Background
Since the earliest days of the study of medicine and the human body, anatomists and pathologists have been intrigued by the mysterious, gelatinous substance filling a majority of the volume of the eye. The vitreous body comprises four fifths of the globe, averaging 4 mL in an adult. Vitreous is 99% water, with collagen and hyaluronic acid comprising the remaining 1%. These components give vitreous its specific gel-like form.
Emergency physicians are rarely called upon to diagnose and treat diseases of the vitreous, but sometimes their timely diagnosis and referral to a specialist can be vision saving. Frequently, even the suspicion of abnormalities within the vitreous mandates referral to an eye surgeon with special training in the diagnosis and treatment of vitreoretinal disease of the eye.
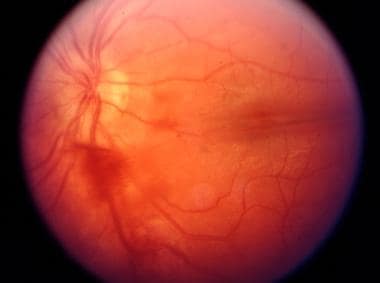
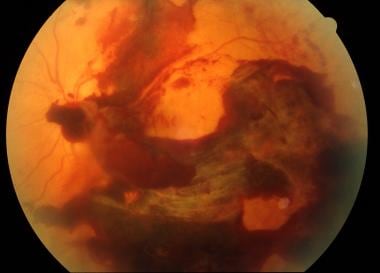
One such ophthalmologic emergency presenting to an emergency room is a vitreous hemorrhage, as shown in the images below. Vitreous hemorrhage is defined as the presence of extravasated blood within the space outlined by the zonular fibers and posterior lens capsule anteriorly, the nonpigmented epithelium of the ciliary body laterally, and the internal limiting membrane of the retina (lamina limitans interna) posteriorly and posterolaterally. Because distinguishing blood actually within the vitreous from bleeding between the internal limiting membrane and the retina's nerve fiber layer (called a subinternal limiting membrane hemorrhage) and from preretinal hemorrhages (those between the internal limiting membrane and the vitreous) is not always possible by the ED physician, these conditions are all considered types of vitreous hemorrhage.
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
Pathophysiology
The vitreous is a clear, gelatinous, and avascular substance, filling the space bound by the lens, ciliary body, retina, and optic disc. A layer of cells, termed the internal limiting membrane, lines the inner surface of the retina, separating it from the vitreous and forming one side of a potential space between it and the vitreous (ie, subhyaloid space).
Since healthy vitreous is relatively inelastic and impervious to cells and debris, it plays an essential role in maintaining the transparency and form of the eye. If the vitreous is removed surgically and replaced with saline (as occurs with some forms of vitreous surgery), cellular matter and debris may more freely migrate into the optical pathway than if there is only natural vitreous.
Since the vitreous is avascular, a vitreous hemorrhage describes the invasion of blood into a bloodless gel.
The vitreous is attached firmly to other portions of the inner eye at two important areas e. First, A 4-millimeter-wide circumferential portion of the vitreous, termed the vitreous base. located at the anterior termination of the retina (ie, ora serrata),is firmly attached to the underlying retina and pars plana. This maintains its strength throughout life. Any pulling forces (traction) on the vitreous are transmitted to the adjacent peripheral retina at the vitreous base.
The second attachment is at the posterior portion of the globe at the margin of the optic nerve, where the vitreous is attached in a circle of approximately 2 mm in diameter. During the aging process, the vitreous normally liquefies and shrinks. This shrinkage commonly reaches a certain stage at which this attachment of the vitreous gives way and the vitreous detaches from its posterior attachment at the margin of the optic nerve. This is called a posterior vitreous detachment (PVD) or posterior vitreous separation. The prior attachment of the vitreous to the optic nerve head can often be seen as a feathery ring (ie, Weiss ring) following PVD. A PVD is present in approximately 50% of people at age 60 years.
The vast majority of PVDs are spontaneous and are unassociated with vitreous hemorrhage. However, tractional forces at either of these attachments may result in hemorrhage from retinal blood vessels underneath the vitreous. If bleeding has occurred in the subhyaloid space, it appears boat shaped on the surface of the retina, forming a superior straight line in an upright patient but changing with the position of the patient. Blood within the space between the internal limiting membrane and the nerve fiber layer is under tension and does not shift with the position of the patient's head. In contrast, blood in the vitreous body shows no characteristic borders, variable mixing with the vitreous, somewhat dependent on the degree of prior liquefaction of the vitreous, may clot in parts, and clears slowly, at about 1% per day.
One of the earliest clinical descriptions of vitreous hemorrhage was authored by the German ophthalmologist Litten in 1881 in persons with subarachnoid hemorrhage (SAH). [1] This uncommon but interesting mechanism of vitreous hemorrhage is called Terson syndrome, named after the French ophthalmologist who described it 19 years later; vitreous hemorrhage occurs as a result of abrupt intracranial (ie, subarachnoid) bleeding with anterior dissection of blood under the arachnoid coat of the optic nerve into the eye.
Between 10 and 40% of all patients with SAH have an associated vitreous hemorrhage, which is termed Terson syndrome. If Terson syndrome is bilateral, its presence represents a poor prognostic indicator of SAH. Some studies have suggested that compared with patients with SAH alone, patients with both subarachnoid and vitreous bleeding are 4.8 times more likely to die. [2]
Epidemiology
Frequency
United States
The prevalence of vitreous hemorrhage corresponds to the frequency of the underlying disease processes with which it is associated. In the United States, the population-based incidence of spontaneous vitreous hemorrhage is approximately 7 cases per 100,000 persons per year.
The most common causes of vitreous hemorrhage are proliferative diabetic retinopathy, vitreoretinal traction with retinal tears, PVD with or without retinal tears, severe choroidal neovascularization with breakthrough bleeding into the vitreous, and ocular trauma (eg, shaken baby syndrome, postsurgical eyes, automobile injuries, direct trauma to the eye). Together, these account for the majority of all cases. Less common causes include branch or central retinal vein occlusion, sickle cell retinopathy, age-related macular degeneration, intraocular tumors, retinopathy of prematurity, the leukemias, acute retinal necrosis, HIV-related retinopathy, and some types of uveitis. Retinal neovascularization of any cause can result in vitreous hemorrhage.
Race
Race, sex, and age of the patient presenting with vitreous hemorrhage correspond to the incidence of the underlying disease. Examples include aneurysmal SAH among women, diabetes and sickle cell disease among black individuals, macular degeneration among elderly white individuals (which can lead to subretinal/choroidal neovascularization and breakthrough bleeding into the vitreous), and individuals with high myopia, more common in Asian populations, who have an increased risk of retinal tears, detachment, and associated vitreous hemorrhage.
-
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
-
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
-
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
-
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
-
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
-
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.
-
Vitreous hemorrhage. Courtesy of UT Southwestern Medical School, Department of Ophthalmology.