Overview
Epistaxis is defined as acute hemorrhage from the nostril, nasal cavity, or nasopharynx. It is a frequent emergency department (ED) complaint and often causes significant anxiety in patients and clinicians. However, the vast majority of patients who present to the ED with epistaxis (likely more than 90%) may be successfully treated by an emergency physician. [1]
Also see Epistaxis, Anterior Nasal Packing for Epistaxis, and Posterior Epistaxis Nasal Pack.
Clinical Presentation
Patient history
Controlling significant bleeding or hemodynamic instability should take precedence over obtaining a lengthy history.
Note the duration, severity of the hemorrhage, and the side of initial bleeding. Inquire about previous epistaxis, hypertension, hepatic or other systemic disease, family history, easy bruising, or prolonged bleeding after minor surgical procedures. Recurrent episodes of epistaxis, even if self-limited, should raise suspicion for significant nasal pathology. [2]
Use of medications, especially aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), warfarin, heparin, ticlopidine, and dipyridamole should be documented, as these not only predispose to epistaxis but make treatment more difficult.
Physical examination
Perform a thorough and methodical examination of the nasal cavity. Blowing the nose decreases the effects of local fibrinolysis and removes clots, permitting a better examination. Application of a vasoconstrictor before the examination may reduce hemorrhage and help to pinpoint the precise bleeding site. Topical application of a local anesthetic reduces pain associated with the examination and nasal packing.
Gently insert a nasal speculum and spread the naris vertically. This permits visualization of most anterior bleeding sources. Approximately 90% of nosebleeds can be visualized in the anterior portion of the nasal cavity. Massive epistaxis may be confused with hemoptysis or hematemesis. Blood dripping from the posterior nasopharynx confirms a nasal source.
A posterior bleeding source is suggested by failure to visualize an anterior source, by hemorrhage from both nares, and by visualization of blood draining in the posterior pharynx.
Differential Diagnosis
The differential diagnosis includes the following:
Diagnostic Considerations
Other problems to be considered include the following:
-
Chemical irritants
-
Hepatic failure
-
Leukemia
-
Thrombocytopenia
-
Heparin toxicity
-
Ticlopidine toxicity
-
Dipyridamole toxicity
-
Trauma
-
Tumor
A study by Szyszkowicz et al suggested that an association exists between air pollution exposure and ED visits for epistaxis. The report indicated that the number of such ED visits rises with increases in the interquartile range for the concentration of ozone and PM-10 (particles with a diameter of up to 10 micrometers). [3]
A prospective study on the influence of meteorologic factors on nosebleeds indicated that air temperature affects epistaxis rates, although the report, which involved 310 patients, did not find the incidence to be linked to air pressure, rainfall, humidity, wind speed, or duration of sunlight. [4]
Treatment & Management
Initial measures
Gowns, gloves, and protective eyewear should be worn. Adequate light is best provided by a headlamp with an adjustable narrow beam. Patients should be positioned comfortably in a seated position, holding a basin under their chin.
As always, first address the ABCs (A irway, B reathing, and C irculation). Rarely, severe epistaxis may necessitate endotracheal intubation.
Stable patients should be instructed to grasp and pinch their entire nose, maintaining continuous pressure for at least 10 minutes. Make sure that they compress the soft nose tissues against the nasal septum; pinching the hard, incompressible nasal bones will not aid hemorrhage control.
Patients with significant hemorrhage should receive an intravenous (IV) line and crystalloid infusion, as well as continuous cardiac monitoring and pulse oximetry. Patients frequently present with an elevated blood pressure; however, a significant reduction can usually be obtained with analgesia and mild sedation alone.
Specific antihypertensive therapy is rarely required and should be avoided in the setting of significant hemorrhage. The relation between hypertension and epistaxis is often misunderstood. [5, 6, 7] Patients with epistaxis commonly present with an elevated blood pressure. Epistaxis is more common in hypertensive patients, perhaps owing to vascular fragility from long-standing disease.
