Practice Essentials
Vertebral artery dissection (VAD) is a relatively rare but increasingly recognized cause of stroke in patients younger than 45 years. Although the term spontaneous VAD is used to describe cases that do not involve significant blunt or penetrating trauma as a precipitating factor, many patients with so-called spontaneous VAD have a history of trivial or minor injury involving some degree of cervical distortion. See the image below.
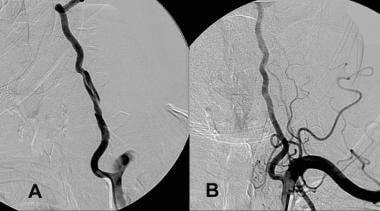 A, Dissection of the left vertebral artery secondary to guidewire injury. B, Complete resolution occurred in 6 months with only aspirin and clopidogrel (Plavix) therapy.
A, Dissection of the left vertebral artery secondary to guidewire injury. B, Complete resolution occurred in 6 months with only aspirin and clopidogrel (Plavix) therapy.
Signs and symptoms
The typical patient with VAD is a young person who experiences severe occipital headache and posterior nuchal pain following a head or neck injury and subsequently develops focal neurologic signs attributable to ischemia of the brainstem or cerebellum. The focal signs may not appear until after a latent period lasting as long as three days, however, and delays of weeks and years also have been reported. Many patients present only at the onset of neurologic symptoms.
When neurologic dysfunction does occur, patients most commonly report symptoms attributable to lateral medullary dysfunction (ie, Wallenberg syndrome). Patient history may include the following:
-
Ipsilateral facial dysesthesia (pain and numbness) [1] - Most common symptom
-
Dysarthria or hoarseness (cranial nerves [CN] IX and X)
-
Contralateral loss of pain and temperature sensation in the trunk and limbs
-
Ipsilateral loss of taste (nucleus and tractus solitarius)
-
Hiccups
-
Vertigo [1]
-
Nausea and vomiting
-
Diplopia or oscillopsia (image movement experienced with head motion)
-
Dysphagia (CN IX and X)
-
Disequilibrium
-
Unilateral hearing loss [2]
Rarely, patients may manifest the following symptoms of a medial medullary syndrome:
-
Contralateral weakness or paralysis (pyramidal tract)
-
Contralateral numbness (medial lemniscus)
Depending upon which areas of the brainstem or cerebellum are experiencing ischemia, the following signs may be present:
-
Limb or truncal ataxia
-
Nystagmus [3]
-
Ipsilateral hypogeusia or ageusia (ie, diminished or absent sense of taste)
-
Ipsilateral impairment of fine touch and proprioception
-
Contralateral impairment of pain and thermal sensation in the extremities (ie, spinothalamic tract)
-
Lateral medullary syndrome [6]
Cerebellar findings may include the following:
-
Nystagmus
-
Medial medullary syndrome
-
Tongue deviation to the side of the lesion (impairment of CN XII)
-
Contralateral hemiparesis
-
Ipsilateral impairment of fine touch and proprioception (nucleus gracilis)
-
Internuclear ophthalmoplegia (lesion of the medial longitudinal fasciculus)
See Presentation for more detail.
Diagnosis
Imaging studies in patients with suspected VAD may include the following:
-
Computed tomography (CT) scanning – Identifies subarachnoid hemorrhage [3] ; CT angiography (CTA), along with magnetic resonance angiography (MRA), are the imaging modalities of choice for vertebral artery dissections; however, CTA is less accurate in the presence of calcified arteries.
-
Four-vessel cerebral angiography [7] – Once the criterion standard for diagnosis, now largely supplanted by noninvasive techniques
-
Vascular duplex scanning – Demonstrates abnormal flow in 95% of patients with VAD, [8] but shows signs specific to VAD (eg, segmental dilation of the vessel, eccentric channel) in only 20%
-
Transcranial Doppler ultrasonography – Approximately 75% sensitive to the flow abnormalities seen in VAD useful also in detecting high-intensity signals (HITS), which are characteristic of microemboli propagating distally as a result of the dissection; ultrasonography may have a role in the initial diagnosis of dissections if CT-A or MRA are unavailable.
