Background
Periorbital infections consist of a group of infections that can be broadly classified into 2 distinct groups. One group consists of infections of the dermis and associated tissues around the eyes. The other group consists of infections of the lacrimal system.
Periorbital cellulitis
Infections of the superficial skin around the eyes are called periorbital, or preseptal cellulitis. These infections are limited to the area anterior to the orbital septum. Periorbital cellulitis is predominantly, although not exclusively, a pediatric disease. [1, 2]
 Periorbital cellulitis. This image shows an 8-year-old patient who presented with unilateral eyelid swelling and erythema.
Periorbital cellulitis. This image shows an 8-year-old patient who presented with unilateral eyelid swelling and erythema.
Periorbital cellulitis represents the first of the 5 nonprogressive types of orbital infections. These are classified as follows [3] :
-
Group 1 - Preseptal cellulitis
-
Group 2 - Orbital cellulitis
-
Group 3 - Subperiosteal abscess
-
Group 4 - Orbital abscess
-
Group 5 - Cavernous sinus thrombosis
Lacrimal system infections
Infections of the lacrimal system are classified based on the location of the infection; they include the following:
-
Blepharitis - Inflammation of the lid margins; anterior blepharitis affects the area of the lid where the eyelashes attach; posterior blepharitis affects the inner portion of the eyelid margin that is in contact with the eye; blepharitis primarily affects older persons (mean age 40-50 years) [4]
-
Canaliculitis – Inflammation of the canaliculi
-
Dacryoadenitis - Inflammation of the lacrimal gland
-
Dacryocystitis - Inflammation of the lacrimal duct or sac; obstructed lacrimal ducts causing dacryocystitis are common in infants and usually resolve by age 9-12 months [5]
Patient education
For patient education information, see Cellulitis. A blepharitis fact sheet is available for purchase from the American Academy of Ophthalmology. [6]
Anatomy
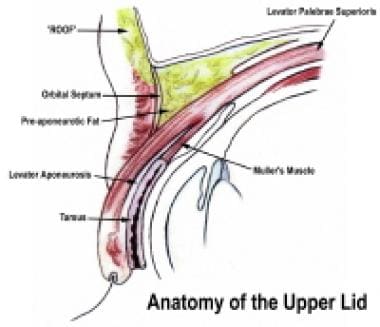
Orbital septum
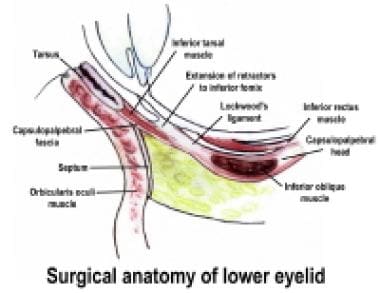
The orbital septum is a fibrous membrane that extends from the periosteum of the orbit as the arcus marginalis and lies just deep to the orbicularis oculi muscle.
In the upper lids, the septum fuses with the levator aponeurosis. In the lower lids, the septum fuses with the capsulopalpebral fascia. [7] The orbital septum acts as a physical barrier to the spread of infection.
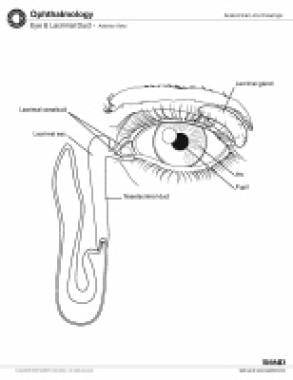
Lacrimal system
The lacrimal system includes the structures involved in the production and drainage of tears. The lacrimal gland is located in the lateral upper lid margin. It produces about 10 mL of secretions per day.
In the process of blinking, the eyes close from the lateral edge to the medial edge, pushing the tear film across the surface of the eye. Most of the tear volume is lost through evaporation. A small portion is drained from the lacrimal lake, located at the inner canthus, through the puncta and into the superior and inferior canaliculi. Tears then flow into the common canaliculus and lacrimal sac.
