Background
Toxic megacolon is a life-threatening condition characterized by nonobstructive segmental or pancolonic dilatation of at least 6 cm with systemic toxicity. [1] It was recognized by Marshak and Lester in 1950. [2] Although inflammatory bowel disease (IBD) is a common reason for toxic megacolon, other etiologies including infections, inflammation, bowel ischemia, radiation, and certain medications can lead to the development of this condition. [3, 4, 5] See the following images.
 Toxic Megacolon. A 22-year-old man presented with abdominal pain, passage of blood and mucus per rectum, abdominal distention, fever, and disorientation. Findings from sigmoidoscopy confirmed ulcerative colitis. Abdominal radiographs obtained 2 days apart show mucosal edema and worsening of the distention in the transverse colon. The patient's clinical condition deteriorated over the next 36 hours despite steroid and antibiotic therapy, and the patient had to undergo a total colectomy and ileostomy.
Toxic Megacolon. A 22-year-old man presented with abdominal pain, passage of blood and mucus per rectum, abdominal distention, fever, and disorientation. Findings from sigmoidoscopy confirmed ulcerative colitis. Abdominal radiographs obtained 2 days apart show mucosal edema and worsening of the distention in the transverse colon. The patient's clinical condition deteriorated over the next 36 hours despite steroid and antibiotic therapy, and the patient had to undergo a total colectomy and ileostomy.
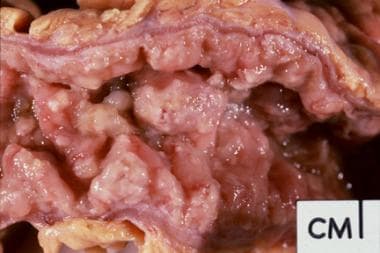 Toxic Megacolon. Gross pathology specimen from a case of pseudomembranous colitis demonstrating characteristic yellowish plaques.
Toxic Megacolon. Gross pathology specimen from a case of pseudomembranous colitis demonstrating characteristic yellowish plaques.
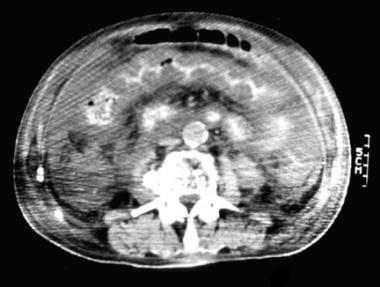 Toxic Megacolon. Computed tomography scan from a patient with pseudomembranous colitis demonstrating the classic accordion sign.
Toxic Megacolon. Computed tomography scan from a patient with pseudomembranous colitis demonstrating the classic accordion sign.
It is important to differentiate toxic megacolon from other conditions that present with megacolon without systemic toxicity such as Hirschsprung disease, [6] idiopathic megacolon/chronic constipation, chronic long-standing constipation of any etiology, and intestinal pseudo-obstruction (Ogilvie syndrome). [1] Patients with these conditions do not develop signs of systemic toxicity and, therefore, do not fall into the category of having toxic megacolon (see the image below). (See also Etiology, Presentation, and Workup.)
 Toxic Megacolon. A 72-year-old woman presented with vomiting and abdominal distention. The supine (right) and erect (left) plain abdominal radiographs show gross dilatation of the colon with multiple air-fluid levels. On further questioning, the patient revealed that she was taking diuretics for hypertension. Blood biochemical tests revealed markedly lowered potassium levels. After potassium replacement therapy, the patient's pseudo-obstruction completely resolved.
Toxic Megacolon. A 72-year-old woman presented with vomiting and abdominal distention. The supine (right) and erect (left) plain abdominal radiographs show gross dilatation of the colon with multiple air-fluid levels. On further questioning, the patient revealed that she was taking diuretics for hypertension. Blood biochemical tests revealed markedly lowered potassium levels. After potassium replacement therapy, the patient's pseudo-obstruction completely resolved.