Hypertension, however, is rarely a direct cause of epistaxis. More commonly, epistaxis and the associated anxiety cause an acute elevation of blood pressure. Therapy, therefore, should be focused on controlling hemorrhage and reducing anxiety as primary means of blood pressure reduction.
Insert pledgets soaked with an anesthetic-vasoconstrictor solution into the nasal cavity to anesthetize and shrink nasal mucosa. Soak pledgets in 4% topical cocaine solution or a solution of 4% lidocaine and topical epinephrine (1:10,000) and place them into the nasal cavity. Allow them to remain in place for 10-15 minutes.
If a bleeding point is easily identified, gentle chemical cauterization may be performed after the application of adequate topical anesthesia. The tip of a silver nitrate stick is rolled over mucosa until a gray eschar forms. To prevent septal necrosis or perforation, only 1 side of the septum should be cauterized at a time. To be effective, cauterization should be performed after bleeding is controlled. Thermal cauterization using an electrocautery device is reserved for more aggressive bleeding and is done with the patient under local or general anesthesia. [8]
If attempts to control hemorrhage with pressure or cauterization fail, the nose should be packed. Options include traditional nasal packing, a prefabricated nasal sponge, an epistaxis balloon, or absorbable materials. [9, 10, 11, 12, 13, 14, 15]
A literature review by Kamhieh and Fox suggested that tranexamic acid is an effective treatment for epistaxis. Although one trial reported that topical tranexamic acid is not of significant benefit in acute epistaxis, the largest trials did indicate significant efficacy. One study also reported that oral tranexamic acid was not effective in acute epistaxis, but two randomized, controlled trials found it to reduce severity and frequency of recurrent epistaxis in patients with hereditary hemorrhagic telangiectasia. [16]
Another literature review, by Gottlieb et al, also indicated that topical tranexamic acid is effective against acute epistaxis. While the rate of bleeding cessation within 30 minutes did not differ significantly between the tranexamic acid group and controls, more patients treated with the agent were discharged within 2 hours of arrival. Moreover, at 24-hour and 1-week follow-up, there were fewer rebleeding episodes with tranexamic acid. The complication rate associated with tranexamic acid did not differ from that for controls. [17]
In contrast to the Gottlieb study, a retrospective report by Birmingham et al found no significant difference in emergency department length of stay between patients with acute epistaxis who were treated with topical tranexamic acid and those who received standard care. However, the rates of otolaryngologist consults and nasal packing were significantly lower in the tranexamic acid group than in the standard care patients (30.0% vs 65.2% and 16.7% vs 23.9%, respectively). [18]
Traditional (petrolatum gauze) packing
Traditional anterior nasal packing with petrolatum gauze has largely been supplanted by the use of tampons and balloons, which are readily available and more easily placed. This method is commonly performed incorrectly, using an insufficient amount of packing placed primarily in the anterior naris. When placed in this way, the gauze serves as a plug rather than as a hemostatic pack. Physicians inexperienced in the proper placement of a gauze pack should use a nasal tampon or balloon instead.
The proper technique for placement of a gauze pack is as follows. Grasp the gauze ribbon about 6 inches from its end with a bayonet forceps. Place it in the nasal cavity as far back as possible, ensuring that the free end protrudes from the nose. On the first pass, the gauze is pressed onto the floor of nasopharynx with closed bayonets.
Next, grasp the ribbon about 4-5 inches from the nasal alae, and reposition the nasal speculum so that the lower blade holds the ribbon against lower border of the nasal alae. Bring a second strip into the nose, and press downward.
Continue this process, layering the gauze from inferior to superior until the naris is completely packed. Both ends of ribbon must protrude from the naris and should be secured with tape. If this measure does not stop the bleeding, consider bilateral nasal packing.
Packing with compressed sponge
Trim the compressed sponge (eg Merocel) to fit snugly through the naris. Moisten the tip with surgical lubricant or topical antibiotic ointment. Firmly grasp the length of the sponge with a bayonet forceps, spread the naris vertically with a nasal speculum, and advance the sponge along the floor of the nasal cavity. Once wet with blood or a small amount of saline, the sponge expands to fill the nasal cavity and tamponade bleeding (see the images below).
