Practice Essentials
Nitrogen dioxide (NO2) is a reddish-brown gas that has a sharp, harsh odor at higher concentrations but may be clear and odorless at lower, but still harmful, concentrations. NO2 is one of several pollutants formed as a byproduct of burning fuel or combustion. Common sources include cars, trucks, buses, power plants, and diesel-powered heavy engines, but smaller significant sources also include kerosene burners, gas space heaters, and tobacco smoke. [1]
Thus, NO2 toxicity is an occupational hazard for arc welders, firefighters, military and aerospace personnel, traffic personnel, and those working with explosives. [2] In addition, individuals who spend significant amounts of time near major roadways or in traffic may be at considerably increased risk of long-term exposure. [3]
Finally, NO2 can also form from noncombustion sources. When farm silos are filled with fresh organic material (eg, corn, other grains), anaerobic fermentation of the crops results in NO2 production. Within a few hours, high levels of NO2 develop on top of the silage. This may also occur with silage bags, but this risk is lower given natural outdoor ventilation. In either case, farmers who enter silos, work with silage bags, or remain near open silo hatches during the first 10 days after filling may experience NO2 toxicity in a phenomenon known as silo filler’s disease.
Signs and symptoms
The diagnosis of NO2 toxicity largely depends on the history of exposure. If possible, inquire about exposure and occupation. Welders, firefighters, military and aerospace personnel, individuals working with explosives, traffic personnel, and farmers generally have higher risk of short-term exposure than those in other occupations. Additionally, individuals living in particular urban areas or near congested highways may have increased risk of long-term low-level exposure.
NO2 is a mucous membrane irritant commonly associated with other toxic products of combustion. Symptoms most commonly range from mild cough and mucous membrane irritation to severe exacerbations of underlying pulmonary diseases (eg, COPD or asthma) and, in extreme cases, death. Suspect methemoglobinemia in patients exposed to NO2 who exhibit cyanosis or dyspnea. The initial absence of significant symptoms does not exclude a subsequent development of serious disease.
Common signs and symptoms are as follows:
-
New or worsening cough and/or wheezing (most common)
-
Eye, nose or throat irritation
-
Light-headedness or headache
-
Dyspnea (shortness of breath)
-
Chest tightness
-
Choking
-
Chest pain
-
Diaphoresis (sweating)
In addition, the following signs and symptoms may appear acutely or persist for days to weeks, and may indicate severe or worsening disease:
-
Severe shortness of breath
-
Turning blue in the lips, fingers, or toes
-
Rapid breathing
-
Rapid heart rate
-
Fever
-
More frequent use of inhalers
See Presentation for more detail.
Diagnosis
No laboratory studies that are specific to the diagnosis of NO2-induced illness have been reported. However, the following blood studies can be helpful in excluding other causes of the symptoms:
-
Arterial blood gas (ABG) levels
-
Lactate level
-
Methemoglobin (MHb) level
-
Complete blood cell count (CBC) with peripheral smear
-
Glucose levels
Other studies are as follows:
-
ECG can rule out cardiac events
-
Pulmonary function tests (PFTs) should be performed as soon as possible, to establish a baseline
-
Chest radiography findings range from normal to noncardiogenic pulmonary edema to that of soft reticulonodular infiltrates (see the image below)
 Noncardiogenic pulmonary edema following exposure to nitrogen dioxide. Courtesy of Dr. Ann Leung, Department of Radiology, Stanford University Hospital.
Noncardiogenic pulmonary edema following exposure to nitrogen dioxide. Courtesy of Dr. Ann Leung, Department of Radiology, Stanford University Hospital.
See Workup for more detail.
