Practice Essentials
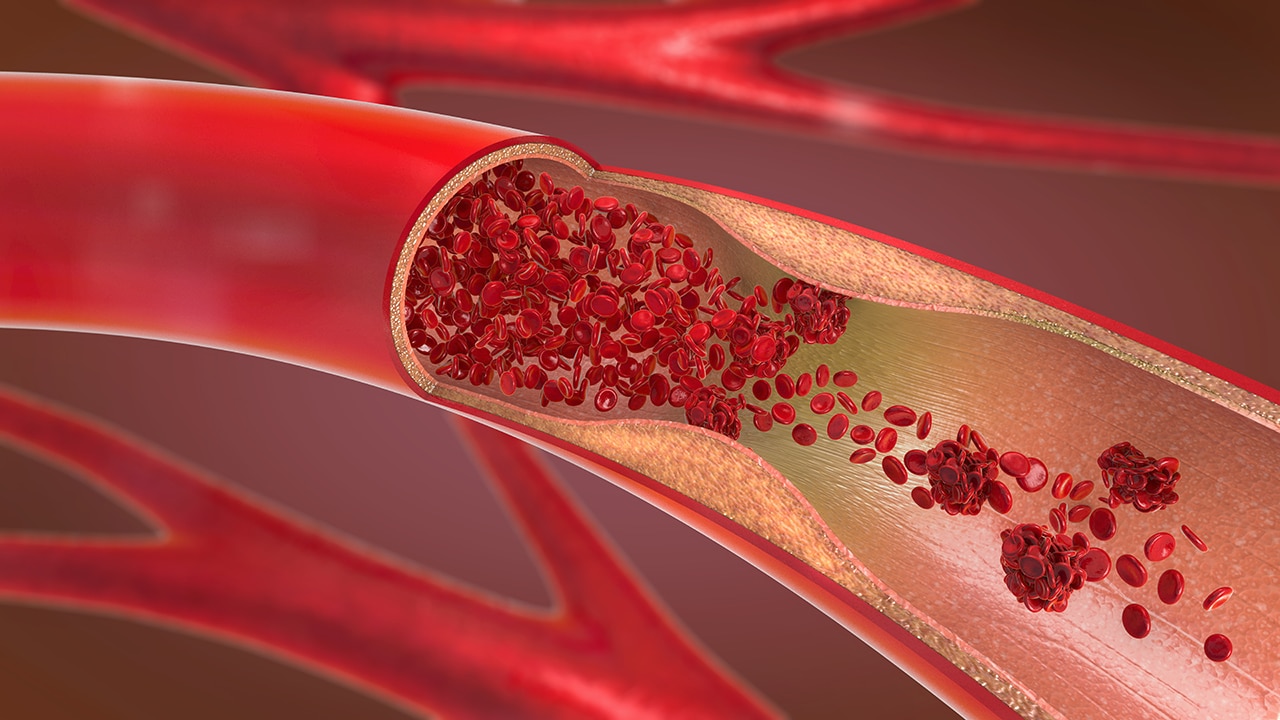
Patients with acquired hypercoagulable states or hereditary thrombophilia are more likely to develop clots, venous thrombosis, and arterial thrombosis, than healthy individuals. Venous thrombosis and pulmonary embolism are associated with significant morbidity and mortality.
The most common acquired risk factors for hypercoagulability and thrombosis are as follows [1] :
-
Advanced age
-
Immobilization
-
Inflammation
-
Pregnancy
-
Oral contraceptive use
-
Obesity
-
Diabetes mellitus
-
Hormone replacement therapy
-
Cancer (especially adenocarcinoma)
-
Antiphospholipid syndrome
Given the high prevalence of obesity and diabetes in the United States, and the aging of the population, the incidence of thrombosis is likely to increase.
Idiopathic (unprovoked) venous thrombotic events are defined as the occurrence of venous thrombosis in the absence of any of the risk factors listed above. About 50% of patients presenting with a first idiopathic venous thrombosis have an underlying thrombophilia.
Hereditary thrombophilias should be suspected in individuals with a history of recurrent thromboembolism, thrombosis at a young age (< 40 years), and/or a family history of thrombosis. Hereditary thrombophilias include the following:
-
Factor V Leiden
-
Prothrombin 20210A
-
Protein C deficiency
-
Protein S deficiency
-
Antithrombin deficiency
Deficiencies of anticoagulant factors may also be acquired.
Risk of venous thromboembolism is increased in individuals with chronic hemolytic anemias. [2] These may be inherited (eg, sickle cell anemia, [3] beta thalassemia, paroxysmal nocturnal hemoglobinuria)or acquired.