Because VAD occurs in young, generally healthy individuals, laboratory evaluation is directed toward establishing baseline parameters in anticipation of anticoagulant therapy, as follows:
-
Prothrombin time (PT) with international normalized ratio (INR)
-
Activated partial thromboplastin time (aPTT)
In addition, elevation of the erythrocyte sedimentation rate (ESR) may suggest vasculitis involving the cerebrovascular circulation.
See Workup for more detail.
Management
Acute management of proven or suspected spontaneous VAD is as follows [13] :
-
Anticoagulants and antiplatelet agents are the drugs of choice to prevent thromboembolic disorders; the data suggest no difference between the two modalities on outcomes and adverse effects
-
More potent agents (eg, intra-arterial thrombolytics) have been used in selected cases; there may be a role for these medications during acute ischemic events
-
Endovascular and surgical treatments are reserved for patients with concomitant complications or whose maximal medical therapy is unsuccessful
See Treatment and Medication for more detail.
Background
Vertebral artery dissection (VAD) is an increasingly recognized cause of stroke in patients younger than 45 years. [4, 14, 15, 16, 17] Although its pathophysiology and treatment closely resemble that of its sister condition, carotid artery dissection (CAD), the clinical presentation, etiology, and epidemiologic profile of VADs are unique. In particular, advances in imaging have contributed to growing awareness of this entity. [8]
Pathophysiology
An expanding hematoma in the vessel wall is the root lesion in vertebral artery dissection (VAD). This intramural hematoma can arise spontaneously or as a secondary result of minor trauma, through hemorrhage of the vasa vasorum within the media of the vessel. It also can be introduced through an intimal flap that develops at the level of the inner lumen of the vessel. Major trauma is also an increasingly recognized cause of VAD. [18]
This intramural hemorrhage can evolve in a variety of ways, resulting in any of the following consequences:
-
The hematoma may seal off and, if sufficiently small, remain largely asymptomatic.
-
If the dissection is subintimal, the expanding hematoma may partially or completely occlude the vertebral artery or one of its branches. Extensive dissections (those that extend intracranially and involve the basilar artery) result in infarctions of the brainstem, cerebellum or, rarely, the spinal cord. Subintimal dissections also may rupture back into the vertebral artery, thus creating a false lumen (pseudolumen).
-
Subadventitial dissections tend to cause pseudoaneurysmal dilation of the vertebral artery, which may compress adjacent neurologic structures. These subadventitial dissections are prone to rupture through the adventitia, resulting in subarachnoid hemorrhage. In an autopsy series of more than 100 patients with subarachnoid hemorrhage, 5% of the hemorrhages were deemed the result of VAD.
-
The intimal disruption and low flow states that arise in VAD create a thrombogenic milieu in which emboli may form and propagate distally. This results in transient ischemia or infarction.
An understanding of the anatomy of the vertebral artery is helpful. The course of the vertebral artery usually is divided into four sections as follows:
-
Segment I runs from its takeoff at the first branch of the subclavian artery to the transverse foramina of cervical vertebra C5 or C6.
-
Segment II runs entirely within the transverse foramina of C5/C6 to C2.
-
Segment III, a tortuous segment, begins at the transverse foramen of C2, runs posterolaterally to loop around the posterior arch of C1, and passes subsequently between the atlas and the occiput. This segment is encased in muscles, nerves, and the atlanto-occipital membrane.
-
Segment IV, the intracranial segment, begins as it pierces the dura at the foramen magnum and continues until the junction of the pons and medulla, where the vertebral arteries merge to join the larger proximal basilar trunk.
Spontaneous dissection of the vertebral artery usually occurs in the tortuous distal extracranial segment (segment III) but may extend into the intracranial portion or segment IV.
Etiology
Spontaneous vertebral artery dissection (VAD) is the term used to describe all cases that do not involve blunt or penetrating trauma as a precipitating factor. However, a history of trivial or minor injury is elicited frequently from patients with so-called spontaneous VAD. The diagnosis of traumatic VAD is reserved for those patients with a history of significant trauma, including motor vehicle accidents (MVAs), falls, or penetrating injuries. Despite the severity of the injury mechanism, dissections of the vertebral artery are exceedingly rare in these contexts.