Management
Treatment varies with the severity of symptoms, as follows:
-
If no initial symptoms are present, observe the patient for at least 12 hours for hypoxemia
-
Hospitalize the patient for 12-24 hours for observation or longer if gas exchange is compromised
-
Administer oxygen to hypoxemic patients
-
Consider high-dose steroids for patients with pulmonary manifestations
-
Intubation and mechanical ventilation may be necessary if gas exchange is severely impaired
-
Administer volume expanders cautiously
-
Transfer to a tertiary care center for further diagnostic evaluation and ventilator support may be necessary
-
Bronchiolitis obliterans, which may develop 2-6 weeks after NO 2 exposure, may require 6-12 months of corticosteroid therapy
-
Inhaled sympathomimetics (eg, albuterol), anticholinergics (eg, ipratropium bromide), and steroids (eg, fluticasone propionate) may be indicated if the patient develops symptoms of reactive airway disease
See Treatment and Medication for more detail.
Background
Harmful effects of nitrogen dioxide (NO2) often occur from either high-level short-term or low-level long-term exposures. In an era founded largely on the success and availability of fossil fuels, the realization of the harmful effects of fossil fuel byproducts has become an increasing public health concern. Clean air is recognized as a basic requirement for human health and well-being, alongside access to clean water and sanitation. [4] NO2 in particular is among the most commonly recognized components of air pollution. NO2 and the other pollutants it consorts with are increasingly associated with worsening lung function, increased risk of ischemic heart disease and stroke, increased rates of hospital admissions, and even increased rates of mortality. [5, 6, 3]
Registry numbers for NO2 include the following:
-
American Chemical Society's Chemical Abstract Service (CAS): CAS #10102-44-0
-
United Nations/Department of Transportation: UN#1067
-
National Institute of Occupational Safety and Health (NIOSH) Registry of Toxic Effects of Chemical Substances (RTECS): QW 9800000
NO2 is poorly soluble in water. As a result, when inhaled, it easily bypasses the moist oral mucosa and upper airways and penetrates deep into the lower respiratory tract. Toxicity depends largely on the concentration and duration of exposure, as well as an individual’s baseline pulmonary function. Elderly individuals or individuals with COPD or asthma are at much higher risk of adverse events, are more susceptible to developing infections, and may experience more severe symptoms than healthy individuals with normal pulmonary function.
Current World Health Organization (WHO) guidelines, updated in 2021, recommend limiting annual average long-term NO2 exposure to less than 10 µg/m3 (approximately 5 parts per billion [ppb]), with the following interim targets as incremental steps in a progressive reduction of air pollution in areas where pollution is high [4] :
-
Target 1: 40 µg/m 3 (approximately 20 ppb)
-
Target 2: 30 µg/m 3 (approximately 15 ppb)
-
Target 3: 20 µg/m 3 (approximately 10 ppb)
For short-term (24-hour) exposure, the recommended limit is 25 µg/m3 (approximately 12.5 ppb), defined as the 99th percentile (equivalent to three to four exceedance days per year) of the annual distribution of 24-hour average concentrations. The interim targets in areas where pollution is high are as follows: [4]
-
Target 1: 120 µg/m 3 (approximately 60 ppb)
-
Target 2: 50 µg/m 3 (approximately 25 ppb)
These values are based on using NO2 as a general marker for the complex mixture of pollutants generated by combustion. The recommended values are also based on values shown to have direct effects on the pulmonary function of asthmatic people. [4]
In the United States, current Environmental Protection Agency (EPA) standards are set at less than 100 ppb for 1-hour exposures and less than 53 ppb annual average for long-term exposure. [7] States such as California may have more stringent state regulations. Specific regions, including the Northeast corridor, Chicago, and Los Angeles have historically high levels of NO2. [8] Nationally, however, NO2 levels in the US have been falling steadily for decades and are currently well within EPA standards. See the EPA’s Nitrogen Dioxide Trends for specific NO2 level trends in a particular national region. [9] Also see the graph below.
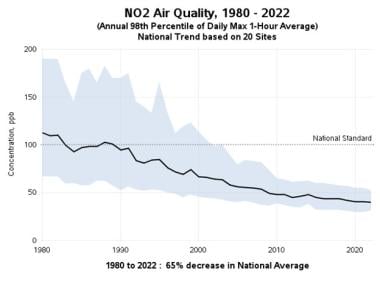 Nitrogen dioxide air quality from 1980 to 2022. Courtesy of the Air Quality Analysis Group, US Environmental Protection Agency (EPA).