Pathophysiology
Although the precise pathophysiology of toxic megacolon is unproven, several factors may contribute to its development and precipitation. In cases of uncomplicated colitis, the inflammatory response is confined to the mucosa. The microscopic hallmark of toxic megacolon is inflammation extending beyond the mucosa into the muscularis propria. Whereas the typical ulcerative colitis inflammatory response is limited to the mucosa, toxic megacolon is characterized by severe inflammation extending into the smooth muscle layer, thus paralyzing the colonic smooth muscle and leading to dilatation. The extent of dilatation seems to be correlated with the depth of inflammation and ulceration. [1]
Studies by Mourelle et al showed significantly increased amounts of inducible nitric oxide (NO) synthetase in the muscularis propria of patients with toxic megacolon, particularly in the more dilated colonic segments. [7, 8, 9]
As inflammation progresses into the smooth-muscle layers of the colon, NO and local inflammatory modulators appear to be involved in toxic megacolon pathogenesis. Neutrophils invade the muscle layer in toxic megacolon and directly damage the myocytes by the release of proteolytic enzymes, cytokines, and leukotriene B4. Systemic uptake of cytokines and other inflammatory mediators leads to fever, tachycardia, hypotension, and other signs of systemic toxicity. NO is generated by macrophages and smooth muscles cells in the inflamed portions of the colon, inhibiting smooth muscle tone and leading to colonic dilatation. [1]
These findings were supported by the idea that, in animal models, giving dexamethasone and/or decontaminating the bowel with broad-spectrum antibiotics led to decreased NO levels and improvement in colonic dilatation. [8] According to a study by Schworer et al, patients with toxic megacolon were successfully treated with NO synthase inhibitor. [10]
A number of other precipitating factors have been identified, including antimotility agents, opiates, anticholinergics, antidepressants, barium enemas, colonoscopies/bowel preparations, and immunotherapies. [5, 11, 12]
Myenteric plexus involvement is not consistent and likely does not contribute to colonic dilatation.
Etiology
Inflammatory causes of toxic megacolon include the following:
-
Crohn colitis [14]
Infectious causes of toxic megacolon include the following:
-
Salmonella species [15]
-
Shigella species [16]
-
Campylobacter species [17]
-
Yersinia species
-
Entamoeba histolytica: About 3% of patients with amoebic infections develop severe colitis and a small percentage of these will have toxic megacolon; use of loperamide in this setting increases the risk of developing toxic megacolon [21]
-
Cryptosporidium [22]
-
Cytomegalovirus [23]
-
Rotavirus [24]
-
Invasive aspergillosis [25]
Other etiologies of toxic megacolon include the following:
Often, triggering or predisposing factors can be identified. Signs and symptoms of acute colitis may be present for as long as 1 week before dilatation develops. Although the risk of toxic megacolon increases with the severity of the colitis, rapid tapering or abrupt discontinuation of medications such as steroids, sulfasalazine, and 5-aminosalicylic acid may precipitate toxemia and dilatation.
Medications that negatively impact bowel motility are also implicated in the development of toxic megacolon. These include, but are not limited to, anticholinergics, antidepressants, loperamide, atropine, [5] and opioids. Procedures such as barium enema or colonoscopy may cause distention, impair blood supply, or exacerbate a microperforation and cause subsequent toxemia. [12]
A retrospective study by Tschudin-Sutter et al indicated that the incidence of toxic megacolon is higher in pediatric patients with community–associated, rather than healthcare facility–associated, C difficile infection. [33] The study involved 202 pediatric patients with C difficile infection, including 38 with community–associated infection, 144 with healthcare facility–associated infection, and 20 with an indeterminate source of infection. Compared with the healthcare facility–associated group, children with a community–associated infection had a higher rate not only of toxic megacolon but also of toxic shock and recurrence. (They were less likely, however, to have comorbidities than were children with healthcare facility–associated infection.) [33]
Epidemiology
There is a lack in literature regarding accurate reporting of toxic megacolon prevalence. The incidence rates can change based on the main etiology. The risk of developing toxic megacolon can increase with older age and/or the presence of other risk factors such as hypertension, neurologic disorders, coagulopathy, anemia, chronic pulmonary disease, congestive heart failure, and renal failure. [34, 35]
Doshi et al reported the results of an analysis of data collected from the Nationwide Inpatient Sample database from January 2010 through December 2014: The most common cause of hospital admissions was inflammatory bowel disease (IBD) (51.6%), followed by septicemia (10.2%) and intestinal infections (4.1%). [34, 36]
Three decades ago, the incidence of toxic megacolon in IBD patients was approximately 1-5%. [14] However, this rate has diminished due to early recognition and intensive medical management of severe colitis. Unfortunately, the data on the incidence of toxic megacolon in ulcerative colitis versus Crohn disease are contradicting; some studies show a higher incidence in patients with Crohn disease compared to those with ulcerative colitis (1-2.5% ulcerative colitis; 4.4-6.3% Crohn disease), [14] whereas others report the opposite. [4, 37]
