-24 weeks’ gestation; may cause first-, second-, or third-degree AV block
International data
The international incidence is similar to that of the United States.
Age-, sex-, and race-related demographics
A 60% female preponderance exists in congenital third-degree AV block; for acquired third-degree AV block, a 60% male preponderance exists. No racial proclivity exists in AV blocks.
Prognosis
The prognosis in atrioventricular (AV) block is directly related to its degree and the patient's underlying medical problems. Those with advanced AV block who are not treated with permanent pacing remain at risk for syncope and sudden cardiac death, especially individuals with underlying structural heart disease.
In a prospective study of patients with first-degree AV block and the outcomes associated with it using data from 7,575 individuals from the Framingham Heart Study (mean age, 47 years; 54% women) who underwent a 12-lead electrocardiography, Cheng et al found 124 individuals had PR intervals above 0.2 sec on the baseline examination. [9] On follow-up, first-degree AV block was associated with an increased incidence of atrial fibrillation, pacemaker implantation, and all-cause mortality. [9] Other studies have also demonstrated similar findings. [10, 11, 12]
Symptomatic Mobitz type I AV block is associated with increased mortality if left untreated. A retrospective study that evaluated 299 patients (average age 75 years) with Mobitz I AV block found that device implantation was associated with a 46% reduction in mortality (hazard ratio [HR] 0.54; 95% confidence interval [CI] 0.35 to 0.82; P = 0.004). [9] Other studies have confirmed these findings. [13, 14]
Higher degrees of AV block are associated with poor outcomes. Kosmidou et al examined 3,115 patients undergoing percutaneous coronary intervention for ST-segment elevation myocardial infarction and found high-degree AV block (Mobitz type II or third-degree AV block) in 1.5% of the cohort. [15] Patients with high-degree AV block had increased mortality at 30-day, 1-year, and 3-year follow-ups (unadjusted HR 3.83, 95% CI 1.40 to 10.48; unadjusted HR 4.37, 95% CI 2.09 to 9.38; and unadjusted HR 2.78, 95% CI 1.31 to 5.91, respectively). [15]
Fetuses with second- or third-degree AV block, associated with congenital heart disease, have increased mortality, and surviving infants may require pacemaker therapy. [16]
Complications
Complications include the following:
-
Death due to asystole or Torsade de pointes
-
Cardiovascular collapse with syncope, aggravation of ischemic heart disease, congestive heart failure, and exacerbation of renal disease
Patient Education
Patients need to be aware of the reversible causes of atrioventricular (AV) block. Avoiding AV node–blocking antihypertensive agents could eliminate symptoms.
Inform patients with known first-degree AV block who are asymptomatic that block may increase over time, and they should quickly seek medical attention if syncope, lightheadedness, chest pain, or shortness of breath occurs.
-
Atrioventricular Block. This rhythm strip shows first-degree atrioventricular block with a PR interval of 0.360 sec. Note the fixed prolonged PR interval.
-
Atrioventricular Block. First-degree atrioventricular block. PR interval is constant and is 0.280 sec.
-
Atrioventricular Block. Second-degree Mobitz type I atrioventricular block. Note the prolongation of the PR interval preceding the dropped beat and the shortened PR interval following the dropped beat.
-
Atrioventricular Block. Second-degree atrioventricular block, Mobitz type I (Wenckebach). Note the prolongation of the PR interval preceding the dropped beat and the shortened PR interval following the dropped beat.
-
Atrioventricular Block. Second-degree Mobitz II atrioventricular block. Note the fixed PR interval, but after the third beat, an atrial impulse fails to conduct to the ventricle. Courtesy of Wikimedia Commons (https://commons.wikimedia.org/wiki/File:Second_degree_heart_block.png).
-
Atrioventricular Block. Second-degree atrioventricular block, Mobitz type II. A constant PR interval in conducted beats is present. Intraventricular conduction delay is also present.
-
Atrioventricular Block. A constant PP interval and normal PR interval in conducted beats is present. This progresses to 2:1 atrioventricular (AV) block. A 2:1 AV block can be present with conduction delay in the AV node or His-Purkinje system, but it is more likely to be in the AV node for all patients (with a greater chance of AV block in the His-Purkinje system if there is a bundle branch block). Review extended monitoring strips because Mobitz I or Mobitz II may be present at other times, and this might help to determine the level of the block.
-
Atrioventricular Block. High-degree atrioventricular block is demonstrated with a 4:1 atrial-to-ventricular conduction ratio. Note the P wave prior to the QRS conducts whereas the others do not. Courtesy of Life in the Fast Lane (https://lifeinthefastlane.com/ecg-library/basics/high-grade-block/), Edward J Burns, MD, Sydney, Australia.
-
Atrioventricular Block. This rhythm strip shows third-degree atrioventricular block (complete heart block). The atrial rate is faster than the ventricular rate, and no association exists between the atrial and ventricular activity. Courtesy of Life in the Fast Lane (https://lifeinthefastlane.com/ecg-library/basics/complete-heart-block/), Edward J Burns, MD, Sydney, Australia.
-
Atrioventricular Block. Third-degree atrioventricular block (complete heart block). The atrial rate is faster than the ventricular rate, and no association exists between the atrial and ventricular activity.