Nitrogen dioxide air quality from 1980 to 2022. Courtesy of the Air Quality Analysis Group, US Environmental Protection Agency (EPA).
Some studies suggest that chronic exposure to NO2 may predispose individuals to the development of chronic lung diseases, including infection and COPD, and particularly asthma in children. In a study of 728 children with active asthma, children in households with gas stoves (which increase the levels of NO2) had an increased likelihood of wheezing, shortness of breath, and chest tightness. [10]
More recent literature on NO2 focuses on its association with nitrous acid (HONO), a molecule that can be formed as a primary product of gas combustion or by the reaction of NO2 with surface water. [11, 12, 13, 14] Although early data are inconclusive, some studies suggest that HONO may contribute to the adverse health outcomes previously attributed to NO2.
Pathophysiology
In the lung, nitrogen dioxide (NO2) hydrolyzes to nitrous acid (HNO2) and nitric acid (HNO3), which can then cause chemical pneumonitis and pulmonary edema. Because NO2 is poorly water soluble, it hydrolyzes more slowly than other water-soluble gases, resulting in deep lung injury in the bronchioles and alveoli. Type I pneumocytes and ciliated airway cells are primarily affected, but damage also occurs from free radical generation, which results in protein oxidation, lipid peroxidation, and cell membrane damage. A proposed pathway involves oxidation of mitochondrial cytochrome c, [15] which can result in electron transport chain decoupling and cellular apoptosis.
The chemical irritation of the alveoli and bronchioles results in rapid destruction of the epithelial cells and breakdown of the pulmonary capillary bed. The subsequent release of fluid results in pulmonary edema.
Nitrogen oxides can alter immune function and macrophage activity, leading to an impaired resistance to infection. Viral illnesses such as influenza are commonly associated infections. Significant exposure can also result in methemoglobinemia. NO2 binds to hemoglobin with great affinity, forming nitrosyl hemoglobin, which is readily oxidized to methemoglobin. Methemoglobin results in a leftward shift of the oxygen disassociation curve, which impairs the oxygen delivery and compounds the already present hypoxia.
In untreated cases, fibrous granulation tissue may develop within small airways and alveolar ducts, resulting in bronchiolitis obliterans. As its name suggests, bronchiolitis obliterans refers to an inflammatory process that results in the progressive partial or complete obliteration of the small airways. This results in obstructive lung disease. (See Constrictive Bronchiolitis Obliterans: The Fibrotic Airway Disorder.)
Briefly, bronchiolitis obliterans is classified in two subtypes: proliferative and constrictive. Proliferative bronchiolitis is more common and is characterized by the development of steroid-reversible intraluminal polyps that obstruct the small airways. By contrast, constrictive bronchiolitis is a more diffuse and chronic process characterized by concentric thickening and destruction of bronchioli. While fumes containing sulfur or ammonia have been associated with constrictive bronchiolitis, proliferative bronchiolitis is more common with nitrogen dioxide toxicity.
Etiology
Occupational risk for nitrogen dioxide (NO2) exposure is high for the following workers:
-
Farmers, particularly those who work near silos
-
Firefighters
-
Arc welders
-
Military personnel, particularly those working with explosives or in regions with poor air-quality control
-
Aerospace workers (missile fuel)
-
Traffic officers, particularly those standing at high-volume intersections
-
Miners
In addition, workers in any occupation that involves the production, transportation, or use of nitric acid are at risk. Gas- and kerosene-fired household appliances and motor vehicle exhaust all pose significant risk of exposure. For example, there are multiple reports of nitrogen dioxide exposure occurring in ice skating rinks secondary to poor ventilation and exhaust from ice resurfacing machines [16] and exposures in mines where poor ventilation results in exposure to fumes from diesel engine equipment or explosives.