Packing with epistaxis balloons
Anterior epistaxis balloons (eg, Rapid Rhino) are available in different lengths (see the images below). A carboxycellulose outer layer promotes platelet aggregation. The balloons are as efficacious as nasal tampons, easier to insert and remove, and more comfortable for the patient. To insert the balloon, soak its knit outer layer with water, insert it along the floor of the nasal cavity, and inflate it slowly with air until the bleeding stops.
Posterior epistaxis is frequently treated with double-balloon devices that have separate anterior and posterior balloons.
After passing the posterior balloon through the naris and into the posterior nasal cavity, inflate it with 4-5 mL of sterile water, and gently pull it forward to fit snugly in the posterior choana. After bleeding into the posterior pharynx has been controlled, fill the anterior balloon with sterile water until the bleeding completely stops. Avoid overinflation, because pressure necrosis or damage to the septum may result. Record the amount of fluid placed in each balloon.
If a Foley catheter is used, place a 12-16 French catheter with a 30-mL balloon into the nose along the floor of the nasopharynx, until the tip is visible in the posterior pharynx. Slowly inflate the balloon with 15 mL of sterile water, pull it anteriorly until it is firmly seated against the posterior choanae, and secure it in place with an umbilical clamp. Use a buttress clamp with cotton gauze to avoid pressure necrosis on the nasal alae or columella. Finally, place an anterior nasal pack.
Also see Anterior Epistaxis Nasal Pack and Posterior Epistaxis Nasal Pack.
Packing with absorbable materials
Absorbable materials such as oxidized cellulose (Surgicel), gelatin foam (Gelfoam), and gelatin and thrombin combination (FloSeal) are suitable alternatives to nasal packing for anterior bleeds. [19] They directly tamponade bleeding sites, increase clot formation, and protect the nasal mucosa from desiccation or further trauma. They are easy to use and comfortable and conform to the irregularity of the nasal contours. [20, 21]
Consultations
Attempts at nasal packing may result in significant slowing but not cessation of hemorrhage. Failure to completely control hemorrhage is an absolute indication for consultation with an otolaryngologist in the emergency department (ED).
Epistaxis that requires posterior packing should be managed in cooperation with an otolaryngologist. Because of multiple possible complications, admission is required, usually in a monitored setting.
Consultation with a hematologist is indicated for patients with bleeding dyscrasias or coagulopathies.
Antibiotics
In a survey of physician members of the American Rhinologic Society (307 responses), Mallen et al found that in patients with epistaxis who are treated with packing, 20.0% of respondents prescribe antibiotics when dissolvable packing is used, while 84.2-84.6% prescribe antibiotics when non-dissolvable packing is employed. The risk of toxic shock syndrome was cited as a rationale for antibiotic prescription by 85.6% of the physicians. According to the investigators, evidence is limited regarding the benefit of prophylactic antibiotic use in patients with epistaxis who undergo nasal packing. [22]
Further inpatient care
Admit patients with posterior packing. Posterior nasal packing is particularly uncomfortable for the patient and promotes hypoxia and hypoventilation. Failure to admit and appropriately monitor all patients who require posterior packing may result in significant mortality.
Elderly patients or patients with cardiac disorders or chronic obstructive pulmonary disease (COPD) should receive supplemental oxygen and be admitted to a monitored setting.
Significant or uncontrolled bleeding from a posterior site may require operative management; this occurs in about 30% of cases. Interventional radiology embolization of involved arteries and surgical ligation of vessels are possible options in such instances. [21, 23, 24]
Further outpatient care
Patients discharged from the hospital with anterior packing should receive follow-up care with an otolaryngologist within 48-72 h. Nasal packing prevents drainage of sinuses and increases the risk of sinusitis or toxic shock syndrome.
Tumors or other serious pathology are infrequent causes of epistaxis. However, all patients who present with epistaxis should have follow-up care arranged with an otolaryngologist for a complete nasopharyngeal examination. Recurrent unilateral epistaxis should particularly raise concern for neoplasm. [8]
Consider placing patients on a broad-spectrum antibiotic (eg, a penicillin or first-generation cephalosporin) to cover all likely pathogens in the context of the clinical setting.
