Practice Essentials
Vertebrobasilar atherothrombotic disease (VBATD) describes a wide spectrum of clinical entities with a common pathophysiology. Transient ischemic attacks (TIAs) in this vascular territory are also referred to as vertebrobasilar insufficiency (VBI).
In this article, VBATD describes both transient and permanent ischemic deficits as they affect posterior cerebral circulation.
Signs and symptoms
Vertebrobasilar TIAs typically have shorter duration than attacks involving the carotid territory, lasting 8 minutes on average compared with 14 minutes for carotid TIAs.
Classic symptoms of posterior region ischemia include the following: [29]
-
Vertigo
-
Visual field defects (diplopia, hemianopia)
-
Auditory phenomena (sudden sensorineural hearing loss)
-
Facial numbness or paresthesias
-
Dysphagia, dysarthria, hoarseness
-
Syncope (drop attacks)
-
Hemisensory extremity symptoms (eg, contralateral to facial component)
Vertigo is the hallmark symptom of patients experiencing ischemia in the vertebrobasilar distribut
Diagnosis
Imaging studies are the primary tools used to confirm a VBATD diagnosis.
Management
VBATD management in the emergency department varies on the basis of the patient's symptoms and condition.
-
For patients with VBATD who have experienced ischemic infarcts, management falls into 2 major categories: supportive measures and interventions to reestablish patency in the infarct-related artery or to prevent occlusion of a vessel at risk for atherothrombotic or embolic occlusion.
-
Airway issues must be addressed in patients with brainstem infarction resulting from VBATD.
-
If a hemorrhagic lesion has been excluded, patients with VBATD are treated with antiplatelet agents or, in certain circumstances, an anticoagulant such as warfarin.
Surgery is not an established treatment option for VBATD, in contrast to its value for treating carotid territory ischemia.
Background
Vertebrobasilar atherothrombotic disease (VBATD) describes a wide spectrum of clinical entities with a common pathophysiology. Transient ischemic attacks (TIAs) in this vascular territory are also referred to as vertebrobasilar insufficiency (VBI). This more commonly used term was developed in the 1950s when Fisher introduced the term carotid insufficiency to describe TIAs of the anterior circulation. These, in turn, frequently serve as the prodrome to carotid branch infarcts. Although carotid insufficiency has been dropped from common medical jargon, vertebrobasilar insufficiency persists as the term that encompasses all TIA syndromes of the posterior circulation. In this article, vertebrobasilar atherothrombotic disease describes both transient and permanent ischemic deficits as they affect posterior cerebral circulation.
Vertebrobasilar atherothrombotic disease (VBATD) deserves special attention among emergency physicians because it is difficult to diagnose and important not to misdiagnose. Signs and symptoms of VBATD overlap those of other more common benign entities (eg, labyrinthitis, vestibular neuronitis, benign paroxysmal positional vertigo).
Pathophysiology
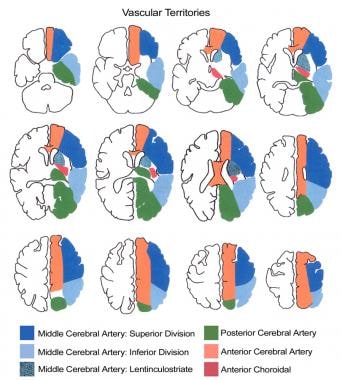
Vertebrobasilar (posterior) circulation constitutes the arterial supply to the brainstem, cerebellum, and occipital cortex. The image below shows the vascular territories of the brain.
Any interruption in blood flow to these areas may manifest in a myriad of symptoms. These symptoms are determined by which particular branch or branches of the vertebrobasilar circulation have been compromised, extent of any collateral circulation, and degree of occlusion.
The brainstem is an intensely concentrated area of neurologic activity, housing cranial nerves, the reticular activating system, and a series of ascending and descending neurosensory tracts. As a result of impaired blood flow, this compact area of neurologic activity malfunctions and results in several different but overlapping clinical syndromes.
Embolic phenomena cause infarction in vertebrobasilar territory in 9-40% of reported cases. The vertebrobasilar bed appears less susceptible than carotid circulation to embolic occlusion.
The vertebral artery is often classified into intracranial and extracranial segments; the atherosclerotic process tends to affect vertebrobasilar circulation at specific intracranial and extracranial sites. The extracranial site is defined as the initial segment of the vertebral artery just proximal to its take-off from the subclavian. The intracranial site is defined as the proximal portion of the basilar artery, just after the joining of the 2 vertebral arteries or just distal to the pontomedullary junction.
Epidemiology
Frequency
Approximately one fourth of strokes and transient ischemic attacks (TIAs) occur in the vertebrobasilar distribution. [1]
-
Brainstem infarctions have been reported in autopsy series at a rate of 2 per 1000 cases. One clinical study has suggested that the disease occurs 25% as frequently as occlusions of the carotid artery and its branches.
-
Recent developments in neuroimaging provide new perspectives about the disease's prevalence. Some studies using MRI suggest that 40% of patients with vertebrobasilar TIAs have evidence of brainstem infarction.
Mortality/Morbidity
Vertebrobasilar ischemic disease encompasses a vast spectrum of clinical syndromes, extending from subclinical to lethal brainstem infarctions.
-
Of patients who suffer infarctions in the vertebrobasilar territory, 50% report TIAs in the days or weeks (rarely months) prior to onset of the permanent deficit. A systematic review suggests that although overall mortality is no different than anterior territory ischemia, the early risk (within 7 d) of recurrent stroke or TIA progression to stroke is higher with VBATD. [1]
-
Basilar artery syndrome, which presents as a locked-in state, is caused by complete occlusion of the intracranial portion of vertebrobasilar circulation. It is a devastating disease with a mortality rate of 75-85%.
Race-, sex-, and age-related demographics
Intracranial atherosclerosis is more common among black African [34] or East Asian ethnicities. [33]
As with atherosclerosis, this disease affects men twice as often as it does women.
Vertebrobasilar ischemic disease occurs in the late decades of life (eg, 70s and 80s).
Prognosis
Vertebrobasilar transient ischemic attacks (TIAs) (ie, vertebrobasilar insufficiency) generally may have a more favorable prognosis than carotid territory TIAs because the risk of developing a completed stroke is less. Collateral circulation may account for improved outcome in these patients.
Lateral medullary infarction (Wallenberg syndrome) is characterized by persistent symptoms that last for years.
-
Vascular territories of the brain.
-
Diffusion-weighted MRI images showing a right cerebellar infarct.
-
Magnetic resonance angiography demonstrating the absence of flow in the vertebrobasilar system.
-
Right vertebral artery angiography showing an occlusion with no flow in the basilar artery.
-
Angiography performed after intra-arterial thrombolysis and angioplasty showing recanalization and perfusion of the basilar artery and its branches.
-
Hyperdense basilar artery (arrow).