Silo filler’s disease
Silos filled with freshly cut corn, oats, grass, alfalfa, or other plant material generates oxides of nitrogen within hours. Maximum concentrations of NO2 are reached within 1-2 days, and then the levels begin to fall after 10-14 days. In well-sealed silos, NO2 can be present for weeks. Silage that is heavily fertilized, has experienced drought, or is derived from immature plants produces much higher concentrations of nitrogen oxides within the silo. The same phenomenon occurs with silage bags, but because of better natural ventilation, the hazard is lower.
During storage, NO2, which is 1.5 times heavier than air, can remain in deep depressions of the silage material. Exposure can develop while attempting to level the silage without proper ventilation or breathing apparatus. One documented case occurred in an individual who traversed the ladder at the opening of a silo. The heavier-than-air NO2 flowed down the side of the silo, exposing the worker to toxic levels of gas.
Epidemiology
In the United States, manufactured sources of nitrogen oxides primarily from burned fuels exceed 19.4 million metric tons. The US Environmental Protection Agency (EPA) has regulations for monitoring nitrogen dioxide (NO2) concentrations and has historically found outdoor ambient air concentrations highest in large urban regions such as the New York metropolitan area, Chicago, and Los Angeles. [8]
The World Health Organization (WHO) estimated that ambient (outdoor air pollution) in both cities and rural areas caused 4.2 million premature deaths worldwide in 2019. Approximately 89% of those premature deaths occurred in low- and middle-income countries, especially in the Western Pacific and South-East Asia regions. [17]
In the United States, the EPA estimates that 16% of US housing units are located within 100 yards of a major highway, railroad, or airport. This translates to roughly 48 million people at increased risk of exposure. In addition, this population likely includes an increased proportion of lower-income individuals and minorities. [3]
Individuals at increased risk of adverse effects include those with underlying asthma or COPD, those with other pulmonary diseases with poor pulmonary function (eg, interstitial lung disease, pulmonary fibrosis, pulmonary hypertension), and those with existing cardiovascular disease and low oxygen reserve. Elderly persons and children are also at increased risk of respiratory infections or asthma exacerbations, respectively. [3]
Time-series studies on ozone (formed by the oxidation of NO2 in ambient air) reported by the WHO suggested a 1-2% increase in attributable daily deaths when ozone concentrations exceeded 100 µg/mL (approximately 47.3 ppb). Levels above 160 µg/mL (approximately 75.7 ppb) were associated with an estimated 3-5% increase in daily mortality, even in purportedly healthy individuals. Levels above 240 µg/mL (approximately 114 ppb) were associated with a 5-9% increase. All numbers of daily mortality are relative to background levels of ozone at 70 µg/mL (33.1 ppb).
Silo filler's disease is prevalent during the harvest months of September and October. An estimated annual incidence of 5 cases per 100,000 silo-associated farm workers per year was reported in New York. [18, 19] Silo filler's disease is likely significantly underreported.
Prognosis
Overall, the long-term prognosis is good for patients who survive the initial exposure to nitrogen dioxide (NO2). Some cases of NO2 toxicity resolve with no persistent or delayed symptoms. The long-term prognosis for an individual patient can be determined by conducting follow-up pulmonary function tests.
In patients with lung damage from NO2, improvement in pulmonary function may take weeks or months. Permanent mild dysfunction, likely due to bronchiolitis obliterans, may occur. This manifests as the following:
-
Mild hyperinflation
-
Abnormal flow at 50% or 75% of vital capacity (V max50, V max75)
-
Reduction in forced expiratory flow from 25-75% of vital capacity (FEF 25-75)
-
Increased respiratory resistance
-
Airway obstruction
The lungs clear quickly with steroid treatment, and the chest radiograph may reveal no evidence of residual lung damage. Deconditioning can be treated with a pulmonary rehabilitation program.
Complications
Complications include secondary infection and bronchiolitis obliterans. Infection (eg, pneumonia) is possible because of the mucosal injury caused by pulmonary edema and the inhibition of immune function by NO2. Bronchiolitis obliterans consists of fibrous granulation tissue that develops within small airways and alveolar ducts. It occurs weeks or months after the initial incident.