The objectives of this article are to provide an overview of hereditary and acquired hypercoagulability, to discuss indications for initiating a workup, and to review the selection and interpretation of laboratory tests for these disorders. The indications and options for anticoagulant therapy and prophylaxis, as well as the advantages and adverse effects of low molecular weight heparin (LMWH), direct thrombin, and factor Xa inhibitors are discussed.
For patient education information, see Blood Clots, Deep Vein Thrombosis, Pulmonary Embolism, and Inherited Blood-Clotting Problems.
COVID-19
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (COVID-19) is associated with hypercoagulability. COVID-19 can damage vascular endothelium, affecting many organs, promoting hypercoagulability and causing arterial and venous micro- and macrothrombosis. [4] The incidence of clotting events in patients with COVID-19 varies from 11% to 70%, depending on case series, severity of disease, and predisposing factors. [5] A study by Kiraz et al found that the presence of factor V Leiden contributes strongly to the development of thrombosis in COVID-19. [6]
In addition to high rates of DVT and pulmonary embolism, several reports of arterial thrombosis have been noted, including stroke, myocardial infarction, and limb ischemia. The inciting event is suggested to be the attachment of the coronavirus spike protein to the vascular endothelial angiotensin-converting enzyme 2 (ACE2) receptor. [5] This transforms the luminal surface of the blood vessel from a thromboresistant to a thrombogenic surface, facilitating microclot formation there.
Coagulation abnormalities noted in COVID-19 patients include high levels of D-dimer, von Willebrand factor (vWF) antigen and activity, and factor VIII activity consistent with a hypercoagulation associated with a severe inflammatory state, [7] rather than disseminated intravascular coagulation (DIC). Italian researchers have used thromboelastography (TEG) and standard coagulation tests to confirm hypercoagulability. [8] While abnormal coagulation studies such as increasing D-dimer levels have prognostic value, intervention in the absence of clinical indications is not typically recommended.
Early in the pandemic, limited data available suggested increasing intensity of anticoagulation as a reasonable approach. However, more recent evidence suggests that prophylactic-dose anticoagulation is as effective as higher-intensity (ie, therapeutic-dose) anticoagulation in reducing the risk of venous thromboembolism (VTE) in patients with COVID-19, with a trend toward lower risk of bleeding. [9, 10] Based on the currently available evidence, several societies, including the American Society of Hematology (ASH), suggest using prophylactic dosing for patients hospitalized for COVID-19, including those in the intensive care unit (ICU), in the absence of VTE. [11]
Therapeutic-dose anticoagulation is recommended for patients with documented VTE, and in whom VTE is strongly suspected but cannot be confirmed due to unavailability or feasibility of confirmatory testing. In patients without VTE, post-discharge prophylactic anticoagulation is not recommended, excepting patients with major prothrombotic risk factors such a history of VTE, trauma, or recent major surgery. In COVID-19 patients who have not been admitted to the hospital, anticoagulation is typically not used but may be appropriate for patients with other thrombotic risk factors, including recent major surgery, prior VTE, or immobilization.
Vaccine-induced immune thrombotic thrombocytopenia
COVID-19 vaccination may be associated with thrombosis and thrombocytopenia, as observed in a small number of patients who received ChAdOx1 CoV-19 vaccine (AstraZeneca) and Ad26.COV2.S vaccine (Johnson & Johnson [J&J]), both of which utilize recombinant adenoviral vectors [12, 13] This syndrome has been termed thrombosis with thrombocytopenia syndrome (TTS) or vaccine-induced immune thrombotic thrombocytopenia (VITT).
As of March 2021, the European Medicines Agency (EMA) had identified a total of 169 cases of cerebral venous sinus thrombosis and 53 cases of splanchnic vein thrombosis in more than 35 million people who received the AstraZeneca vaccine. [14] In the United States, as of May 12, 2021, the Centers for Disease Control and Prevention (CDC) had identified 28 patients with TTS among the more than 8.7 million persons vaccinated with J&J vaccine; most of those were women aged 18 to 49 years. [15]
VITT is characterized by arterial or venous thrombosis, often at unusual sites (eg, cerebral venous sinus or splanchnic vein thrombosis), along with mild to severe thrombocytopenia. It is mediated by platelet-activating antibodies against platelet factor 4 (PF4) after vaccination, leading to platelet activation, coagulation cascade stimulation, thrombosis, and thrombocytopenia. [12]
VITT should be suspected in patients who develop any of the following signs and symptoms 4 to 30 days after receiving the J&J or AstraZeneca COVID-19 vaccine:
-
Severe headache
-
Visual changes
-
Abdominal pain
-
Nausea, vomiting
-
Shortness of breath
-
Leg pain or swelling
-
Petechiae or bleeding
The initial workup includes the following:
-
Complete blood cell count (CBC)
-
Imaging for thrombosis
-
Coagulation panel including prothrombin time (PT), activated partial thromboplastin time (aPTT), D-dimer, fibrinogen, and an enzyme-linked immunosorbent assay (ELISA) for PF4-heparin complex
A positive PF4-heparin ELISA is confirmatory of VITT. Initiating appropriate treatment should not be delayed until the results of confirmatory testing.