Oral analgesics should also be prescribed. Pain control is essential to quality patient care: it ensures patient comfort, promotes pulmonary toilet, and enables physical therapy regimens. Most analgesics have sedating properties, which are beneficial for patients who have painful skin lesions. Advise patients to avoid aspirin, aspirin-containing products, and nonsteroidal anti-inflammatory drugs (NSAIDs).
Patients who take warfarin may generally continue their current regimen unchanged. Temporary discontinuation of warfarin or active reversal of coagulopathy is indicated only in cases of uncontrolled hemorrhage and a supratherapeutic international normalized ratio (INR).
COVID-19 guidelines
In May 2020, D’Aguanno et al published the following clinical recommendations for addressing epistaxis during the coronavirus disease 2019 (COVID-19) pandemic [25] :
-
Strict recommendation for disposable equipment use
-
Preference for FFP3 (Europe) or N99 (United States) mask use
-
Use of FFP2 or N95 masks, covered by a surgical mask, if FFP3 masks are not available
-
Strong recommendation for cap and shoe covers, goggles, gown, and double nitrile gloves
-
Control of nosebleed risk factors (blood pressure, coagulation factors, ongoing therapies with antithrombotic or anticoagulant agents)
-
Checks should be made for fever, respiratory symptoms, and at-risk contacts
-
Investigate sudden loss of smell and/or taste
-
Surgical mask for patients, if permissible
-
Immediate assessment of nosebleed severity
-
Noninvasive intervention is recommended, including bidigital compression and use of antifibrinolytic agents
-
If conventional operating rooms are unavailable, use well-demarcated spaces within the emergency department
-
Use of a reduced and experienced clinical staff, including a surgeon and a scrub nurse, with proper personal protective equipment (PPE)
-
Avoid unnecessary intervention
-
Perform nasal packing or cautery in case of noninvasive procedure failure
-
Use of resorbable packing, if available
-
Postponement of surgery for posterior epistaxis requiring sphenopalatine artery ligation, until COVID-19 testing is performed
-
Avoid local anesthetic atomized sprays; soaked pledgets are preferred
-
During the procedure, use a suction system, employing a closed system with a viral filter
-
Patient should receive postprocedural instructions with regard to packing removal or antibiotic prophylaxis, in order to lower recurrence risk and optimize outcome
-
Careful execution of gowning and degowning procedures should be employed
-
Use of standard PPE by personnel who handle surgical equipment decontamination
Patient Education
Give patients specific written follow-up instructions. For rebleeding or future nosebleeds, patients should be instructed to firmly pinch their entire nose for 10-15 minutes. Ice packs do not help. [26]
Encourage nasal hydration with topical gels, lotions, or ointments to moisturize mucosa and promote healing of friable areas. Humidifiers or vaporizers in bedrooms may increase ambient humidity. [27, 20]
-
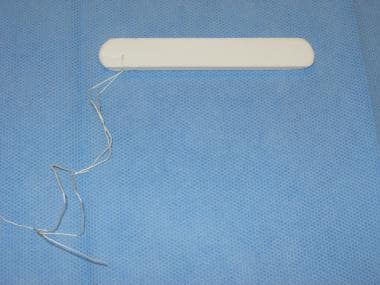
Compressed sponge - Merocel.
-
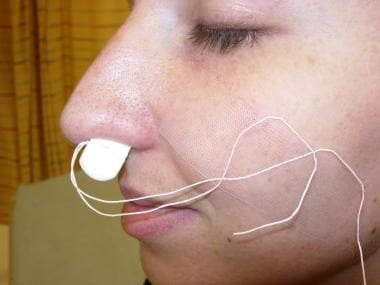
Merocel placed in left nostril for anterior packing.
-
Rapid Rhino - 5.5 cm for anterior nasal packing.
-
Rapid Rhino bilateral - 7.5 cm for anterior/posterior nasal packing.