In a number of meta-analyses, NO2 exposure in pregnant women has been associated with increased risk of coarctation of the aorta in their offspring. [20] An analysis of data from the National Birth Defects Prevention Study found that NO2 exposure was positively associated with ventricular septal defects, but the risk could be reduced with higher intake of methyl donor micronutrients (eg, methionine, choline). [21]
A meta-analysis of nine European epidemiologic studies found that birth weight decreases and the risk of preterm birth increases with increased maternal NO2 exposure, although the findings were not statistically significant. The authors of the analysis concluded that the findings suggest increased air pollution exposure during pregnancy may contribute to lower birth weight, but further population-based studies are needed. [22]
Mortality/morbidity
NO2 poisoning may result in mortality or short-term and long-term morbidity. Manifestations of NO2 toxicity are related to the concentration inhaled, duration of exposure, and time since exposure.
Illness from acute exposure is usually mild and self-limiting; however, some exposure results in pulmonary edema, bronchiolitis obliterans, or rapid asphyxiation. In one study, approximately one third of people with severe exposures died. Death can result from bronchiolar spasm, laryngeal spasm, reflex respiratory arrest, or asphyxia. If sufficiently high, NO2 can displace oxygen and cause fatal asphyxiation. High concentrations can render a person helpless within 2-3 minutes.
A meta-analysis found consistent evidence of a relationship between NO2, as a proxy for exposure to air pollution from traffic, with lung cancer. The study estimated that a 10-μg/m3 increase in exposure to NO2 was associated with a 4% change in lung cancer rates. [23]
Two studies have found long-term exposure to NO2 is associated with higher risk of myocardial infarction (MI) and heart failure, mainly in men. Combined high exposure to both NO2 and road traffic noise was associated with the highest risk for both MI and heart failure. [24, 25] Long-term exposure to NO2 and road traffic noise was associated with higher risk of heart failure, mainly among men, in both single- and two-pollutant models. High exposure to both pollutants was associated with highest risk.
A systematic review and meta-analysis by Wilker et al on the role of air pollutants in risk of dementia found an overall hazard ratio per 10 μg/m3 NO2 of 1.02 (95% confidence interval, 0.98 to 1.06). The authors noted that hazard ratios were larger for studies that utilized an active case ascertainment approach, but that data are limited and more research is needed. [38]
Patient Education
In general, patients should be taught to recognize the signs and symptoms of worsening pulmonary or cardiovascular function.
Educate farm workers at risk for exposure and development of silo filler's disease. Offer the following preventive advice:
-
Stay out of silos during the 2-week danger period after the initial filling
-
Close all doors before putting in the silage
-
Go up the outside ladder to the level of silage
-
If the silo is not completely full, remove the doors that lead down to the silage
-
Enter the silo only with a complete oxygen support system (ie, air supply, self-contained breathing apparatus)
-
Ventilate the silo by opening the cover flaps and running the silo blower for 24-48 hours before entering
-
Never enter the silo alone or without a lifeline for rescue during the danger period.
-
If it is necessary to enter a silo during filling, enter immediately after the last load
Advise patients who have had a significant exposure to nitrogen dioxide (NO2) to avoid other pulmonary toxins. They should wear appropriate personal protective equipment in the workplace.
Advise patients that delayed symptoms, including life-threatening pulmonary edema and dyspnea caused by bronchiolitis obliterans, may result. Therefore, patients should be followed for a minimum of 2-3 months after exposure to monitor possible development of bronchiolitis obliterans.
-
Bronchiolitis obliterans following exposure to nitrogen dioxide. Courtesy of Dr. Ann Leung, Department of Radiology, Stanford University Hospital.
-
Noncardiogenic pulmonary edema following exposure to nitrogen dioxide. Courtesy of Dr. Ann Leung, Department of Radiology, Stanford University Hospital.
-
Nitrogen dioxide air quality from 1980 to 2022. Courtesy of the Air Quality Analysis Group, US Environmental Protection Agency (EPA).









