Practice Essentials
Although hirsutism is broadly defined as excessive hairiness, the common clinical use of the term refers to women with excess growth of terminal hair in a male pattern. In this sense, hirsutism is one of the most common endocrine disorders, affecting approximately 10% of women in the United States. In these women, the hairiness implies the presence of abnormal androgen action, which may represent a serious or, more likely, a nonserious medical problem. Regardless of the etiology, hirsutism can produce mental trauma and emotional anguish. [1] Even mild cases of hirsutism may be viewed by the patient and others as a presumptive loss of femininity. In more severe cases, hirsutism can be a serious cosmetic problem. The major objectives in the management of hirsutism are to rule out a serious underlying medical condition and to devise a plan of treatment. [2, 3]
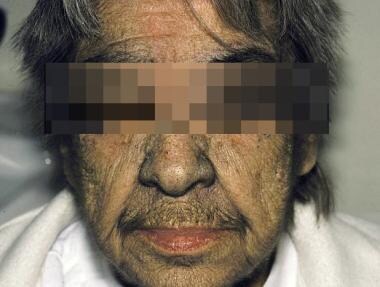
Idiopathic hirsutism in an elderly woman is shown in the photo below.
Signs and symptoms of hirsutism
Terminal hair, which depends on androgen, must be differentiated from vellus hair, which is androgen-independent. Vellus hair is fine, soft, and lightly pigmented. By contrast, terminal hair is coarse, curly, and pigmented.
In women with moderate to severe hirsutism, seek additional signs of hyperandrogenism, including (1) temporal hair recession, (2) oily skin, (3) masculine voice, (4) well-developed musculature, (5) enlargement of the clitoris (>35 mm2 in surface area), (6) irregular menses, and (7) psychological changes (eg, heightened libido, aggressiveness).
A thorough abdominal and pelvic examination is important in patients with hirsutism because more than half of androgen-secreting adrenal and ovarian tumors are palpable.
Workup in hirsutism
Approximately 50% of women with even minimal hirsutism have excessive androgen. Laboratory studies in hirsutism serve both to confirm the clinical impression of hyperandrogenism and to identify the source of excess androgens, either adrenal or ovarian.
The most important assay is the level of serum testosterone, the major circulating androgen. If the total serum testosterone level is normal, measure the free serum level because hyperandrogenism (and insulin resistance, if present) decreases sex steroid-binding globulin, such that the unbound, biologically active testosterone moiety may be elevated even if the total level is unremarkable.
If indicated based on the findings from the clinical evaluation and laboratory testing, perform ovarian ultrasonography and adrenal computed tomography (CT) scanning or magnetic resonance imaging (MRI) to evaluate for either ovarian or adrenal sources of androgen production.
Management of hirsutism
The treatment of hirsutism begins with a careful explanation about the cause of the problem and reassurance that the patient is not losing her femininity. Then, direct intervention, if possible, is instituted for the underlying disorder. If hirsutism persists (or the patient has idiopathic hirsutism), other cosmetic or systemic treatment may be necessary. In some cases, cosmetic measures may be sufficient. In others, the slow progress of systemic therapy may necessitate more immediate cosmetic treatment. The most effective strategy is to combine systemic therapy, which has a slow onset of effectiveness, with mechanical depilation (shaving, plucking, waxing, depilatory creams) or light-based (laser or pulsed-light) hair removal.
Systemic therapies directed at hirsutism can be divided into those that decrease ovarian or adrenal androgen production and those that inhibit androgen action in the skin. The systemic therapies include glucocorticoids, oral contraceptives (OCs), spironolactone, flutamide, finasteride, cyproterone acetate (not available in the United States), and insulin sensitizers (metformin and rosiglitazone).
Laser therapy has been shown not only to reduce unwanted hair but also to improve depression and anxiety in women with hirsutism. In many patients, hirsutism can be controlled just with laser, without using any drugs.
Pathophysiology
Hormones and the intrinsic characteristics of the hair follicle determine the quality of hair growth. Vellus hairs are fine, lightly pigmented hairs that cover most of the body before puberty. Pubertal androgens promote the conversion of these vellus hairs to coarser, pigmented terminal hairs. The level and duration of exposure to androgens, the local 5-alpha-reductase activity, and the intrinsic sensitivity of the hair follicle to androgen action determine the extent of conversion from vellus to terminal hair. However, some terminal hair growth is androgen-independent (eg, scalp, eyebrows, lashes). [4]
The development of terminal hair or reversion back to a vellus pattern may not be immediately evident because of the characteristics of the hair cycle. This cycle has 2 phases that include active hair growth (anagen phase) and a resting period (telogen phase), which follows the anagen phase. During the resting period, the hair shaft separates from the dermal papillae at the follicle base, and no further growth takes place. Eventually, growth restarts and the new hair shaft formed by the reactivated papillae pushes the old hair out. The cycle may take months to years to complete, and this causes a delay in hair growth response to changes in the androgen milieu.
Dihydrotestosterone is the androgen that acts on the hair follicle to produce terminal hair. This hormone is derived from both the bloodstream and local conversion of a precursor, testosterone. The local production of dihydrotestosterone is determined by 5-alpha-reductase activity in the skin. Differences in the activity of this enzyme may explain why women with the same plasma levels of testosterone can have different degrees of hirsutism.
A study by Willis et al found that self-reported hirsutism in women, as measured using the modified Ferriman-Gallwey score, was associated with menstrual irregularity, bleed lengths of 7 days or more, and heavy menstrual bleeding. [5]
Epidemiology
Frequency
United States
Hirsutism affects approximately 10% of women in the United States.