The management of VITT is similar to the treatment of heparin-induced thrombocytopenia (HIT). Treatment consists of high-dose intravenous immune globulin (IVIG) 1g/kg daily for 2 days, along with non-heparin anticoagulation with parenteral direct thrombin inhibitors such as argatroban or bivaluridin, or fondaparinux. Heparin and platelet transfusions should be avoided.
Pathophysiology
Hemostasis is highly regulated to maintain a delicate balance between controlling bleeding in response to injury and avoiding excess procoagulant activity, to prevent hypercoagulability and thrombosis. The Virchow triad identifies the three underlying factors that are thought to contribute to thrombosis: hypercoagulability, hemodynamic dysfunction (ie, stasis—from immobilization or peripheral venous obstruction—or turbulence), and endothelial injury/dysfunction.
Hypercoagulability can result from the release of procoagulants from tumor cells or the presence of antiphospholipid antibodies (lupus anticoagulants). Insufficient inactivation of procoagulants due to impaired regulatory antithrombotic pathways can result in hypercoagulability. The presence of factor V Leiden or a mutant prothrombin can cause hypercoagulability.
The neutralization of activated factor Xa and thrombin are impaired in antithrombin (AT) deficiency. The formation of activated protein C (APC), which is a key down-regulator of factor V and factor VIII, may be impaired by protein C deficiency or protein S deficiency. Such deficiencies may be hereditary or acquired. [16] The ability of APC to inactivate factor V and factor VII can be impaired in individuals with mutant factor V such as factor V Leiden. This is known as APC resistance. Individuals with a mutant prothrombin (variously termed prothrombin G20210A, prothrombin G2010A, and mutant factor II) generate excess prothrombin that is associated with hypercoagulability.
Normal endothelium provides a non-thrombotic surface. Injury to endothelium is accompanied by loss of protective molecules and expression of adhesive molecules, procoagulant activity, and mitogenic factors, leading to development of thrombosis, smooth muscle cell migration, and proliferation and atherosclerosis. [17] In Behcet disease, a generalized autoimmune vasculitis and endothelial dysfunction occurs, with protean consequences that include thrombosis, mucocutaneous lesions, uveitis, and neurological abnormalities.
Thrombosis during pregnancy can be due to increased procoagulant factors, impaired fibrinolysis, venous stasis, and endothelial cell injury. [18] The risk of thrombosis is increased in patients on hormone replacement therapy. However, whether this risk is due to increased procoagulants or the presence of an underlying thrombophilia is not clear. [19]
Lupus anticoagulants are antiphospholipid antibodies that are associated with acquired hypercoagulability. The mechanisms for hypercoagulability in these patients remains poorly understood, but alteration of the regulation of hemostasis and endothelial cell injury might be responsible. [20, 21, 22] The inappropriate name for these antibodies is due to their initial discovery in patients with lupus—although they can also occur in individuals without lupus—and to their anticoagulant effect in vitro.
Non-O blood type is associated with an approximately two-fold increase in risk for venous thrombembolism. An inherited thrombophilic condition in association with non-O blood type further increases risk. A weaker, less well documented, association exists between non-O blood type and arterial thrombosis. [23]
In addition to thrombophilias resulting from individual mutations, an inherited susceptibility to venous thromboembolism may result from multigenic action. Research on multiple polymorphisms within the anticoagulant, procoagulant, fibrinolytic, and innate immunity pathways confirms a complex interrelationship that appears to increase the risk of venous thromboembolism. [24]
Thrombosis, especially venous thromboembolism, may complicate hypereosinophilia. Conditions associated with chronic hypereosinophilia include Churg–Strauss syndrome, hypereosinophilic syndrome (HES), and chronic eosinophilic leukemia. [25]
Activated protein C (APC) resistance
The ability of APC to inactivate factor V and factor VIII can be impaired in individuals with mutant factor V, such as factor V Leiden. This is known as APC resistance. Individuals with a mutant prothrombin (variously termed prothrombin 20210A, prothrombin G2010A, and mutant factor II) generate excess prothrombin that is associated with hypercoagulability. [26]
Factor V Leiden
Factor V Leiden is resistant to APC and hence not inactivated (APC resistant). About 20-60% of patients with thromboembolism have a form of APC resistance, and factor V Leiden is responsible for 95% of APC resistance.