The incidence of toxic megacolon in patients with C difficile colitis rapidly increased from 0.4% to 3% before 1990 to 4.3% after 1990, due to the rising use of broad spectrum antibiotics and the development of a hypervirulent Crohn disease strain. [4, 35, 37]
Prognosis
Toxic megacolon mortality is variable depending on the treatment modality. One study revealed that before 1976, there was a 27% mortality of toxic megacolon among patients treated medically and a 19% mortality in patients treated surgically. [38] In-hospital mortality for patients with toxic megacolon fell from 9.2% to 6.5%, according to an observational study for the period between 2010 and 2014. [35] Older age, hypertension, neurologic disorders, coagulopathy, anemia, chronic lung disease, heart failure, and renal failure were the main predictors of increased mortality. [35]
Colon perforation is associated with higher surgical mortality relative to undergoing surgery before colonic perforation. [34, 38] Similarly, postoperative mortality in patients with C difficile infection and toxicity is lower when they undergo surgery before the development of septic shock compared to septic patients who have surgery. [39]
Fecal microbiota transplantation has shown promise as a salvage therapy for critically ill patients with C difficile infection and toxic megacolon in whom maximum medical therapy failed and who are not a surgical candidates. [40]
Mortality in patients with inflammatory bowel disease (IBD) and toxic megacolon have fallen in the last 3 decades due to multiple factors, including early recognition of toxic megacolon, early escalation from steroid treatment to biologics such as infliximab or cyclosporine, improved care in the intensive care unit (ICU), earlier surgical intervention, and optimal postoperative care. [41]
Note that C difficile infection in patients with IBD are associated with higher rates of colectomy and longer hospital stays compared to IBD patients without C difficile infection. [42]
Patient Education
Educating patients about toxic megacolon, is crucial. First, educate the patient about the causes of the disease, of which the most common is inflammatory bowel disease (IBD). However, with the rising incidence of C difficile infections, pseudomembranous colitis must always be considered, even in patients with IBD. Educate patients about ulcerative colitis, Crohn disease, and indeterminate colitis.
Also discuss with patients that medications such as corticosteroids, immunosuppressants, and/or immunomodulators may be administered to control the disease severity and that antibiotics may be used to prevent or treat infection. Inform patients of the potential risks and benefits of these agents as well as those that can exacerbate their condition (eg, opioids, antidepressants, nonsteroidal anti-inflammatories, antidiarrheals, anticholinergics.)
Secondly, clearly inform patients that if an operation is required for this acute problem, an ostomy likely will be the necessary procedure, regardless of the cause. Patients require at least a temporary and, possibly, a permanent ostomy. Provide a thoughtful, compassionate discussion regarding this aspect of their treatment: The psychological aspects of dealing with an ostomy can be extremely difficult.
Finally, educate patients so that they understand that this disease may require several months to overcome if an operation is needed and that a two- or three-stage procedure is usually required.
-
Toxic Megacolon. A 22-year-old man presented with abdominal pain, passage of blood and mucus per rectum, abdominal distention, fever, and disorientation. Findings from sigmoidoscopy confirmed ulcerative colitis. Abdominal radiographs obtained 2 days apart show mucosal edema and worsening of the distention in the transverse colon. The patient's clinical condition deteriorated over the next 36 hours despite steroid and antibiotic therapy, and the patient had to undergo a total colectomy and ileostomy.
-
Toxic Megacolon. A 72-year-old woman presented with vomiting and abdominal distention. The supine (right) and erect (left) plain abdominal radiographs show gross dilatation of the colon with multiple air-fluid levels. On further questioning, the patient revealed that she was taking diuretics for hypertension. Blood biochemical tests revealed markedly lowered potassium levels. After potassium replacement therapy, the patient's pseudo-obstruction completely resolved.
-
Toxic Megacolon. Gross pathology specimen from a case of pseudomembranous colitis demonstrating characteristic yellowish plaques.
-
Toxic Megacolon. Computed tomography scan from a patient with pseudomembranous colitis demonstrating the classic accordion sign.
-
Toxic Megacolon. Plain abdominal radiograph from a patient with known ulcerative colitis who presented with an acute exacerbation of his symptoms. This image shows thumbprinting in the region of the splenic flexure of the colon.
-
Toxic Megacolon. Increased postrectal space is a known feature of ulcerative colitis.
-
Toxic Megacolon. A 45-year-old woman presented with acute pain and colitis of uncertain etiology. The radiograph shows an increase in gaseous distention of the distal transverse colon, now measuring up to 80 mm in diameter (it was 60 mm 2 days previous). The transverse colon and sigmoid colon are both featureless, consistent with severe colitis. There is fecal loading in the right side of colon. No evidence of free gas or pneumatosis intestinalis is noted. The appearance is concerning for toxic megacolon. Courtesy of Craig Hacking, MBBS, Associate Professor, Royal Brisbane and Women’s Hospital (Radiopaedia.org, rID: 79194).