International
The prevalence rates of hirsutism in northern Europe are similar to those in the United States; in other places, rates are not known with certainty.
Mortality/Morbidity
The mortality and morbidity of hirsutism are determined by the underlying cause. Most women with idiopathic hirsutism have no associated mortality or morbidity. On the other extreme, a small number of women may have malignant disease with a grave prognosis.
A study by Comim et al suggested that premenopausal hirsutism and/or oligomenorrhea are risk factors for postmenopausal fractures, especially in the humerus and lower leg. The study included 1057 postmenopausal women aged over 55 years. [6] However, another study, by Rubin et al, suggested that PCOS reduces fracture risk, although the report dealt with a younger group of patients than did the Comim study and indicated that the risk reduction was greater in women who were under age 30 years when diagnosed. [7]
A prospective study by Robinson et al indicated that an association exists between maternal hirsutism and behavioral problems in offspring. The investigators reported that children born to mothers with hirsutism had a greater risk of borderline emotional symptoms (adjusted risk ratio [aRR] = 2.61), conduct disorder (aRR = 2.54), attention deficit hyperactivity disorder (aRR = 2.33), conduct problems (aRR = 2.22), and peer relationship difficulties (aRR = 1.92). [8]
Race
Ethnic origin significantly affects terminal hair growth in healthy women. Northern, fair-skinned Europeans have the least amount of terminal hair, whereas southern European, dark-skinned Mediterranean women have the greatest amount of terminal hair.
The difference in the racial patterns of normal terminal hair growth may be related to genetic differences of 5-alpha-reductase activity in the skin.
A study by Engmann et al reported that among patients with polycystic ovary syndrome (PCOS), aged 18-40 years, the prevalence of hirsutism was significantly greater in Hispanic women than in non-Hispanic white patients (93.8% vs 86.8%, respectively). [9]
A retrospective study by Afifi et al also found hirsutism in women with PCOS to be linked to ethnicity, as well as to Fitzpatrick skin type. Hirsutism in PCOS was most prevalent, and the modified Ferriman-Gallwey (mFG) hirsutism score was highest, in women of Hispanic, Middle Eastern, African American, and South Asian ethnicity. Moreover, a greater prevalence of hirsutism, along with an increased tendency toward truncal hirsutism, was noted with higher Fitzpatrick skin types. The investigators also determined that mFG scores in the truncal region and extremities tended to be higher in women of Middle Eastern and Hispanic ethnicity, while the score for the face was greater in African American and Hispanic patients. The least amount of hirsutism was found in women of Caucasian, Ashkenazi Jewish, East/Southeast Asian, and Native American ethnicity. [10]
A study by Chin et al found the prevalence of hirsutism to be 10% within a community sample of over 1500 African American women. An association with PCOS, severe acne, and irregular menstrual cycles suggested that the hirsutism resulted from hyperandrogenism. [11]
With the exception of congenital adrenal hyperplasia (CAH), the actual prevalence of diseases that cause hyperandrogenism and hirsutism has not been shown to differ among persons of different races.
Sex
As a medical problem, hirsutism predominates in women.
-
Although hirsutism can occur in men, it is more difficult to recognize because of the wide variability of healthy male terminal hair growth.
-
Hirsutism in prepubertal children occurs equally between sexes, is usually a sign of precocious puberty, and may signify a serious underlying disease.
This discussion focuses on adult women.
Age
The age of onset of hirsutism depends on the etiology. Most forms of nonneoplastic hirsutism become evident around puberty. This includes polycystic ovary syndrome (PCOS), CAH, and idiopathic hirsutism.
Hirsutism and acne are shown in the image below.
 The photograph depicts hirsutism in a young woman with polycystic ovary syndrome. Note the acne lesions and excessive hair on her face and neck.
The photograph depicts hirsutism in a young woman with polycystic ovary syndrome. Note the acne lesions and excessive hair on her face and neck.
Hirsutism may also develop after weight gain and cessation of the use of oral contraceptives (OCs) in young women. Normally, terminal hair growth becomes apparent after adrenarche and accelerates after puberty. Terminal hair continues to develop gradually in healthy women until after menopause, when loss of ovarian androgen leads to a loss of hair. Rapidly worsening hirsutism, especially in older women, should raise the suspicion of an androgen-secreting tumor.
Prognosis
Prognosis depends on the etiology of the hirsutism and whether it is benign or malignant.
Patient Education
Hirsutism requires a careful and systematic clinical evaluation coupled with a rational approach to treatment. Throughout this process, the patient must understand that, although diagnostic testing can be time consuming (and even inconclusive), it is sometimes essential for the determination of an effective intervention. In other cases, counseling and education may be all that is needed.
For the patient who desires treatment, a wide variety of pharmacologic strategies are available. Informing the patient that current systemic therapy is imperfect is important. Furthermore, none of the drugs used to treat hirsutism has FDA approval for such use. Initiate therapy only in patients who give informed consent after a complete explanation of the potential benefits and risks of a particular treatment and alternative approaches.
-
Idiopathic hirsutism in an elderly woman.
-
The photograph depicts hirsutism in a young woman with polycystic ovary syndrome. Note the acne lesions and excessive hair on her face and neck.
-
The photograph depicts familial hirsutism in a Pakistani woman.
-
Etiologic diagnosis of hirsutism.