Factor V Leiden (named after the city in the Netherlands where it was first identified, in 1994) results from a specific point mutation in the factor V gene, which is located in the long arm of chromosome one. Glutamine (Q) is substituted for arginine (R)-506 in the heavy chain of factor V (R506Q). The amino acid substitution alters the APC cleavage site on factor V, causing a partial resistance to inactivation.
About 5% of whites in the United States are heterozygous carriers of factor V Leiden. The carrier frequency among African Americans, Asian Americans, and Native Americans is less than 1% and in Hispanics is 2.5%. Carrier frequency is especially high—up to 14%—in whites of Northern European and Scandinavian ancestry. Inheritance is autosomal dominant. Most heterozygote carriers are asymptomatic while homozygotes have a high incidence of clinical thrombosis. [27]
The literature suggests that factor V Leiden is associated with increased risk of perioperative and postoperative thromboembolic events. Risk of surgery-specific morbidity and transplant-related adverse outcomes, particularly arterial thrombotic events, is also increased in patients with factor V Leiden. [28]
The 5% of APC resistance not due to factor V Leiden results from a variety of factors. These include other genetic mutations, as well as acquired conditions such as pregnancy, oral contraceptives, and lupus anticoagulant, all of which may also cause APC resistance. [27]
Prothrombin G20210A
Prothrombin G20210A is a polymorphism in a noncoding region (nucleotide 20210A) of the factor II (prothrombin) gene that consists of replacement of guanine with adenine, and results in elevated prothrombin levels. This mutation occurs primarily in white. Heterozygotes are at minimal risk for thrombosis, but homozygotes are 2- to 3-fold increased risk for developing thrombosis.
Additional risks
While persons who are heterozygous for factor V Leiden and prothrombin G20210A are at minimal risk for thrombosis, the presence of a second risk factor such as immobilization and pregnancy greatly increases the risk for thrombosis. The screening of patients for mutant Factor V and prothrombin during pregnancy and prior to initiation of hormone replacement therapy to determine whether prophylactic anticoagulation is indicated appears to be logical, but it is controversial.
Epidemiology
Frequency
United States
Lupus anticoagulants and antiphospholipid syndromes are present in 4-14% of the population. Table 1 shows the incidence of hereditary hypercoagulable disorders in the general population and the risk for thrombosis and recurrent thrombosis. [29, 30] Other underlying risk factors are elevated levels of factor VIII, fibrinogen, and other coagulation factors. Increases in type-1 plasminogen activator inhibitor (PAI-1), D-dimers, and homocysteine are also reported to be risk factors.
Table 1. Prevalence of Acquired or Hereditary Hypercoagulable Disorders and Risks of Venous Thrombosis. (Open Table in a new window)
Condition |
Prevalence in General Population (%) |
Relative Risk of VTE (%) |
Relative Risk of Recurrent VTE (%) |
Factor V Leiden (heterozygous) |
3-7 |
4.3 |
1.3 |
Prothrombin 20210A (heterozygous) |
1-3 |
1.9 |
1.4 |
Protein C deficiency (heterozygous) |
0.02-0.05 |
11.3 |
2.5 |
Protein S deficiency (heterozygous) |
0.01-1 |
32.4 |
2.5 |
Antithrombin deficiency (heterozygous) |
0.02-0.04 |
17.5 |
2.5 |
VTE = Venous thromboembolism |
|||
A study by Couturaud et al sought to identify risk factors and quantify the risk of venous thromboembolism in first-degree relatives of patients with a first episode of unprovoked venous thromboembolism. [30] The investigators found a prevalence of 5.3% of previous venous thromboembolism in the first-degree relatives. The strongest predictor of venous thromboembolism in this group was thrombosis at a young age. However, the presence of factor V Leiden or G20210A prothrombin genes in patients were weak independent predictors of venous thromboembolism in relatives. [30]
Mortality/Morbidity
Morbidity and mortality in patients with hypercoagulable states and thrombophilia are primarily due to venous thrombosis and pulmonary embolism. Pulmonary embolism is associated with a 1-3% mortality rate. The incidence of factor V Leiden and prothrombin 20210A is significantly greater than that of protein C, protein S, and antithrombin III (ATIII) deficiencies. However, the risk of venous thrombosis in protein C, protein S, and ATIII deficiencies is greater than in factor V Leiden and prothrombin 20210A, as shown in Table 1, above.
The risk for thrombosis can be markedly increased in patients with two or more risk factors for thrombosis. Any multiplicity of risk factors, whether hereditary thrombophilias or acquired risks, increases the risk for thrombosis.
Race-, Sex-, and Age-related Demographics
For details on the effects of race and sex on hereditary and acquired hypercoagulability, see the following articles [31, 32] :
The risk for thrombosis increases with age and associated immobility.