The lacrimal duct, which lies within the bone, connects the lacrimal sac with the eventual site of egress, the inferior meatus of the nose. [7]
Etiology
Periorbital cellulitis
Data regarding the causes of preorbital cellulitsi is limited. Periorbital cellulitis can occur by several mechanisms, including the following [2, 8] :
-
Infection as a result of local trauma, including insect bites
-
Infection as a result of spread from contiguous structures, as in conjunctivitis, hordeolum, lacrimal system infections, and impetigo
-
Infections secondary to hematogenous spread during bacteremia due to nasopharyngeal pathogens
-
Infection secondary to sinusitis, causing venous and lymphatic congestion - Sinusitis may be of odontogenic origin [9] ; thorough examination of dentition may be warranted
Infectious organisms
When associated with trauma, periorbital cellulitis can be caused by the following bacterial species:
-
Staphylococcus aureus - This may include methicillin-resistant S aureus [10] ; treatment should be tailored to local incidence of infection
-
Streptococcus pyogenes (group A streptococci)
In the absence of trauma, periorbital cellulitis can be caused by the following microbes:
-
Streptococcus pneumoniae
Other unusual causes of periorbital cellulitis include the following:
-
Neisseria gonorrhoeae [14]
-
Herpes simplex virus
-
Mycobacterium tuberculosis [19]
-
Bacillus anthracis [20]
-
Taenia solium – Periorbital cellulitis can develop secondary to orbital cysticercosis caused by this organism [21]
Blepharitis
Anterior blepharitis is usually secondary to infection or seborrheic in nature, or else it is a combination of both. If the pilosebaceous glands of Zeiss and Moll become infected, an abscess may occur. This abscess is known as an external hordeolum, or stye. [22] Cell-mediated immunologic mechanisms have been implicated in the development of chronic blepharitis. [23, 24]
Posterior blepharitis is caused by Meibomian gland dysfunction. The Meibomian gland secretes the oily layer of the tear film. This oily layer is responsible for preventing excessive evaporation of the aqueous layer of the tear film. If the secretions become inspissated, causing plugging of the gland, a chalazion may develop. A chalazion is a noninfectious, granulomatous reaction. If there is infection secondary to plugging, an internal hordeolum develops. [25]
The use of eye makeup, especially eyeliner, can cause acute exacerbations of blepharitis by plugging the glands. [26]
Anterior blepharitis
Causative organisms in anterior blepharitis include the following:
-
Infectious etiology usually due to Staphylococcus species [22]
-
Helicobacter pylori - Associated with blepharitis, but cause and effect have not been established [28]
-
Viruses - Herpes simplex virus, herpes zoster virus, and human papillomavirus
-
Mites -Demodex folliculorum and Demodex brevis [29]
-
Lice -Phthirus pubis, which causes a condition known as phthiriasis palpebrarum [30]
-
Noninfectious entities such as ocular rosacea and seborrheic dermatitis also cause anterior blepharitis
Posterior blepharitis
Etiologic characteristics of posterior blepharitis include the following:
-
Meibomian gland dysfunction leading to increased evaporation of the protective tear layer [31]
-
Most frequently associated with rosacea
-
Pityrosporum fungal infection is associated with Meibomian gland dysfunction [32]
Dacryoadenitis
Dacryoadenitis is caused by local infection of the lacrimal gland by bacteria or viruses. Chronic dacryoadenitis associated with inflammation and swelling of the salivary glands of unknown origin is called Mikulicz disease. When associated with other entities such as tuberculosis, sarcoidosis, or lymphoma, it is termed Mikulicz syndrome. This was previously considered a subtype of Sjögren syndrome, although now differences between the 2 entities have been determined. [33]
Bacteria
Dacryoadenitis is most often caused by gram-positive cocci, usually staphylococci. It may also be caused by S pneumoniae.