Several risk factors have been associated with the development of VAD. These include the following:
-
Spinal manipulation [6, 15, 16, 19, 20, 21, 22] : Has one of the best studied and strongest demonstrated associations with VAD (The Canadian Chiropractic Association, Canadian Federation of Chiropractic Regulatory Boards, Clinical Practice Guidelines Development Initiative, Guidelines Development Committee have specific recommendations on assessment of signs of impaired vertebral artery flow and recommendations for treating or not treating patients with suspected impaired flow. [23] )
-
Vertebral artery hypoplasia [24]
-
Yoga
-
Ceiling painting
-
Nose blowing
-
Minor neck trauma
-
Judo
-
Medical risk factors
-
Hypertension [25] (48% in one series)
-
Oral contraceptive use
-
Intrinsic vascular pathology
-
Cystic medial necrosis
-
Female sex
-
Postpartum (rare) [26]
-
Recent infection [12]
When patients with serious cervical trauma, such as cord injuries or cervical spine fractures, are screened for vertebral artery injury, 20-40% may demonstrate traumatic occlusion. This traumatic vertebral artery occlusion (as opposed to dissection) is asymptomatic, and its management is controversial.
Epidemiology
United States statistics
Dissections of the extracranial cervical arteries are relatively rare. The combined incidence of both verterbral artery dissection (VAD) and carotid artery dissection (CAD) is estimated to be 2.6 per 100,000. However, cervical dissections are the underlying etiology in as many as 20% of the ischemic strokes presenting in younger patients aged 30-45 years. Among all extracranial cervical artery dissections, CAD is 3-5 times more common than VAD. [1]
Sex- and age-related demographics
The female-to-male ratio is 3:1.
In contrast to atherothrombotic disease of the vertebrobasilar circulation, VAD occurs in a much younger population. The average age is 40 years; the average age of a patient with CAD is closer to 47 years. [9]
Prognosis
Extracranial dissection
Most patients with extracranial dissection do remarkably well if they survive the initial crisis. As many as 88% of these patients demonstrate a complete clinical recovery at follow-up. However, this suggests an overall risk of death, recurrent transient ischemic attacks, or stroke of approximately 10%.
One series suggests that the severity of neurologic deficits at the time of presentation is related directly to the functional outcome.
Follow-up angiography demonstrates spontaneous healing in as many as two thirds of these patients.
Intracranial dissection
Patients with intracranial vertebrobasilar dissection constitute a more severely affected subgroup of all patients with verterbral artery dissection (VAD). [13]
The presentation of a dissection involving the intracranial portion of the vertebral artery (segment IV) is characterized by rapidly progressive neurologic deficits, including depressed consciousness.
VAD is associated with subarachnoid hemorrhage, brainstem infarctions, and high mortality rate. [13]
Morbidity/mortality
VAD has been associated with a 10% mortality rate in the acute phase. Death is the result of extensive intracranial dissection, brainstem infarction, or subarachnoid hemorrhage. [6]
Those who survive the initial crisis do remarkably well, with long-term sequelae rare.
Complications
Complications include the following:
-
Brainstem infarction
-
Cerebellar infarction
-
Subarachnoid hemorrhage
-
Vertebral artery pseudoaneurysm causing compressive cranial neuropathy
Major complications of vertebral artery dissection include stroke and death. Previous observational studies have yielded stroke rates between 0.3% and 8.5% after vertebral or carotid artery dissection. However, one randomized clinical trial observed a much lower stroke rate of 1.2% at 3 month follow-up and no deaths were reported in this time. [27, 28] As recurrences are rare, any definitive study examining complications following dissection will require large sample sizes.
-
A, Dissection of the left vertebral artery secondary to guidewire injury. B, Complete resolution occurred in 6 months with only aspirin and clopidogrel (Plavix) therapy.
-
Gunshot wound to the right side of the neck. A, The angiogram shows transections of the right vertebral artery (RVA) and the right internal maxillary artery (RIMAX), with partial transection and pseudoaneurysm formation of the midcervical right internal carotid artery (RICA). The transected segments of the RVA and RIMAX were embolized with coils. B and C, The RICA pseudoaneurysm was successfully treated with a 7 x 40-mm covered stent (Wallgraft).









