Practice Essentials
Tympanic membrane perforations (TMPs) can result from infection (acute or chronic) or trauma, or be secondary to otologic procedures (iatrogenic). Perforations can be temporary or chronic, and their effect varies with size, location on the drum surface, and the associated pathologic condition. Most TMPs are diagnosed using routine otoscopy. Medical therapy for perforations is directed at controlling otorrhea.
Infection is one of the principal causes of TMPs. Acute otitis media may cause rupture of the drum and generally resolves following control of the infection. [1] Chronic otitis media with perforation may be associated with a chronic draining ear or cholesteatoma. [2] Traumatic perforations occur from blows to the ear, severe atmospheric overpressure, exposure to excessive water pressure (eg, in scuba divers), and improper attempts at wax removal or ear cleaning. Trauma from cotton swabs is a relatively common cause of perforation. Traumatic perforations often resolve spontaneously, particularly when associated with swab use. [3]
Diagnosis and management of tympanic membrane perforations
The only symptom of a TMP may be associated hearing loss from decreased vibratory function of the tympanic membrane. Perforations associated with infection may present with drainage (otorrhea) or pain (otalgia). Most TMPs are diagnosed using routine otoscopy. Small perforations may require otomicroscopy for identification. Some hearing screening programs include middle ear impedance testing, or tympanometry. Screening tympanometry may reveal abnormalities consistent with perforation. Routine formal audiometric evaluation is necessary upon initial TMP workup before any repair attempt, whether in the office or the operating room.
The goal of medical therapy for perforations is otorrhea control. Some topical eardrops carry the risk of ototoxicity when exposed to the middle ear. In the setting of a TMP, eardrops containing gentamicin, neomycin sulfate, or tobramycin should be avoided.
With regard to surgery, select patients may be candidates for one of the available office treatments. Such management has the best chance of working when the perforation is small and dry and does not involve the umbo nor the annulus. The simplest, but least effective, in-office operation is freshening of the edges of the TMP followed by application of a small patch of cigarette paper (ie, paper patch). [4]
Another in-office treatment, a fat-plug tympanoplasty, is performed by obtaining a small plug of fat from the ear lobe, with the patient under local anesthesia (although this procedure may also be performed under general anesthesia). The TMP is prepared by anesthetizing its margins with carefully applied phenol solution. Next, the edges are mechanically debrided with microcup forceps. The fat is then tucked into the perforation, extending both into the canal and into the middle ear space. It is important to retract the fat slightly to prevent the edges of the perforation from growing inward to the middle ear and to avoid the formation of a cholesteatoma. The success rate is similar to paper patch but inferior to more formal tympanoplasty; moreover, it is dependent on the location of the perforation. [5]
More formal tympanoplasty can be performed with the patient under local or general anesthesia. In these cases, an incision may be made behind the ear or entirely through the ear canal, depending on the location and size of the TMP. Repair requires preparation of a suitable bed for placement of a graft. Graft options include temporalis fascia, perichondrium, cartilage, and synthetic material. Grafts may be placed medially or laterally to the perforation, or in a combined position. [6]
Epidemiology
Frequency
Incidence of tympanic membrane perforation (TMP) in the general population is unknown. One survey found that that 4% of a population of Native American children had TMP. [7] Another study found that 3% of children treated with ventilation tubes had the condition. [8] However, the incidence in the general population has not been studied. Even the exact number of surgical TMP repairs performed each year is unknown. Analysis of government statistics indicates that perhaps 150,000 tympanoplasties are performed per year in a population of 280 million.
Etiology
Infection is the principal cause of tympanic membrane perforation (TMP). Acute infection of the middle ear may cause a relative ischemia in the drum concurrent with increased pressure in the middle ear space. This leads to a tear or rupture of the eardrum that is usually preceded by severe pain. If the perforation does not heal, it leaves a residual TMP.
A prominent school of thought now advocates less aggressive use of antibiotics. Those who hold this position recognize that many episodes of otitis media are caused by viruses, so they resolve spontaneously; advocates of this position desire to slow emergence of antibiotic-resistant bacterial strains. Evidence is emerging that an increased incidence of acute mastoiditis is resulting from reduced use of antibiotics. [9] It remains to be seen whether increased incidence of perforation and other complications of otitis media, such as brain abscess, meningitis, and septic sigmoid sinus thrombosis, also occur.
A prospective study by Marchisio et al. indicated that an association exists between recurrent episodes of acute otitis media (AOM) and an increased risk for the development of spontaneous tympanic membrane perforation. The study involved 177 children with AOM complicated within 12 hours by spontaneous tympanic membrane perforation. Within that group, recurrent spontaneous tympanic membrane perforation occurred in 92% of those with recurrent AOM and in only 16.9% of those without recurrent AOM. The most common pathogen detected in the middle ear fluid of the study’s children was nontypeable Haemophilus influenzae. [10] Ear canal infections rarely cause TMP. When this occurs, it is often associated with infection by Aspergillus niger.
Traumatic perforations may result from blows to the ear (eg, being struck with the flat of the hand; falling from water skis with the head hitting the water surface, ear down). [11] Exposure to severe atmospheric overpressure from an explosion can tear the drum. [12] TMP from water pressure occurs in scuba divers, usually in a drum with atrophy from previous disease. Objects used to clean the ear canal can perforate the drum (ie, cotton swab trauma).