Viruses
Prior to increased immunization rates, the mumps virus was most often implicated in the development of dacryoadenitis. Now, the Epstein-Barr virus is most often associated with chronic dacryoadenitis. [34]
Dacryocystitis
Dacryocystitis is caused by inflammation of the lacrimal sac; this usually occurs in the setting of obstruction of the lacrimal apparatus. The obstruction may be congenital or secondary to infection, tumor, or trauma. [7]
Infectious causes include gram-positive isolates (Staphylococcus and Streptococcus species), in 71-78% of cases, and gram-negative isolates, in 22-29% of cases. [35, 36] Rarely, dacryocystitis may result from mucormycosis. [37]
Canaliculitis
Canaliculitis is caused by infection of the canaliculi; often, it is chronic. The disorder may also be iatrogenic, occurring after the use of instrumentation or the placement of silicone plugs in the treatment of dry eyes. [38]
It is classically taught that the most common pathogens of canaliculitis are Actinomyces israelii and Nocardia (formerly known as Streptothrix) species. [5, 39]
Case reviews, however, have shown mixed flora associated with infection. Species isolated include Staphylococcus species, Escherichia coli, Haemophilus species, Pseudomonas aeruginosa, Klebsiella oxytocia, [40] Arcanobacterium (previously Corynebacterium) haemolyticum, [41] and M chelonae. [42]
Prognosis
Prognoses in periorbital infections are as follows:
-
Periorbital cellulitis - With appropriate antibiotics, the prognosis is good
-
Blepharitis - Typically, this is a chronic disease with waxing and waning of symptoms
-
Dacryoadenitis - Prognosis of the acute form is excellent, as it is a self-limiting process; prognosis of the chronic form depends on the underlying disease process
-
Dacryocystitis - Success rates for dacryocystorhinostomy are good; external procedures fare better due to the ability to create a larger ostium.
-
Canaliculitis - Prognosis is excellent with definitive treatment by canaliculotomy with curettage.
Complications
Periorbital cellulitis
Complications of periorbital cellulitis include the following:
-
Recurrent periorbital cellulitis (RPOC) - Three periorbital infections occurring within 1 year, spaced by at least 1 month of convalescence [43]
-
Toxic shock syndrome
-
Eschar formation leading to scarring
-
Meningitis
-
Orbital cellulitis
-
Intracranial extension of infection
-
Periorbital necrotizing fasciitis - A potential complication with devastating results; the mortality rate is reported to be 14.4% [44]
Blepharitis
Complications of blepharitis include the following:
-
Hordeolum
-
Chalazion
-
Scarring of the cornea, which could lead to blindness
-
Trichiasis (misdirection of eyelashes)
-
Corneal infection
-
Endophthalmitis - Patients with blepharitis undergoing intraocular surgery may have an increased risk of developing this condition
Dacryocystitis
Dacryocystitis may be associated with periorbital cellulitis. Rarely, it may be associated with orbital cellulitis or abscess formation. This is usually prevented by the orbital septum, which surrounds the lacrimal sac. [45]
Complications may occur during a dacryocystorhinostomy, including hemorrhage, infection, and cerebrospinal fluid (CSF) leakage.
Canaliculitis
Epiphora may result from failure of tear film to appropriately drain through the lacrimal system.
Pathophysiology
S aureus, Staphylococcus epidermidis, and S pyogenes account for approximately 75% of pediatrics periorbital infections. Staphylococcus and Streptococcus are the most two common pathogens responsible for pediatric orbital cellulitis. [46]
Epidemiology
Periorbital cellulitis is primarily a pediatric disease, occurring mostly in children younger than 5 years. Periorbital cellulitis is almost three times more common than orbital cellulitis.
While orbital cellulitis is more common in the pediatric population, it can affect all age groups. In one retrospective analysis, the average age of affected patients was 6.8 years (ranging from age 1 week to 16 years). [47] Worldwide, orbital cellulitis occurs more often in winter. It is associated with upper respiratory tract infections, and most cases have a unilateral presentation. [48, 49]
Periorbital cellulitis has no sexual predilection. Orbital infections have a male-to-female ratio of 2:1.
-
Periorbital cellulitis. This image shows an 8-year-old patient who presented with unilateral eyelid swelling and erythema.
-
Acute dacryocystitis.
-
Upper eyelid anatomy.
-
Lower eyelid anatomy.
-
Eye and lacrimal duct, anterior view.