Inexpertly performed irrigation of the ear canal for wax can lead to perforation. In some settings, when irrigation for cerumen is relegated to medical assistants, otolaryngologists may see 10-20 patients per year with this injury. Evidence exists that such perforations are less likely to heal spontaneously. [13]
TMP is intentionally created whenever a surgeon makes an incision in the eardrum (myringotomy). When pressure-equalizing tubes (ventilating tubes) are placed, the TMP purposely is held open. Failure of surgically created openings to heal when the tube extrudes results in chronic TMP. Roughly 1% of patients who undergo a myringotomy with ventilation tube insertion will develop a chronic perforation. [14] In some patients with chronic eustachian tube dysfunction, however, the presence of a dry, chronic perforation may actually be helpful for ventilation.
Pathophysiology
Many tympanic membrane perforations resolve spontaneously. At times, a perforation heals with a thin membrane consisting only of mucosal and squamous epithelial layers, without a fibrous middle layer. Such a neomembrane may be so thin that it is mistaken for an existing perforation instead of a healed one. [15] Neomembranes may retract deeply into the middle ear, sometimes making them more difficult to distinguish from actual perforations, particularly in the setting of coexisting ventilation issues and negative middle ear pressure. Examination under the operating microscope resolves ambiguity and is recommended. Deep retraction, especially in the posterior-superior quadrant of the drum, may cause erosion of the ossicles or precede cholesteatoma formation.
If bacteria-contaminated water enters the ear canal, the presence of a perforation renders the ear more susceptible to infection. Water precautions are therefore recommended, particularly for large perforations, including the use of earplugs while swimming and avoidance of submerging the head in water when possible. Water surface tension may protect the ear from penetration through a very small perforation. The presence or history of perforation is an absolute contraindication to irrigation for cerumen removal. For patients who have undergone a myringotomy and ventilation tube insertion, consensus guidelines recommend that water precautions not be routinely used, given the limited proven benefit. [16]
A study by Park et al indicated that perforation size and pneumatization of the middle ear and mastoid affect the degree of conductive hearing loss in cases of tympanic membrane perforation. The study involved 42 patients who underwent tympanoplasty type I, or myringoplasty, with a greater preoperative mean air-bone gap (ABG) found in association with larger perforation size and with a smaller middle ear and mastoid pneumatization volume. [17] A prospective study by Pusz and Robitschek reported that subacutely, patients in the study who suffered a tympanic membrane perforation from a combat-related blast injury had both conductive and sensorineural hearing loss, with the latter making up 49% of the loss. [18]
The conductive hearing loss resulting from a TMP appears to be greater at lower frequencies. It increases as the perforation size grows and the volume of the middle-ear and mastoid air space decreases but does not change with location. [19, 20]
Indications
Many persons live their lives with tympanic membrane perforations (TMPs) that are entirely without symptoms; they may even benefit from a perforation if they have significant, coexisting eustachian tube dysfunction and poor ventilation. Repair of such lesions is usually not indicated. Perforations may be associated with recurrent infection when exposed to water. In swimmers, divers, and other water sports enthusiasts, repair may be indicated as a quality-of-life issue. Hearing loss may be present, especially with larger perforations, and may be a reason for repair. [21] Because a risk to residual hearing exists with every operation on the ear drum, a risk-benefit analysis in which the patient participates is mandatory. [22] For example, question whether the person may be helped just as much with use of a hearing aid.
Relevant Anatomy
The tympanic membrane, also called the eardrum (or just the drum), is a stiff (but flexible), translucent, diaphragmlike structure. The eardrum moves synchronously in response to variations in air pressure, which constitute sound waves. The drum's vibrations are transmitted through the ossicular chain to the cochlea. In the cochlea, vibratory mechanical energy changes to electrochemical energy and streams via the eighth cranial nerve to the brain. The tympanic membrane and its attached ossicles thus act as a transducer, changing one form of energy into another form. (See the image below.) The biomechanical coupling of this conductive system produces a gain that can help to overcome the impedance mismatch as the energy undergoes a phase shift from air to the liquid of the inner ear.
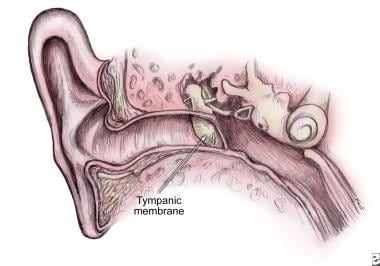 Tympanic membrane (TM) as continuation of the upper wall of external auditory canal (EAC) with angle of incline up to 45 degrees on the border between middle ear and the EAC.
Tympanic membrane (TM) as continuation of the upper wall of external auditory canal (EAC) with angle of incline up to 45 degrees on the border between middle ear and the EAC.
The tympanic membrane has two distinct zones. The larger of the two zones is the pars tensa. This zone consists of a tough and resilient fibrous layer with a diaphanous mucosal layer inside and squamous epithelium outside. The smaller zone is the pars flaccida, which lies superior to the suspensory ligaments of the malleus and lacks a fibrous layer.
Contraindications
Tympanic membrane perforation (TMP) may be unilateral or bilateral. Select the worse-hearing ear first when performing bilateral TMP repair. If increased hearing loss complications ensue, the better-hearing ear remains uninjured. For the same reason, if the TMP is present in a patient's single hearing-capable ear, a frank discussion must be had with the patient regarding the risk of further hearing loss.
-
Tympanic membrane (TM) as continuation of the upper wall of external auditory canal (EAC) with angle of incline up to 45 degrees on the border between middle ear and the EAC.






